The diagnostic and prognostic utility of the dual-task tandem gait test for pediatric concussion
Ktie A.Vn Deventer,Corrine N.Seehusen,Gregory A.Wlker,c,Julie C.Wilson,c,d,Dvid R.Howell,c,*
a University of Colorado School of Medicine,Aurora,CO 80045,USA
b Sports Medicine Center,Children’s Hospital Colorado,Aurora,CO 80045,USA
c Department of Orthopedics,University of Colorado School of Medicine,Aurora,CO 80045,USA
d Department of Pediatrics,University of Colorado School of Medicine,Aurora,CO 80045,USA
Abstract
Keywords: Adolescent;Balance;Mild traumatic brain injury;Postural stability;Prognosis
1. Introduction
Concussion, a brain injury induced by traumatic biomechanical forces,results in altered mental status and/or functional disturbances detectable through balance, motor control,vestibular, o
r oculomotor assessments.1An array of clinical tools is currently available for concussion diagnosis and management, but substantial variability in practice patterns exists.2,3One common assessment is the Sports Concussion Assessment Tool(SCAT),which has evolved through multiple iterations over the past 2 decades.4The current version, the SCAT5,includes assessment of the athlete’s symptoms,cognitive and neurological functions, and postural stability, which includes evaluations of balance and gait. The impact of concussion on postural stability—the ability to maintain an upright position—has been widely documented by using both balance- and gait-based tasks.5-8Within the SCAT5,postural stability is assessed via the modified Balance Error Scoring System(mBESS)and tandem gait tests.9,10
The mBESS is among the most commonly used concussion assessments.2It is easily implemented, providing a viable measure for use within a variety of practice settings.The clinical utility of the mBESS, however, appears to decline after approximately 5 days post-concussion,11although several prior studies suggest functional balance impairments linger beyond this time.12,13Various limitations have been identified as well,including poor reliability,low sensitivity,14-17and effects related to fatigue,testing environment,and ankle instability.14,18-20The mBESS tandem stance condition has,however,shown prognostic value in the prediction of persistent post-concussion symptoms(PPCS),defined as symptoms that persist >28 days after concussion.21,22More sophisticated measures(e.g.,optical motion analysis)appear to provide relevant postural-control information after concussion13,23-26but can be cost-prohibitive and time-intensive.Thus,they are difficult to implement in most clinical settings.
The tandem gait test blends clinical viability with complex motor control requirements. Recent studies indicate that it is useful for identifying coordination, dynamic balance, and locomotion impairments after a concussion.27-29One study of collegiate athletes reported slower (i.e., worse) tandem gait times acutely post-concussion compared to a baseline(pre-injury) examination, but the athletes had similar mBESS performance between baseline and post-injury assessments.30The authors concluded that the tandem gait test might be a useful alternative to the mBESS for concussion management.Yet the methodology for assessing concussion using the tandem gait test is still based primarily on work performed in collegeaged and adult populations. One recent study of a pediatric concussion population reported that a tandem gait assessment was more useful for distinguishing concussions relative to the control group than an instrumented quiet stance assessment.5Within tandem gait assessments, dual-task approaches, where patients complete the tandem gait test while simultaneously completing a cognitive task, may be useful.13,23,25,31,32The addition of a cognitive task during a tandem gait test results in longer detectable deficits post-concussion relative to healthy controls than do single-task tests.28However, the clinical significance of such differences is currently questionable, given that few studies have reported outcomes beyond betweengroup(healthy vs.concussion)comparisons.
Emerging concussion prognosis methods have been described in recent years,21,22but additional objective information about the risk of developing PPCS may assist clinical decision making.Previous work suggests that certain factors,such as demographics,medical history,initial symptoms,and cognitive symptoms, collectively provide utility in assessing PPCS risk,21,22although even when combined, these elements may account for only a small percent of recovery variability.33Furthermore, the utility of postural stability tests in providing prognostic information has not been fully explored.Therefore,although single- and dual-task tandem gait testings demonstrate promise for detection of deficits after concussion,further work is required to determine whether this method can enhance both diagnosis and prognosis for pediatric concussion.
