Impaired motor control after sport-related concussion could increase risk for musculoskeletal injury:Implications for clinical management and rehabilitation
Trs L.Chmilwski*,Justin TtmnShuhi Suzukib,MryBth Horoyski,Dry S.Rismn,Russll M.Bur,Jms R.Clugston,Dnil C.Hrmn
a TRIA Orthopedic Center,Bloomington,MN 55431,USA
b ATP Tour Inc.,Ponte Vedra Beach,FL 32082,USA
c Department of Orthopaedics and Rehabilitation,University of Florida,Gainesville,FL 32607,USA
d Department of Physical Therapy,University of Delaware,Newark,DE 19716,USA
e Department of Clinical and Health Psychology,University of Florida,Gainesville,FL 32611,USA
f Department of Community Health&Family Medicine,University of Florida,Gainesville,FL 32603,USA
Abstract
Keywords: Clinical management;Concussion;Injury;Motor control;Rehabilitation
1. Introduction
Sport-related concussion (SRC) is induced by biomechanical forces to the head that result in a range of transient clinical signs,symptoms, and disturbances in function.1Clinical examination for SRC includes an assessment of patient-reported symptomology and tests of neurologic, cognitive, vestibular, oculomotor,and postural function.1After acute symptoms stabilize, the athlete is allowed to begin a graduated progression of physical activity and cognitive exertion, as long as symptoms are not exacerbated.1,2Multidisciplinary, individualized care is recommended, which may involve treatment or rehabilitation to address persistent clinical impairments in vestibular, cervical,autonomic, and psychological domains.1,3-5Clinical recovery after SRC is judged to be complete when the neurological examination is normal and post-concussion symptoms and the multifactorial assessments of function have returned to baseline status during daily activities including school, work, and sport.1,6Most athletes meet these criteria within 21-30 days post-SRC.7It is recommended that the return to sport participation after SRC follow a stepwise progression where participation in athletic activity without symptom recurrence is evident prior to sport participation at a competitive level.1
Despite advances in SRC clinical management protocols,a growing body of evidence has shown that athletes with SRC have double the odds of sustaining a musculoskeletal injury after they return to sport compared to athletes without SRC.8-13The relationship between SRC and musculoskeletal injury has been consistently observed among studies and in athletes of both sexes and across multiple sports and levels of play.10Furthermore, the increased risk of musculoskeletal injury may persist for months or more past the time of return to sport participation.10Previous reviews have discussed the increased risk of musculoskeletal injury after SRC.10,14-17The phenomenon has been theorized to result from persistent sensorimotor impairments,10decreased neuromechanical responsiveness,16altered perception-action coupling,15or subtle neurocognitive and neuromuscular deficits.14,17From a broader perspective, each of these theories relate to aspects of motor control.Previous reviews have also focused on a singular or narrow aspect of motor function,making it difficult to appreciate the many ways that motor function may change post-SRC.
Our review presents a conceptual framework and supporting evidence that link impaired motor control after SRC to musculoskeletal injury risk. In addition, potential changes in SRC clinical management and rehabilitation to mitigate injury risk are discussed.
2. A brief overview of motor control
Motor control refers to “how the nervous system interacts with the rest of the body and the environment to produce purposeful, coordinated movement” and is often used interchangeably with the term “neuromuscular control” in the rehabilitation literature.18,19Motor control involves the processing of sensory information (e.g., somatosensory, visual,vestibular, and auditory) and coordination of motor output within the central nervous system.The relative weight of each component in producing a given movement varies by situation or task because motor control is context-dependent.18,20
Key aspects of motor control are motor planning and motor learning.21Motor planning refers to the selection of a motor plan,which consists of the movement goals with respect to the muscles and joints.22Motor planning starts with an awareness of sensory cues in the environment and requires appropriate processing of the sensory input in order to select an optimal motor plan.22For movements that occur relatively slowly, the selected motor plan may be shaped by cognitive processing,or decision making, but when there is little time for cognitive processing (e.g., hitting a fastball in baseball), perceptualmotor routines and previously learned action sequences likely provide the basis for the motor plan.23Motor learning refers to the experience-dependent acquisition of a motor skill or adaptation of a motor skill when task conditions change.24Motor learning may be categorized as explicit or implicit. Explicit motor learning occurs with conscious, purposeful cognitive processing, whereas implicit motor learning occurs without conscious awareness of what is being learned and is thought to be a more automatic process.25-27Most motor learning is neither purely explicit nor purely implicit.
