A case of a successful post-transcatheter aortic valve replacement His bundle pacing
Fei Lv, Xiao-hong Pan, Jia-qi Fan, Li-han Wang, Dan-dan Yang, Xin-ping Lin, Hua-jun Li, Qi-feng Zhu, Xian-bao Liu, Jian-an Wang
Department of Cardiology, the Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310009, China
Dear editor,
Transcatheter aortic valve replacement (TAVR) is a safe and effective treatment for severe aortic valve stenosis and aortic regurgitation. Multiple randomized trials have proved its therapeutic advantages in patients at any level of surgical risks.[1-3]However, new-onset conduction disorders,including atrioventricular block (AVB) and left bundle branch block (LBBB), are the most common complications after TAVR procedure,[4]and might lead to deteriorated hemodynamics and worsened clinical outcome. Our center predominantly uses the self-expanding valves, with an incidence of new-onset conduction disorder following TAVR at around 10%. After TAVR, complete AVB usually requires pacemaker implantation, and the presence of newonset LBBB is associated with increased risk of heart failure, complete AVB, and mortality.[5,6]We have a standard protocol to closely observe the post-TAVR electrocardiogram(ECG) changes and identify the ones that require permanent pacemaker implantation. However, conventional pacing mode, with right ventricular lead placed at either the apex or septum, is not capable of correcting QRS width, thus failing to restore the contraction sequence of the ventricular wall.His bundle pacing (HBP) is a new trend to achieve more physiological QRS complexes and ventricular contraction.In a multicenter study of 16 patients who developed newonset LBBB following TAVR to explore the feasibility and safety of HBP, notably narrowed QRS was achieved in 11 patients (69%), but they only recruited patients with balloonexpandable valves, in addition to a small sample size.[7]In this case report, we successfully implanted a permanent pacemaker with HBP technique to correct TAVR-induced AVB in an old female patient.
CASE
A 69-year-old female patient presented for recurrent chest pain and shortness of breath. She had an unremarkable coronary angiography. An echocardiogram revealed severe aortic regurgitation with a mean pressure gradient of regurgitated jet at 11 mmHg (1 mmHg=0.133 kPa) and a maximum velocity at 2.32 m/s. The baseline left ventricular ejection fraction (LVEF) with biplane Simpson’s method was 71%. She had a history of well-controlled hypertension.Due to her recurrent and worsening symptoms, we advised her to consider surgical aortic valve replacement. However,the patient refused open-heart surgery and asked for alternative methods. Based on this, our heart team suggested mini-invasive trans-femoral TAVR. An informed consent form was obtained from the patient and her family. After a comprehensive pre-TAVR assessment, a 29-mm VenusA Valve (Venus Medtech, Hangzhou, China) was selected(Figure 1). The TAVR procedure was performed on 28 November 2019. After balloon pre-dilation, we released the VenusA Valve at the bottom of aortic sinus. The postprocedural digital subtraction angiography (DSA) showed that the mean depth of the implanted valve was 5.53 mm.The prosthetic valve successfully attenuated the aortic regurgitation with the mean pressure gradient decreased to 2 mmHg, and the maximum velocity dropped to 0.8 m/s.Meanwhile, we found a new-onset third-degree AVB with widened QRS. After one week, there was no improvement in her complete AVB. On the 9thday after TAVR, we implanted a dual-chamber permanent pacemaker with HBP technique.The right ventricular pacing lead (3830, Medtronic Inc.,Minneapolis, USA) was screwed into the septum at the level of His bundle, using a fixed curve sheath (C315HIS,Medtronic). The QRS duration and morphology were recorded and analyzed through an intracardiac electrogram.At the f irst time, the classical “W” type morphology of QRS complexes was not observed at lead V1. We adjusted the pacing lead according to the anatomical landmark of His bundle and intracardiac electrogram. Finally, we screwed the lead at the optimal position. When we paced the 3830 lead,there was no right bundle branch block (RBBB) recruitment,which indicated a successful non-selective HBP. The atrial lead was screwed into the right appendage with a 2088TC lead (Abbott, Chicago, USA), and then connected to PM2224 dual-chamber pacemaker (Abbott, Chicago, USA).Post-HBP ECG showed sinus rhythm, ventricular pacing on atrial sense-ventricular pacing (AS-VP), and the QRS width at 107 ms.
At the one-month follow-up visit, the patient was asymptomatic with improved exercise tolerance, at New York Heart Association (NYHA) function class I. Computed tomography (CT) revealed the prosthetic valve and pacing leads were in a good position. An echocardiogram showed LVEF of 55.1%. Aortic valve area was 2.22 cm2, with a mean pressure gradient of 2 mmHg and a maximum velocity of 1.18 m/s. An ECG showed AS-VP with QRS width at 104 ms (Figure 2).
