Myeloid-derived suppressor cells in gastrointestinal cancers:A systemic review
Maham Farshidpour,Monjur Ahmed,Shilpa Junna,Juanita L Merchant
Maham Farshidpour,Inpatient Medicine,Banner University of Medical Center,Tucson,AZ 85724,United States
Monjur Ahmed,Division of Gastroenterology and Hepatology,Department of Internal Medicine,Thomas Jefferson University,Philadelphia,PA 19107,United States
Shilpa Junna,Juanita L Merchant,Division of Gastroenterology and Hepatology,Banner University of Medical Center,Tucson,AZ 85724,United States
Abstract Gastrointestinal (GI) cancers are one of the most common malignancies worldwide,with high rates of morbidity and mortality.Myeloid-derived suppressor cells (MDSCs) are major components of the tumor microenvironment(TME).MDSCs facilitate the transformation of premalignant cells and play roles in tumor growth and metastasis.Moreover,in patients with GI malignancies,MDSCs can lead to the suppression of T cells and natural killer cells.Accordingly,a better understanding of the role and mechanism of action of MDSCs in the TME will aid in the development of novel immune-targeted therapies.
Key Words:Myeloid-derived suppressor cells;Gastrointestinal cancers;Immune checkpoint inhibitors;Tumor progression
INTRODUCTION
In 2018,4.8 million new diagnoses of gastrointestinal (GI) cancer and 3.4 million related deaths were reported globally.The incidence of GI cancer is 26% worldwide,accounting for 35% of all cancer-associated mortalities[1].Numerous stromal and immune cells and soluble markers are related to the immunosuppressive network in the tumor microenvironment (TME)[2].This network is involved in tumor cell growth and the blockade of anti-tumor immune responses,which subsequently promote the progression and invasion of tumor cells[3].Macrophages,monocytes,and dendritic cells (DCs) represent a subgroup of leukocytes called myeloid cells,which are generated from polymorphonuclear granulocytes[4].Myeloid-derived suppressor cells(MDSCs) are a heterogeneous population of immature myeloid cells that arise from myeloid progenitor cells[5].They play a key role in tumor-associated immune evasion,angiogenesis,and tumor metastasis[6,7].
In patients with cancer,the levels of MDSCs are thought to have prognostic and predictive significance[3].Recent studies have examined the role of MDSCs in solid tumors,and discovered that they appear to be independent prognostic factors in GI cancer[8,9].In a meta-analysis of 17 studies with 1115 patients with GI malignancies,patients with a higher number of MDSCs at tumor sites and peripheral blood had higher mortality rates (hazard ratio:3.35,95% confidence interval:1.46-7.68;P=0.0004),risk of relapse,and tumor progression.The authors concluded that MDSC levels have prognostic and predictive value in cancer patients[10].Additionally,higher levels of MDSCs in patients with cancer are associated with advanced tumor stage and a poor clinical prognosis[11].Shibataet al[12]evaluated 123 patients with advanced GI malignancy,including 62 with colorectal cancer (CRC),43 with gastric cancer (GC),and 18 with esophageal malignancies,and found that overall survival (OS) was significantly shorter in stage IV GI cancer patients with high MDSC levels than in those with low MDSC levels (P<0.05).Because MDSCs have a significant role in modulating cancer progression and metastasis by inhibiting the anti-tumor reactivity of T cells and natural killer (NK) cells,targeting MDSCs with immune checkpoint inhibitors (ICIs) can alleviate their pro-tumorigenic functions.Therefore,in this systematic review,we summarize the characteristics and proposed function of MDSCs in the TME and their relationship to prognosis in patients with GI cancers.
MATERIALS AND METHODS
PubMed/MEDLINE databases were explored with search strategies using search keywords “MDSCs,” “gastrointestinal cancers,” “prognosis,” “tumor progression,”and “mortality rate,” to categorize studies published between 2006 and 2020.A total of 128 articles were reviewed by the authors for relevance to MDSCs and GI cancers,including retrospective,cross-sectional,case reports,and cohort studies,of which 85 papers were selected that met our selection criteria.
MDSC MECHANISM OF ACTION
MDSCs are myeloid-derived heterogeneous cells with potent immune regulatory functions.They are derived from the myeloid lineage of immune cells that give rise to macrophages,granulocytes,and immature DCs[13].Monocytic MDSCs (M-MDSCs) and polymorphonuclear MDSCs (PMN-MDSCs) are the two major myeloid subsets of MDSCs[14].Phenotypically and morphologically,they are equivalent to monocytes and neutrophils,respectively (Table 1)[15].