The way feedback is given influences whether motor learning is explicit or implicit.Coaching and rehabilitation predominantly encourage explicit motor learning (principally,strategy-based learning) through verbal cues and visual feedback on motor skill performance.28,29Feedback may be directed toward knowledge of results—that is, how well the movement achieved the goal of the performance—or knowledge of performance,which is about the movement characteristics that led to the performance.30Implicit motor learning,and specifically sensorimotor adaptation,occurs in response to sensory prediction errors detected during motor task performance.31-34To illustrate these concepts, if an athlete is told to“bend your knee”during walking,this feedback on motor task performance initially requires cognitive processing and results in primarily explicit motor learning. In contrast, if an elastic band is used to resist knee flexion during gait, this initially results in less knee flexion during gait,causing a sensory error signal.The error signal results in the athlete producing greater knee flexion to overcome the resistance. By practicing this way, implicit learning through sensorimotor adaptation will occur so that when the elastic band is removed,the athlete will continue to produce greater knee flexion during gait.
3. Theoretical link between impaired motor control and musculoskeletal injury risk
Sport participation is inherently a series of motor tasks performed in a rapidly changing environment with additional cognitive demands, such as recalling plays. If an athlete cannot accurately perceive and process sensory cues in the athletic environment while simultaneously performing cognitive tasks related to the sport,motor plan selection,and thus motor function, could be negatively affected. It is conceivable that this could make the athlete vulnerable to musculoskeletal injury.
Preliminary studies in athletic populations support the proposition that impaired motor control is associated with musculoskeletal injury risk.Athletes with low perceptual and cognitive aptitude in domains such as reaction time, processing speed,and visual and verbal memory have increased risk for non-contact anterior cruciate ligament rupture and other lower extremity injuries.35-37Additionally, athletes with a low aptitude in visual processing and memory domains demonstrate movement patterns during jump landing that are associated with a higher risk of knee injury.38,39It is important to point out that mean neurocognitive test scores fall within acceptable limits in groups that sustain injury or demonstrate altered movement patterns. Furthermore, neurocognitive scores associated with elevated injury risk are not well-defined for athlete populations that vary by sport or other demographics. Despite this limitation, a consistent finding in the current literature is that reaction time scores on the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) of greater than 545-570 ms is associated with increased lower extremity injury risk in collegiate athletes.35-37These data suggest that reaction time and speed of processing in completing cognitive tasks may be useful in evaluating athletes for elevated injury risk.
Research in the SRC population also supports the proposition that impaired motor control could increase the risk for musculoskeletal injury.14For example,athletes with SRC who sustained a time-loss injury within 1 year demonstrated greater decrements in a gait speed differential(gait performed with or without an additional cognitive task) at testing between 21 days post-concussion and clearance for sport participation.40In addition, athletes with SRC who sustained a lower extremity musculoskeletal injury within 1 year demonstrated at preseason testing and clearance for sport participation a slower speed and greater time in double-limb support during gait performance with or without a simultaneous cognitive task.41Current research has not shown that athlete demographics and neurocognitive test scores at baseline or acutely following SRC are indicators of whether athletes are at risk of sustaining a musculoskeletal injury following SRC.42
Current SRC clinical management attempts to normalize post-concussion impairments through return to sport criteria that cover a variety of functional domains.1At this time,motor control is neither explicitly assessed nor targeted in interventions.6,17However,the literature cited in the following sections provides evidence for the persistence of subtle changes in the central nervous system relevant to motor control and altered motor function even after return to sport criteria are fulfilled.Thus, we propose that impaired motor control after SRC, evidenced by neurobiological and motor function changes, leads to an increased risk for musculoskeletal injury(Fig.1).