The purpose of this study was to determine the diagnostic and prognostic value of single-and dual-task tandem gait performance and mBESS performance in pediatric concussion. To achieve these goals, we (1) compared patients with concussion assessed within 10 days of injury relative to controls and (2) compared patients with concussion assessed within 10 days of injury who did and did not go on to develop PPCS after initial testing.Based on existing literature,28,30we hypothesized that the concussion group would have slower single- and dual-task tandem gait test times than controls. We also hypothesized that concussion patients tested within 10 days of injury who developed PPCS would have slower single- and dual-task tandem gait test times than those who recovered within 28 days of injury and that no differences would be detected between groups for the mBESS.
2. Methods
2.1. Study design and participants
We retrospectively examined data from patients who were seen for concussion at the Children’s Hospital Colorado Sports Medicine Center between January 1, 2019, and December 31,2019, and who underwent a standardized set of concussion assessments as a part of their routine clinical care. Patients included in the concussion group were seen within 10 days of injury,diagnosed with a concussion by a sports medicine physician,and returned for follow-up care according to their individual clinical needs until they no longer required care or were referred to another specialist.In addition,we enrolled a cohort of healthy control subjects during a sports pre-participation evaluation to serve as comparisons to concussion patients.Prior to our study, the Colorado Multiple Institutional Review Board approved the protocol as an exempt study in that it retrospectively reviewed existing medical records, and all participants signed written informed consent to participate in the study.
At each clinical visit, patients with concussion and their caregivers answered standardized questions, and patients participated in a standard set of postural stability tests administered by athletic trainers or trained research staff.We excluded concussion patients if they (1) had not been diagnosed with a concussion (e.g., had a alternative diagnosis), (2) were older than 18 years of age or younger than 6 years of age, (3) were seen for their initial visit >10 days post-injury, (4) were asymptomatic at the initial clinical visit,(5)had an abnormality on neuroimaging,(6)had sustained a recent or concomitant orthopedic injury, or (7) had sustained a subsequent head injury prior to clearance from the injury prompting the initial clinical evaluation. Concussion clinical management aligned with consensus guidelines,4with individualized recovery plans for physical activity, school, and cognitive activity. Control participants were not eligible for recruitment if they (1) were older than 18 years of age or younger than 6 years of age, (2)had sustained a medically diagnosed concussion within 6 months of the assessment or were still experiencing symptoms from a previous concussion,or(3)had a lower-extremity injury that affected balance.
2.2. Symptom severity
Patients in the concussion group reported their current concussion symptoms using the Health and Behavior Inventory(HBI),34a 20-item scale that measures the frequency of symptoms associated with concussion.Patients completed the child version,and an accompanying caregiver completed the parent version. Each version used a 4-point Likert scale to measure the frequency of symptoms: 0 (never), 1 (rarely), 2 (sometimes),and 3(often).33A total symptom score was also calculated as the sum of the individual frequency scores of all items,with a maximum score of 60.
Concussion patients then recorded whether they were still experiencing concussion symptoms at each follow-up clinical evaluation.If their symptoms had resolved(HBI score=0),they recorded the last date they had experienced symptoms, and symptom resolution time was then calculated in days from the date of injury. As is consistent with previous work,21,22we defined PPCS as symptom resolution >28 days post-injury,although we recognize that varying definitions and disagreements exist pertaining to this definition.35To address our 2nd study purpose,we classified concussion patients into sub-groups based on symptom duration: (1) those who reported symptoms>28 days post-injury (PPCS group) or (2) those who reported symptom resolution ≤28 days post-injury (No PPCS group).Those patients who were seen more than 28 days post-injury and were still symptomatic were included in the PPCS group.