The process of myelopoiesis is driven by granulocyte-macrophage colonystimulating factor (GM-CSF) in normal physiological conditions.Ultimately,GM-CSF and M-CSF induce the differentiation of granulocytes and macrophages from a common myeloid precursor that transforms into a common myeloblast[16].Myeloid DCs eventually arise from monocytic as opposed to granulocytic lineages[17].However,the hypersecretion of these mediator factors during chronic inflammation and cancer leads to the generation of MDSCs[18].For example,inflammatory cytokines such as interleukin 6 (IL-6),IL-1β,and IL-3 and C-X-C chemokine receptor type 4 (CXCR4) and CXCL12 can lead to the induction and proliferation of MDSCs in peripheral blood and tumor sites in cancer patients[7,19].The most important function of MDSCs is immunosuppression,mainly of target T cells (Figure 1)[14].
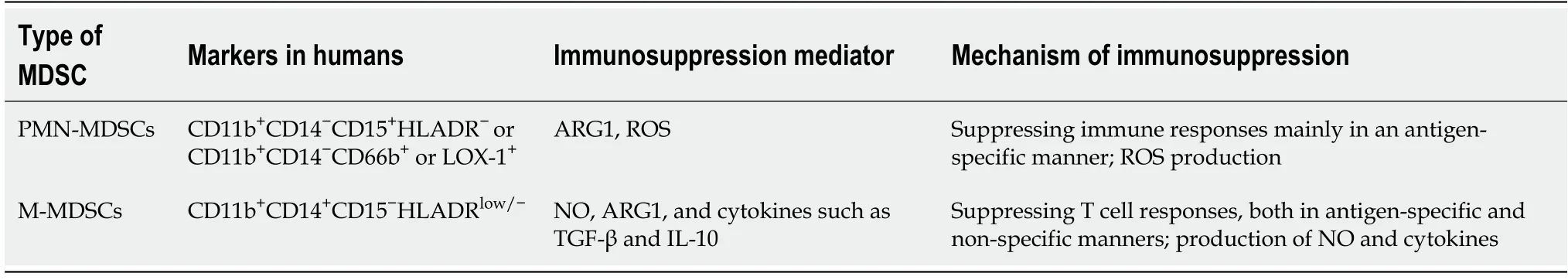
Table 1 Two main categories of myeloid-derived suppressor cells and their immunosuppressive functions[59]
Severalin vitroandin vivostudies have documented the mechanisms underlying the immunosuppressive actions of MDSCs.Arginase 1 (ARG1),inducible nitric oxide(iNOS),reactive oxygen species,and reactive nitrogen species are important suppressive factors produced by MDSCs[20,21].Caoet al[22]reported that PMN-MDSCs store ARG1 and secrete it to the TME.ARG1 and NOS activities lead to cellular depletion of L-arginine (referred to as L-arg),which is an essential substrate for T cell proliferation[22,23].Similar to T cells,depletion of L-arg also impairs the function of NK cells[24].
In addition to immunosuppressive factors,MDSCs can overpower T cell functions by directly engaging with T cell inhibitory and apoptotic receptors.Activated MDSCs express high levels of Fas ligand (referred to as Fas L),programmed death-ligand 1(PD-L1),and galectin-9.Subsequently,the interaction between these ligands with their receptors on T cells leads to T cell exhaustionviaPD-L1/programmed cell death protein 1 (PD-1) or T cell apoptosis through the Fas L/Fas and galectin-9/T cell immunoglobulin and mucin domain-3 pathways[25].Generally,M-MDSCs have more suppressive effects than PMN-MDSCs[26].Moreover,MDSCs can stimulate and recruit regulatory T cells (Tregs) to the TME[27].Tregs suppress anti-tumor immunity,and the interaction between MDSCs and Tregs create a strong blockade preventing cytotoxic immune cells from mounting an anti-tumor attack[28].Elevated levels of Tregs are associated with poor survival in patients with hepatocellular carcinoma (HCC) and pancreatic cancer[29,30].Regarding metastasis,MDSCs can promote angiogenesis by secreting IL-28 [interferon lambda (IFN-λ)] and matrix metalloproteinase (MMP)-9,promoting the invasion and migration of tumor cells[31].