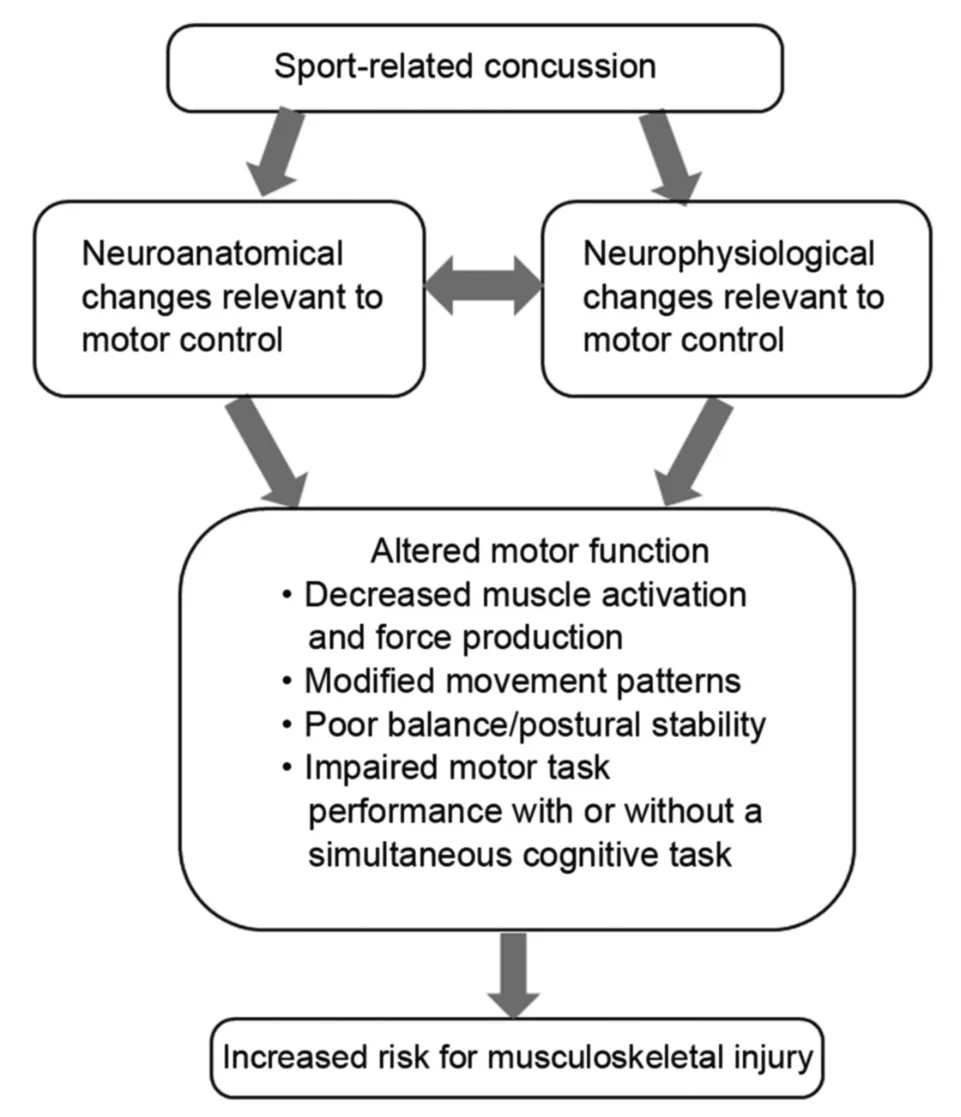
Fig.1. Conceptual framework that links unresolved impairments in motor control after sport-related concussion to an increased risk for musculoskeletal injury.