2.3. The mBESS
Certified athletic trainers or trained research staff administered the postural stability assessments.The mBESS is a static balance assessment wherein patients complete 3 stance conditions (double-leg, single-leg, and tandem stance) for 20 s while standing with their eyes closed, hands on hips, and on firm ground.Patients stood with their feet side by side for the double-leg stance and stood on what they identified as their non-dominant kicking foot for the single-leg stance. Tandem stance was completed with the non-dominant foot directly behind the dominant foot. As is consistent with previously established methods,30the test administrator counted the total number of errors during each trial,with a maximum of 10 per condition.We counted an error if patients opened their eyes,lifted their hands off their hips,took a step, fell out of the testing position, lifted one of their feet off the ground (during double/tandem stance), abducted their hip more than 30°, or stayed out of the test position for >5 s. The number of errors committed in each mBESS condition was the primary outcome,with a total score ranging from 0 to 10 per condition.We also calculated the total mBESS score(sum of errors made across all conditions). The inter-rater reliability of the mBESS has been previously reported to be moderate.15
2.4. Single-and dual-task tandem gait test
The administration of the tandem gait test was consistent with previously published studies and standardized instructions.9,28,36Patients were instructed to walk, as quickly as possible, heel-totoe and without shoes,along a strip of tape 3 m in length,make a 180˚turn beyond the end of the tape and then return to their starting point with the same heel-to-toe gait.Times were recorded to the nearest hundredth of a second using a stopwatch or Smartphone.Overt separation of heel and toe,stepping off the tape,or touching the test administrator or wall were used to define a failed trial,and the trial was repeated if a failed trial occurred.The dualtask trial required patients to complete one of 3 different cognitive tasks while simultaneously walking heel-to-toe: (1) serial subtraction by 6 s or 7 s from a randomly presented 2-digit number;(2)reciting months in reverse order starting from a randomly selected month; or (3) spelling a 5-letter word backward. For younger children(7-11 years of age),we adjusted these tasks so that they (1) completed the serial subtraction by 3 s, (2) recited the days of the week in reverse order, or (3) spelled a 4-letter word backward.These cognitive tasks used during dual-task trials were varied across trials in order to avoid a practice effect and have been used in prior studies of dual-task tandem gait with high reliability in both single-task and dual-task forms of the test.6,28,31Outcomes included average test time for single- and dual-task tandem gait tests and dual-task cognitive accuracy.Average tandem gait test time was calculated as the mean the trial time across the 3 trials,calculated separately for single-and dualtask conditions. Dual-task cognitive accuracy was calculated as the number of correct trials divided by the total number of trials completed. To determine test performance, we elected to use average test time as our primary outcome rather than a pass/fail outcome(as specified in the SCAT5)because of the subjectivity of the pass/fail method.
2.5. Statistical analysis
Data are presented as means(standard deviation(SD)or 95%confidence intervals(95%CIs))for continuous variables and the number of patients and corresponding percentage within a group for categorical outcome variables. We compared demographic and injury characteristics between concussed (PPCS and No PPCS) and healthy control groups, using one-way analyses of variance and x2analyses.For our primary purpose,we compared concussion and control groups on tandem gait and mBESS outcomes using independent samples t tests.We calculated area under the curve(AUC)values via receiver operating characteristic (ROC) curves to identify the discriminatory value between concussed and control groups for each variable. AUC values were defined as excellent (>0.9-1.0), good (>0.8-0.9), fair(>0.7-0.8), or poor (≤0.7). For our secondary purpose, we compared PPCS and No PPCS groups on tandem gait and mBESS outcomes using independent samples t tests. We then calculated AUC values to identify the classification ability for each postural stability measure in those who did and did not develop PPCS. For both purposes, we then identified optimal cut-points (i.e., highest classification accuracy) from AUC values,along with the corresponding sensitivity and specificity values for the single- and dual-task tandem gait tests at these cutpoints.Finally,we used multivariable ROC models to assess the combined ability of each postural test outcome, along with symptom severity,age,and time from injury to assessment so as to classify those who developed PPCS and those who did not.There were limited instances where data were missing (5 controls did not have mBESS data;1 control did not have dual-task cognitive accuracy data). Any missing data were treated as such, and no imputations were performed. Statistical significance was determined as p <0.01 to account for multiple comparisons. All statistical tests were two-sided and performed using Stata Version 15(StataCorp.,College Station,TX,USA).