MARKERS OF MDSCS IN PERIPHERAL BLOOD
MDSCs are categorized according to their phenotype,which includes several recognized surface markers,such as cluster of differentiation 33 (CD33),CD11b,or human leukocyte antigen-DR isotype (HLA-DR),as well as by the lack of expression of markers distinctive of mature lymphoid cells,such as CD3,CD19,and CD56[32].Typically,flow cytometry is performed to isolate MDSCs from peripheral mononuclear blood cells (PBMCs)[33].Fluorescent-labeled monoclonal antibodies are used to distinguish M-MDSCs and granulocytic MDSCs (G-MDSCs).M-MDSCs are identified as CD11b+CD14+CD33highHLA-DR-/lowand CD66b,whereas G-MDSCs are recognized as CD11b+CD14-CD33lowHLA-DR-CD66b+[34].MDSCs can be distinguished from other immune suppressor cells within the myeloid lineage,e.g.,tumor-associated macrophages and macrophage type 2,by other specific surface markers,including CD163 and F4/80[35].
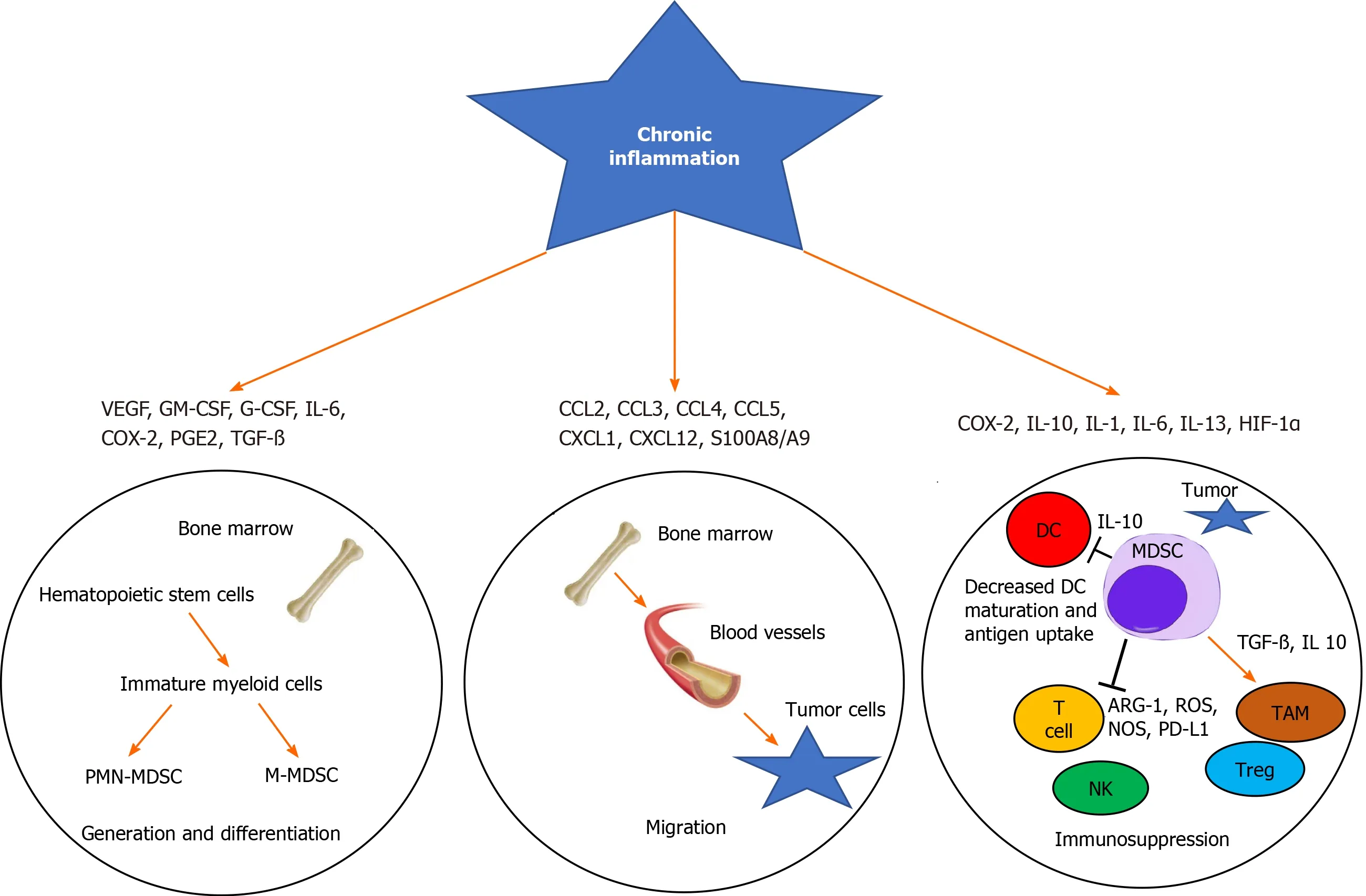
Figure 1 Chronic inflammation activates myeloid-derived suppressor cell generation,migration,and immunosuppression in the tumor microenvironment.