4. Evidence for subclinical changes in the central nervous system relevant to motor control after SRC
4.1. Neuroanatomic changes
Diffusion tensor magnetic resonance imaging has been used to evaluate white matter microstructure integrity after concussion, including SRC.43-51Abnormalities in brain structures with a direct relationship to motor control,such as the internal capsule, cerebellar tracts, and corpus callosum,43-48,51have been revealed, although significant interindividual variability exists.49The superior and inferior longitudinal fasciculi have also shown abnormalities that could affect connectivity between systems that provide critical information for motor planning,for example,visual and spatial attention,orientation,memory, and the motor system.44,50,51While such imaging is not a standard component of SRC clinical management, the cited studies provide neuroanatomic evidence of impaired motor control after SRC.
4.2. Neurophysiological changes
Studies employing trans-cranial magnetic stimulation of the primary motor cortex have demonstrated increased cortical inhibition,increased motor activation threshold,and decreased intra-cortical facilitation after concussion.52Non-motor areas, such as the somatosensory cortex, also undergo neurophysiological changes after SRC that can impair motor control.53-55Changes in these areas may alter the somatosensory processing used to guide and modulate ongoing movement. It is of particular interest that neurophysiological changes in motor and non-motor areas of the brain appear to be dose-dependent,such that greater concussion severity or an increasing number of concussions results in greater alterations in neurophysiological function.56Importantly, these studies have shown that neurophysiological abnormalities can persist for months or even years after the concussion event,well beyond the fulfillment of clinical return to sport criteria.52,54,57Moreover, these neurophysiologic changes have been directly connected to alterations in motor function after SRC.56,58,59
5. Evidence for altered motor function after SRC
5.1. Muscle activation and force production
Voluntary muscle activation after SRC has only been examined in 1 study,which reported decreased activation of the first dorsal interosseous muscle.59On the other hand, several studies have examined muscle force production after SRC,and the results have been inconclusive.59-63For example,in one study no reduction was found in isometric force of the first dorsal interosseous muscles within 1 month post-SRC,59whereas in another study, grip strength was reported to be reduced when concussion symptoms were elevated.60Moreover, 1 study found that isometric strength of the anterolateral cervical musculature was reduced post-SRC,61but a different study found no difference in isometric strength of the cervical musculature in subjects with or without a history of concussion.62Finally,a study found no difference in isokinetic quadriceps and hamstrings strength between military personnel with or without a history of concussion;however,the same study found that the time to peak knee extension torque was slower in those with a history of concussion.63It is unclear if decreased muscle strength is a persistent outcome after SRC.Because SRC often requires a period of rest and removal from sport participation,inactivity could contribute to acute decreases in strength. It may be that measures related to how muscle is activated are more sensitive to residual impairment. In support of this supposition, 1 study found that concussed football players tasked with holding a steady submaximal force showed faster and greater force decline over time, more force variability over time, and greater perceived sense of effort compared to their uninjured counterparts.59
5.2. Movement patterns
SRC might affect movement patterns, but the manner in which it does is not yet clear. Altered inter-joint coordination and larger changes in center of mass position have been found in gait after SRC,14and it was found that leg stiffness during a single-legged jump-landing task decreased post-season in football players who sustained SRC.64This could be problematic because insufficient joint stiffness is thought to increase the risk for soft tissue injury.65,66Another study examined a twolegged jump-landing task and found no differences in lower extremity kinematics between subjects with a history of concussion and controls.67Two studies have evaluated movement patterns during a jump-cut task.67,68One of these studies reported that individuals with a concussion history displayed knee kinematics that could increase knee ligament injury risk(e.g., decreased knee varus and external rotation),68while the other study found only slightly more trunk flexion during a cut to the non-dominant side in individuals with a concussion history.67
5.3. Balance and postural stability
Deficits in balance, or postural stability, are common after SRC and could result from either direct injury to vestibular apparatus or poor integration of sensory input.17Balance is often assessed with tools such as the Balance Error Scoring System1,3The Balance Error Scoring System has been extensively researched and holds good utility for acute balance assessment (sensitivity 34%; specificity 91%-96%),69but is less able to identify deficits after 3-5 days post-concussion.70,71Postural stability was examined during a single-legged hop from a box and a single-legged squat in subjects with a history of concussion and in subjects who served as controls.72Time to stabilization after landing from the hop off a box was longer for the non-dominant limb in concussed subjects compared to controls, while no group differences were found for the dominant limb or in the squat task.72At this time, it is unclear whether balance/postural stability tasks and measures can identify persistent motor control impairments after SRC.