3. Results
3.1. Study participants
For our cohort of patients with concussion, a total of 337 patients underwent evaluation for concussion during the study period.We excluded 211 concussion patients from the analysis(n=98 completed the initial assessment >10 days post-injury;n=37 did not complete the tandem gait test; n=32 were asymptomatic at the 1st clinical visit; n=29 did not receive a concussion diagnosis;n=7 were not seen by a sports medicine physician; n=5 sustained a 2nd concussion before resolution of the first; n=2 presented with traumatic neuroimaging abnormalities;n=1 was outside the ages of 6-18 years).After applying inclusion and exclusion criteria, a total of 126 concussion patients were included in this investigation. There were no significant differences between concussion patients who were included and excluded in the study in mean age(p=0.59), proportion of females (p=0.62), or proportion of patients with a prior concussion history(p=0.53).
Of the patients we included in our analysis, 31 (25%)developed PPCS, 81 (64%) recovered within 28 days of injury,and 14(11%)did not have reliable data to determine PPCS designation. In addition, 58 healthy controls participated in the study and completed the test protocol. The healthy control group was significantly older than the concussed No PPCS group,and a significantly greater proportion of the concussed subjects had histories of concussion relative to the healthy control group.Furthermore, among the concussion group, the PPCS group reported significantly greater symptom burden at the initial visit(Table 1).
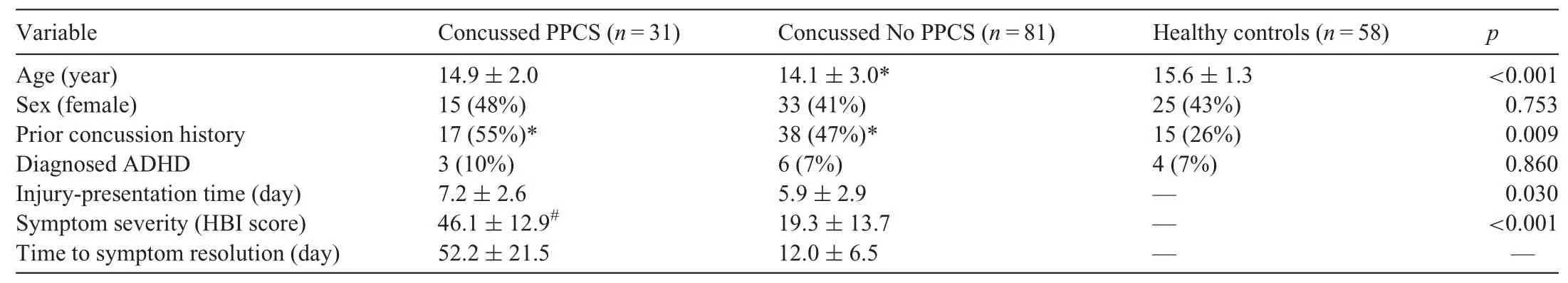
Table 1 Demographic and injury characteristics of the PPCS,No PPCS,and control groups.
3.2. Concussion vs.control group comparisons
For our 1st aim, we compared the concussion and control groups. We observed that patients diagnosed with concussions had significantly slower times on the single-and dual-task tandem gait tests (Fig. 1), demonstrated worse dual-task cognitive accuracy, and made more errors on the single and tandem mBESS stances compared to controls. AUC values suggested that both single- and dual-task tandem gait test times provided good discriminatory information for diagnosing concussion compared to healthy controls(Table 2).For the single-task tandem gait test,a cut-point of 16 s provided 87.5%sensitivity and 72.4%specificity and correctly classified 82.4%of patients as concussed or control. For the dual-task tandem gait test, a cut-point of 22 s provided 84.8% sensitivity and 72.4% specificity and correctly classified 80.6%of patients as concussed or control.

Fig. 1. Diagnostic data. Individual data points describing the distribution of single-task(A)and dual-task(B)tandem gait times for concussion and control groups.The line within the plot indicates the mean value.Significant betweengroup differences were observed for both single-task and dual-task assessments(p <0.001).