MDSCS IN GI MALIGNANCIES
Esophageal cancer
High levels of circulating MDSCs in esophageal cancer are associated with a poor prognosis[5].Elevated MDSCs in the blood are correlated with elevated numbers of immunosuppressive cells,including Tregs[5].Jiaoet al[36]evaluated 31 esophageal cancer patients and 26 healthy controls (HCs),and found that MDSC numbers in the peripheral blood were increased 15-fold in esophageal cancer patients compared to HCs.The authors also showed that the plasma levels of ARG1 were 3-fold higher in cancer patients than in HCs.Xuet al[37]showed that 178 patients with esophageal cancer had a high level of G-MDSCs (>82.5%),which were correlated with high morbidity due to the development of sepsis postoperatively after esophageal cancer surgery.The authors suggested that the level of G-MDSCs may be used to determine the incidence of sepsis in preoperative esophageal cancer patients postoperatively,and could improve the mortality of cancer-associated sepsis by targeting the level of MDSCs.
Additionally,a study by Chenet al[38]found that the levels of IL-6 and MDSCs predicted the prognosis and treatment response in mice with esophageal squamous cell carcinoma (SCC).The levels of MDSCs induced by IL-6 were linked to tumor growth and a poor prognosis.The authors concluded that targeted therapy against IL-6 with rapamycin or casein kinase 2 inhibitors might be a potential treatment modality for esophageal SCC[38,39].
GC
According to the Global Cancer Observatory (GLOBOCAN) 2018 database,GC is the fifth most common cancer and third most deadly cancer worldwide,with an estimated 783000 deaths in 2018[40].Liet al[41]documented the levels of MDSCs in the peripheral blood of 21 GC patients who had not previously received treatment,and noted that the levels of MDSCs in these patients were about 4-fold higher than in the control groups.The authors concluded that cancer cell differentiation and lymph node metastasis are mostly related to the presence of M-MDSCs.They also showed that treatment with epirubicin and paclitaxel regimens can reduce the level of MDSCs in these patients,potentially leading to better outcomes for patients due to inhibition of cancer progression.Moreover,in 29 patients with GC and 18 HCs,MDSCs were increased in stage IV patients compared with HCs,and the 2-year survival rate of patients with higher levels of MDSCs was significantly poorer (median OS:498 dvs473 d;P=0.048),but no significant difference was observed in survival among patients with stage I,II,and III GC[42].Previously,we reported that schlafen (SLFN) 4-expressing myeloid cells recruited to the stomach duringHelicobacterinfection undergo a phenotypic shift to G-MDSCs under the influence of damage-associated molecular pattern (DAMP) signaling and the production of IFN-α[43,44].SLFN4 is a myeloid cell differentiation factor that controls myelopoiesis[45].These SLFN-expressing MDSCs secrete factors including microRNAs,which can be detected in the peripheral blood as a biomarker and promote epithelial cell growth.This sustained immune dysregulation creates a microenvironment capable of supporting GC development[46].
HCC
HCC is a leading cause of death in cirrhotic patients.Per the GLOBOCAN 2018 database,841000 new cases of primary liver cancer and 782000 deaths due to HCC occurred that year[40].In a prospective case-control study,Elwanet al[47]demonstrated a higher number of MDSCs in the peripheral blood of cirrhotic groups without HCC than in patients with cirrhosis and HCC compared to patients in control groups.They showed that mean MDSC counts in the peripheral blood of cirrhotics without HCC group and cirrhotics with HCC group were about 3.5-fold and 5-fold higher compared to the control groups,respectively.Although not statistically significant,the authors reported a low number of MDSCs in the ascitic fluid of patients with both cirrhosis and HCC.Additionally,they investigated the correlation of levels of IFN-γ and alphafetoprotein with MDSC level.Their data showed that alpha-fetoprotein was positively and INF-γ was negatively correlated with MDSC count in the HCC group[47].A high frequency of MDSCs in the PBMCs of patients with HCC has been linked to more aggressive forms of HCC and poor clinical outcomes following local ablation,hepatectomy,or hepatic arterial infusion chemotherapy[48,49].A cohort study by Bayiket al[50]showed an upsurge in circulating MDSC frequency in 114 patients with a secondary liver cancer,including CRC with liver metastases and neuroendocrine tumors,compared to individuals with benign lesions.