At the one-year follow-up visit, the patient remained asymptomatic and active in daily activities. The LVEF with biplane Simpson’s method was 69.6%, and the prosthetic valve area was 2.19 cm2. There was no obvious regurgitation of the prosthetic valve identif ied. Cardiac CT also showed a stable position of the prosthetic valve and the pacing leads.
DISCUSSION
New-onset AVB is a common and severe post-TAVR complication, and impairs the outcomes of TAVR.Irreversible AVB mandates permanent pacemaker implantation. The conventional ventricular pacemaker is wildly used in patients with post-TAVR AVB, but it increases the risks of ventricular dyssynchrony and heart failure due to widened QRS duration. The HBP technique is superior to conventional right ventricular pacing in terms of narrowing QRS width and restoring ventricular synchrony, which ultimately improves the outcomes.
The anatomical structure of interventricular septum and the depth of valve implantation are associated with post-TAVR conduction disorders. In our case, the patient’s interventricular septum thickness was 1.4 mm as shown in CT, and the mean valve implantation depth was 5.32 mm,which might lead to the new-onset post-TAVR AVB. Also,the patient’s His bundle area was narrower and longer than the usual AVB patients.
In this report, the patient underwent HBP after TAVR due to a new-onset AVB with widened QRS. At one-month and one-year follow-up visits, she felt well with a good cardiac performance.
This successful case of post-TAVR HBP implies that the HBP can be an efficient way to correct TAVR-induced conduction system abnormities, especially in those with a widened QRS. In the future, we still need more cases of post-TAVR HBP to better understand the pros and cons of this novel technique.
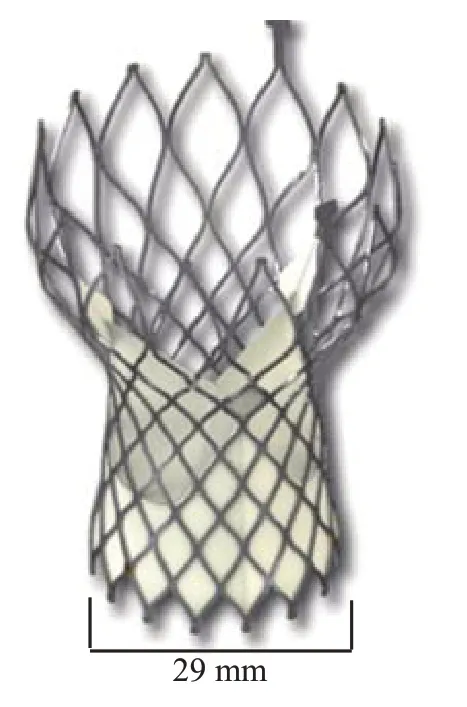
Figure 1. The VenusA Valve.
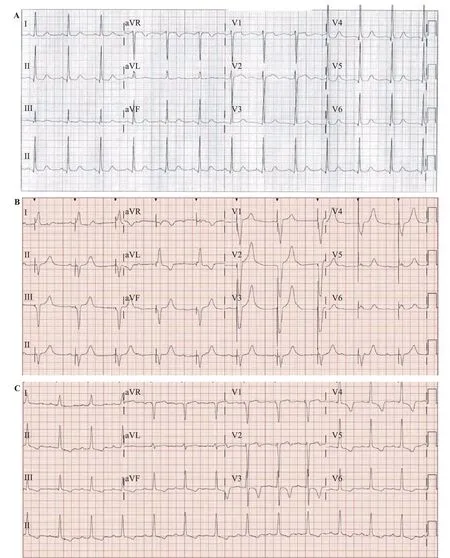
Figure 2. ECG changes of the patient. A: ECG before TAVR showed sinus rhythm, prolonged QT interval, ventricular sinister high potential,PR interval 174 ms, QRS 96 ms; B: post-TAVR ECG with temporary pacemaker showed AVB III, QRS 148 ms; C: ECG with HBP showed ventricular sinister high potential, PR interval 243 ms, QRS 107 ms; ECG: electrocardiogram; TAVR: transcatheter aortic valve replacement. AVB III: third degree atrioventricular block; HBP: His-bundle pacing.
Funding:None.
Ethical approval:The ethics committee of our center approved the study protocol.
Conflicts of interests:The authors declare that they have no competing interests.
Contributors:All authors have substantial contributions to the acquisition, analysis, or interpretation of data for the work. All authors read and approved the final version of the submitted manuscript.
 World journal of emergency medicine2021年2期
World journal of emergency medicine2021年2期
- World journal of emergency medicine的其它文章
- World Journal of Emergency Medicine
- Overlapping public health crises during the coronavirus disease pandemic
- Comparison of intraosseous access and central venous catheterization in Chinese adult emergency patients: A prospective, multicenter, and randomized study
- Empyema associated with vegetable foreign body aspiration
- A red herring: An unusual case of pneumothorax
- Detection of adrenal mass during an educational point-of-care ultrasound in the emergency department