3.3. Concussion group sub-analysis:PPCS vs.No PPCS
When comparing concussion patients who did and did not develop PPCS,the PPCS group had significantly slower times on the dual-task tandem gait test than the No PPCS group during the initial evaluation (Fig. 2). However, the PPCS and No PPCS groups were not significantly different in single-task tandem gait times,dual-task cognitive accuracy,or mBESS measures after adjusting for multiple comparisons(Table 3).For the single-task tandem gait test, a cut-point of 39.2 s provided 16.1%sensitivity and 97.5%specificity and correctly classified 75.0%of patients as PPCS or No PPCS.For the dual-task tandem gait test, a cut-point of 54 s provided 22.6% sensitivity and 95.1% specificity and correctly classified 75.0% of patients as PPCS or No PPCS.
Multivariable ROC results indicated a high classification ability for the single- and dual-task tandem gait tests, along with age, time from injury to assessment, and symptom score(AUC=0.95 for both single-and dual-task models)for classifying those who did and did not develop PPCS.

Table 2 The diagnostic ability of the postural control test battery between concussed and control groups.

Table 3 The prognostic ability of outcome measures administered within 10 days of concussion to distinguish between those who developed PPCS and those who did not.
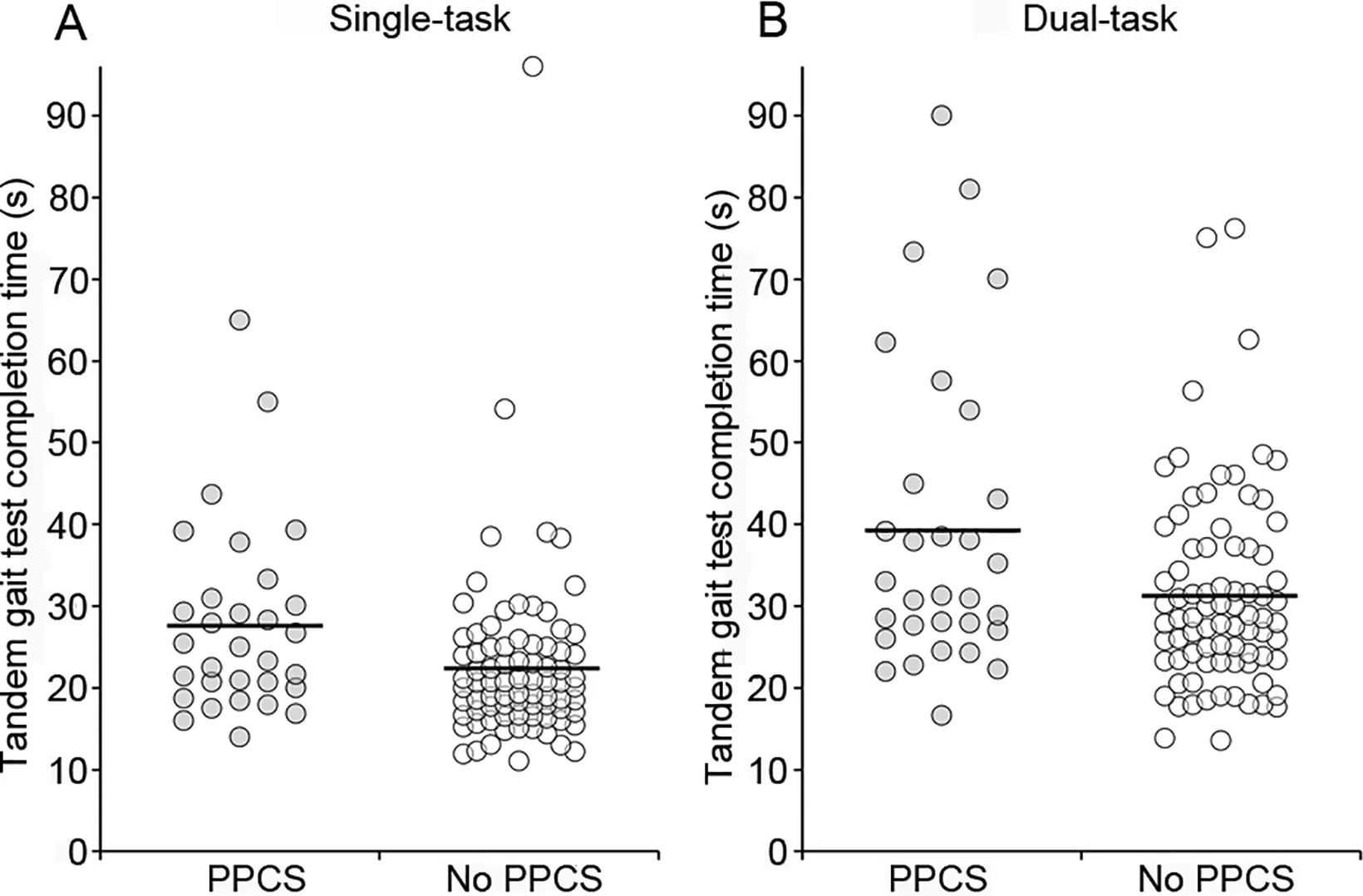
Fig. 2. Prognostic data. Individual data points describing the distribution of single-task(A)and dual-task(B)tandem gait times for the group with persistent post-concussion symptoms (PPCS) and the No PPCS groups. The line within the plot indicates the mean value. Significant between-group differences were observed for dual-task assessments(p=0.009).
4. Discussion
In this study,we examined how clinically viable postural stability assessments were able to distinguish between concussion patients evaluated within 10 days of injury and healthy control patients as well as their ability to provide prognostic information regarding persistent post-concussion symptoms in a pediatric population. The data from our investigation were consistent with previous studies supporting the utility of the tandem gait test within concussion management,28-31the majority of which have been done in college-age and youngadult populations. The pediatric patients with concussions we studied demonstrated impaired performance on both mBESS and tandem gait measures compared to healthy controls. Interestingly,we found that the single-and dual-task tandem gait test times had considerably greater diagnostic ability to