5.4. Motor performance
Gait performance among post-SRC subjects shows slower speed and wider obstacle clearance compared to those without concussion.14On a grooved pegboard test, performance was slower in adolescents with a recent concussion compared to controls when the non-dominant hand was used, while no group differences were found when the dominant hand was used.73Finally, playing performance following SRC has been evaluated in hockey players with a modified plus-minus statistic that assigns points based on scoring and strength of schedule.74Athletes with SRC showed an acute decline in playing performance that was similar to those with a lower extremity injury, but the decline was not long lasting.74This small body of research suggests that the type of motor task or the way motor performance is assessed could determine if a deficit is identified after SRC.
5.5. Motor performance during dual-task conditions
Pairing a motor task with a cognitive task(e.g.,counting by sevens) is known as a dual-task condition. Dual-task conditions require distribution of attention between the cognitive and motor tasks that can reveal or exacerbate poor motor task performance.75,76Generally, as the cognitive task becomes more challenging, the magnitude of the motor control impairments tends to increase.14,76Studies have shown that athletes with SRC demonstrate greater motor impairment, such as reduced speed and decreased postural stability, during dualtask gait compared to gait-only conditions.76,77Athletes with a history of concussion also perform more poorly on reactiontime reaching and side-shuffling tasks performed in a dualtask condition.78Recent work indicates that the risk of musculoskeletal injury after SRC may be directly related to the degree of motor control impairment during gait or side shuffling performed in a dual-task condition.40,79
Dual tasking is common in sport participation and could create the potential for musculoskeletal injury in an athlete with SRC in 2 ways. First, the athlete may place attention on the cognitive demands of the sport activity (e.g., recalling the play) at the expense of the motor task, potentially resulting in poor movement patterns or motor performance that put the athlete at risk for injury. Alternatively, the athlete may place attention on executing the motor task (e.g., running the play)instead of the other cognitive demands of the sport activity(e.g., observing location of other players and obstacles on the field), resulting in a missed opportunity to shape the motor plan appropriately to avoid injury.
6. Implications for SRC clinical management and rehabilitation
A key clinical issue to emerge from the conceptual model is how to ensure that motor control is sufficiently restored after SRC so that injury risk is mitigated.While motor control is not an explicit focus in current SRC clinical management,it could be argued that some tests indirectly (e.g., neuropsychological or vestibular-ocular tests) or directly (e.g., balance and gait tests)assess motor control.The evidence reviewed above suggests that these tests may not ensure that motor control is sufficiently restored when sport participation is resumed. For this reason,it is warranted to consider ways to evolve SRC clinical management to better address motor control.
A fundamental change in SRC clinical management would be to intentionally address motor control through targeted testing and rehabilitation interventions. Such a change aligns with recent concussion practice guidelines.80Also, current SRC clinical management evaluates different types of function in isolation, but it is important to recognize that motor control requires that multiple systems(e.g.,sensorimotor system, vestibular system, central nervous system, and musculoskeletal system) work together. Thus, an integrated systems approach is recommended for motor control assessment and treatment.