distinguish between concussion and control groups than did the mBESS or the dual-task cognitive test.Furthermore,our data indicated that dual-task tandem gait assessments may also provide better prognostic value for determining those who are likely to experience PPCS compared to other balance measures. However, the low sensitivity and high specificity for PPCS prognosis suggest that the dual-task tandem gait test should be used as a screening tool rather than as a prediction tool within the first 10 days of concussion. Therefore, clinicians may consider integrating dual-task tandem gait tests within concussion evaluations to identify deficits and guide management pathways.
Our results suggest that concussed athletes performed worse on both mBESS and tandem gait outcomes relative to healthy controls.This finding aligns with past research,14,17,31in that in our study, different postural stability assessment approaches were able to distinguish between concussed and control groups during the 1st week post-concussion.The mBESS is helpful for concussion diagnosis during field-side assessments,with detectable differences typically decreasing 5-7 days post-injury.11,17Assessment in our sports medicine clinic occurred 2-10 days post-injury. Within this time window, our AUC results suggest that both single- and dual-task tandem gait times provide a greater level of sensitivity and specificity for detecting post-concussion deficits than the number of mBESS errors committed in each condition.Therefore,our data suggest that the tandem gait test may augment existing clinical practices and provide meaningful clinical insights. Furthermore, the cut-points we calculated provide some context for clinicians who administer the tandem gait test within their multifaceted concussion evaluation.For example,a clinician can be reasonably confident in concussion diagnosis if an athlete presents and cannot complete the single-task tandem gait test in <16 s. Further work is necessary,however,to determine the feasibility and utility of this approach for identifying recovery from concussion.
Although each of the 4 outcome variables of interest demonstrated significantly worse performance for concussion patients relative to controls,tandem gait test times(during single-or dualtask conditions) demonstrated the best diagnostic value. These findings reinforce previous work supporting the clinical value of tandem gait assessments.28The addition of a cognitive task, as conducted in our dual-task tandem gait test, suggested a similar benefit in sensitivity when diagnosing concussions.