Motor control can be assessed through the performance of motor tasks and perceptual/cognitive challenges with increasing complexity.We recognize that no standard exists for evaluating motor task performance in relation to musculoskeletal injury risk. However, clinical judgments could be based on performance metrics, such as gait speed or cadence.40,41,81,82Clinicians could also assess for abnormal movement patterns,including those known to increase musculoskeletal injury risk.83Movement patterns can be analyzed during various motor tasks with visual observation or 2-dimensional techniques,84-86which are more feasible in clinical and field settings compared to 3-dimensional analysis. To date, no movement variable has been sufficiently correlated with injury risk in the SRC population to justify the time and cost of 3-dimensional analysis. Performance on perceptual/cognitive tasks can be assessed by comparing performance under dualtask conditions to performance without a concurrent motor task or possibly to pre-SRC performance.
The selection and progression of motor tasks and perceptual/cognitive tasks should be given careful consideration.Motor task selection can be guided by general principles for therapeutic exercise and motor learning.87,88Motor tasks with low physical demand may be presented before progressing to those with higher physical demand, and all motor tasks may first be presented in isolation before presenting with a perceptual/cognitive challenge(i.e.,dual-task condition).It is best to select motor tasks with relevance to the athlete’s activities of daily living and/or sports participation for better generalizability beyond the rehabilitation setting,87and complex motor tasks may need to be practiced in parts for successful completion.22The selection of cognitive/perceptual tasks should be guided by task complexity and knowledge of the athlete.Simple cognitive challenges, such as counting backwards by sevens,may be presented before progressing to those that involve greater cognitive processing, such as Stroop tasks. Some athletes might naturally have more difficulty with certain types of cognitive tasks,such as math-based challenges,and that should be considered when selecting the cognitive task.
An example of clinical application would be to first assess motor performance during low-demand motor tasks such as gait, static balance tests, or squatting. If an athlete demonstrates difficulty performing a motor task, then the motor task becomes a rehabilitation intervention by allowing practice with appropriate feedback.It may be advantageous in an early stage of rehabilitation to encourage implicit learning so as not to stress cognitive resources.Once the athlete demonstrates proficiency with the motor task, a perceptual/cognitive task can be added,starting with easier challenges such as calling out numbers on playing cards presented to the athlete,which acts as a visual distractor. Perceptual/cognitive tasks that involve visual and/or auditory stimuli should be considered because both types of sensory input are encountered during sport participation.Once the athlete demonstrates proficiency in low-demand motor tasks with low-demand perceptual/cognitive tasks, the athlete can be presented with highdemand motor tasks,such as jumping.When the motor task is performed appropriately, a perceptual/cognitive task may be added(e.g.,the athlete adds the last 2 numbers seen in order to challenge working memory or calls out numbers written on balls tossed to the athlete).If intervention is needed,feedback to encourage explicit learning may be used in this advanced phase.The next progression includes sport-specific motor tasks(e.g.,performing a lay-up)and perceptual/cognitive tasks(e.g.,performing a lay-up with a defender) that are similar to what the athlete will encounter during sport participation.
It may also be advantageous to incorporate resistance training into rehabilitation to facilitate better motor output.89This runs somewhat counter to current trends,which emphasize the use of aerobic activity.1However, resistance training induces neuroplastic changes in the motor cortex, such as an increase in corticospinal excitability,a decrease in corticospinal inhibition, and an increase in intra-cortical facilitation,90,91which could address cortical deficits after SRC. Moreover, having the athlete perform resistance training with auditory cues from a metronome could increase corticospinal excitability and decrease intra-cortical inhibition more than self-paced resistance training, thus possibly helping to improve motor skill performance over time.92At this time,there is no guidance on appropriate timing and dosage for resistance training after SRC.It is reasonable that resistance training could be initiated in a controlled,graded fashion as the athlete approaches return to sport participation and can tolerate demanding physical and perceptual/cognitive challenges.
Once an athlete shows proficiency with motor tasks combined with perceptual/cognitive tasks in the clinical setting and fulfills other return to sport criteria, a return to sport continuum can be initiated.93A return to sport continuum allows for gradual,progressive exposure to sport activities before participating in full competition.93Limits are initially placed on the intensity, duration, and contact nature of sport participation. This may be particularly important for athletes with protracted recovery after SRC in which deconditioning could also contribute to the risk of musculoskeletal injury. If an athlete displays poor motor or perceptual/cognitive performance at any point during the return to sport continuum, the athlete would be given contextual drills to facilitate better motor control before continuing to progress toward the intensity and duration of sport participation.
7. Summary and future directions
This review presents a conceptual framework that links impairments in motor control after SRC to an increased risk for musculoskeletal injury. The evidence for motor control impairments after SRC includes neurobiological changes in the central nervous system and altered motor function that persist beyond the time of return to sport. A clinical implication of the conceptual framework is a need to intentionally assess for and treat motor control impairments after SRC to mitigate musculoskeletal injury risk. One way motor control could be assessed is by observing a motor task being performed with or without a perceptual/cognitive task. It is expected that many athletes with SRC will demonstrate motor task performance deficits that indicate a need for rehabilitation, and this may require a change in practice if supervised rehabilitation is currently offered only to athletes with persistent symptomology.In addition, motor control may need to be assessed even after the return to sport continuum is initiated because treatment clinics do not fully replicate the demands of sport participation and because motor learning can attenuate over time.94,95
Additional research is needed on the conceptual framework and SRC clinical management approach suggested in our review.Foremost,research is needed to directly confirm a link between motor control impairment and musculoskeletal injury in athletes with SRC. This may also include examining whether the motor control impairment results from an inability to perceive sensory cues,difficulty processing sensory cues,or challenges in motor planning or motor learning related to cognitive deficits, as demonstrated in a recent study.96Since the suggested SRC clinical management approach is more resource intensive than current approaches,it would be advantageous to identify subgroups of athletes with SRC who are at the greatest risk for subsequent musculoskeletal injury. Similarly, further investigation is needed to identify which motor tasks and measures are predictive of musculoskeletal injury risk in order to give clinicians tools for monitoring rehabilitation progression,including return to sport clearance.It may be of benefit to explore motor tasks involving the upper extremities for athletes who participate in sports with high upper extremity demands. Finally, the risk-reductive and performance-enhancing effects of SRC rehabilitation targeting motor control need to be examined,as well as comparing motor control outcomes in athletes who do or do not participate in such rehabilitation.
Authors’contributions
TLC contributed to the creation of the conceptual model,conception of the manuscript,literature review,and the writing of the manuscript;JT assisted with the conception of the manuscript, literature review, and writing of the manuscript; SS assisted with the literature review and writing of the manuscript; MH provided content expertise in athlete rehabilitation and return to sport decision-making and contributed to writing of the manuscript; DSR provided content expertise related to motor control and rehabilitation of motor control impairments and contributed to writing of the manuscript; RMB provided content expertise in neurophysiological testing and impairments after concussion and contributed to writing of the manuscript; JRC provided content expertise in concussion management and contributed to writing of the manuscript;DCH contributed to the creation of the conceptual model,conception of the manuscript, and writing of the manuscript. All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
 Journal of Sport and Health Science2021年2期
Journal of Sport and Health Science2021年2期
- Journal of Sport and Health Science的其它文章
- Factors associated with concussion-symptom knowledge and attitudes toward concussion care seeking in a national survey of parents of middle-school children in the US
- Effects of purposeful soccer heading on circulating small extracellular vesicle concentration and cargo
- The diagnostic and prognostic utility of the dual-task tandem gait test for pediatric concussion
- Impaired eye tracking is associated with symptom severity but not dynamic postural control in adolescents following concussion
- Slowed driving-reaction time following concussion-symptom resolution
- Detailed description of Division I ice hockey concussions:Findings from the NCAA and Department of Defense CARE Consortium