Our study has potential clinical application for health care providers, who may want to use the dual-task tandem gait test as a part of their routine clinical examinations for concussion.Our results suggest that the dual-task tandem gait test may be considered alongside other established methods for stratifying PPCS risk21,22when attempting to identify those who may benefit from additional treatment or closer monitoring after a concussion within the first 10 days of injury. Our cut-point data suggest, however, that, given the low sensitivity and high specificity observed, the dual-task tandem gait test may be used best in the context of a screening tool to rule out the likelihood of PPCS development rather than as a tool to predict its development. Other investigations have examined possible clinical predictors of PPCS in the pediatric population, such as the severity of acute and sub-acute symptoms, resulting in mixed findings regarding which approaches are most beneficial.33Building upon prior research, the dual-task tandem gait test may add incremental value to clinical models of concussion prognosis for use in sports medicine settings.However,future work aimed at replicating our findings across various ages, geographic settings,and points of health care entry,will be required.
In our study,participants performed tandem gait and mBESS assessments in the context of a routine clinical examination in a sports medicine clinic. The assessments were administered by athletic trainers who worked alongside physicians to evaluate the patients.The addition of tandem gait assessments represents an easily implemented test during standard evaluations or during acute sideline scenarios. Another advantage of this multimodal evaluation is that the only materials needed to measure dynamic and static postural stability, as well as cognitive performance,are a strip of fabric or tape, a quiet walkway, and a watch. In addition,health care providers can easily administer tandem gait tests outside the clinic, enhancing sideline management. Thus,health care providers across many different clinical settings may be able to administer this assessment without the need for extensive equipment,time,space,or training.
The limitations of this study should be considered when interpreting our observations.Although inclusion and exclusion criteria were implemented in the study design to improve the homogeneity of patients, we cannot generalize these results to other populations of different ages,geographic regions,or points of health care entry.Furthermore,we used an alternative version of the test in patients 11 years of age or younger(9%of our sample). This may have led to some variability in our observed results. Age may have affected task performance as well, given that the control group was older than the concussion group. In addition,although athletic trainers and physicians were instructed on testing procedures for both mBESS and tandem gait tests prior to clinical implementation,it is possible that there were variations across the various clinical settings where the protocol was administered,and they may have influenced our results.
5. Conclusion
Our data further support the clinical utility of tandem gait tests within clinical concussion evaluations.Our data also suggest that single- and dual-task tandem gait assessments have diagnostic and prognostic value for clinicians who evaluate pediatric patients with concussions.Using these methods to rule out a high likelihood of PPCS development early post-injury may lead to improved and more individualized rehabilitation pathways.
Acknowledgments
DRH has received research support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development(R03HD094560),the National Institute of Neurological Disorders and Stroke (R01NS100952, R03HD094560, and R43NS108823),and MINDSOURCE Brain Injury Network.The remaining authors have no disclosures.
Authors’contributions
All authors contributed to the conception and design of the work and the interpretation of the data. KAVD contributed to the acquisition of the data and the drafting of the work; CNS contributed to the acquisition of the data and the revision of the work for important intellectual content; DRH contributed to the analysis of the data and the drafting of the work;GAW and JCW contributed to the revision of the work for important intellectual content. All authors have read and approved the final version of the manuscript,agree with the order of presentation of the authors, and agree to be accountable for all aspects of the work.
Competing interests
The authors declare that they have no competing interests.
 Journal of Sport and Health Science2021年2期
Journal of Sport and Health Science2021年2期
- Journal of Sport and Health Science的其它文章
- Factors associated with concussion-symptom knowledge and attitudes toward concussion care seeking in a national survey of parents of middle-school children in the US
- Effects of purposeful soccer heading on circulating small extracellular vesicle concentration and cargo
- Impaired eye tracking is associated with symptom severity but not dynamic postural control in adolescents following concussion
- Slowed driving-reaction time following concussion-symptom resolution
- Impaired motor control after sport-related concussion could increase risk for musculoskeletal injury:Implications for clinical management and rehabilitation
- Detailed description of Division I ice hockey concussions:Findings from the NCAA and Department of Defense CARE Consortium