Data from animal models have shown that myeloid cells secrete MMPs,serine proteases,and cysteine cathepsins,which facilitate tumor cell invasion and metastasis by disrupting cell adhesions[51].Tumor angiogenesis in HCC can be promoted by MDSCs by producing high levels of MMP-9 in HCC[52].
Pancreatic cancer
The incidence of pancreatic ductal adenocarcinoma has significantly increased worldwide over the last 30 years,with a 5-year survival time less than 8%[53].Khaledet al[54]demonstrated that G-MDSCs,but not M-MDSCs,are much higher in circulation and in the tumor tissue of patients with pancreatic cancer compared to HCs or those with chronic pancreatitis.These results suggest that the high level of G-MDSCs in pancreatic cancer plays a key factor in tumor development and progression.A cohort study reported that the percentages of all subpopulations of MDSCs were higher in patients with intraductal papillary mucinous neoplasm (IPMN) than in HCs,and were even higher in those with pancreatic adenocarcinoma.Although there was a trend towards higher MDSC levels in pancreatic cancervsIPMN,it was not statistically significant (P=0.33)[55].
CRC
A recent study reported that CRC cells induce an increase in the number of MDSCs by producing inflammatory factors,such as transforming growth factor-beta,IL-10,and ARG1[56,57].Consequently,T cell proliferation can be suppressed by tumor-derived MDSCs and promote tumor cell growthviaoxidative metabolism.Previously,it was shown that the numbers of circulating Tregs and MDSCs are significantly reduced following tumor resection in patients with CRC.These data indicate that immunosuppression can be mitigated by reducing the number of MDSCs and Tregs in patients with CRC after reducing the tumor burden[57].Tadaet al[58]showed that patients with unresectable metastatic CRC with high M-MDSC,low CD4+,or low CD8+effector memory T cell levels had significantly shorter progression-free survival.
MDSC-TARGETED THERAPY
Many studies have examined MDSCs as the core of targeted therapeutic strategies to improve tumor control in experimental animal models.These targeted therapies could be achieved by reducing MDSC numbers,hindering their trafficking and migration,or inhibiting their immunosuppressive function (Table 2)[59].
Because of variances in immunophenotype and mechanisms of suppression in the TME and diverse nature of human MDSCs,it is challenging to target human MDSCs[60].Wanget al[61]treated pancreatic cancer patients with cytokine-induced killer(CIK) cell immunotherapy,CIK plus gemcitabine,and 5-fluorouracil (5-FU),and analyzed the levels of MDSCs in the peripheral blood pre- and post-treatment.The OS of metastatic pancreatic patients was increased with the combination of CIK and chemotherapy (gemcitabine and 5-FU) compared to patients treated with only CIK.Also,Jianget al[62]reported that the quality of life and 2-year survival rate improved in patients with advanced GC following combining chemotherapy (5-FU and oxaliplatin)with CIK cell treatment compared to treatment with chemotherapy alone.Tadalafil,the Federal Drug Administration-approved phosphodiesterase-5 inhibitor,can suppress MDSCs through downregulation of ARG1 and iNOS activities in several preclinical models[63-65].Rawatet al[66]showed in aflatoxin-induced HCC rats,that tadalafil reduced the level of glutamic oxaloacetic transaminase,an important enzyme that facilitates carbohydrate and protein metabolism in cancer cells.A previous study showed that treatment with tyrosine kinase inhibitors,such as sunitinib,reduced the number of MDSCs and Tregs in animals with intrahepatic colorectal metastases[67].The authors also showed that the number of MDSCs was significantly reduced from 53.9%in phosphate-buffered saline-treated mice to 39% in sunitinib-treated mice.Sunitinib has established efficacy against advanced GI stromal tumors[68].
Treatment of esophageal SCC with 1α,25-dihydroxyvitamin D3 (calcitriol) has been shown to inhibit MDSC proliferation induced by IL-6 stimulation in C57 mice.Therefore,it has been proposed that this treatment may be a promising strategy for the prevention and treatment of esophageal SCC[69].
ICIs such as cytotoxic T-lymphocyte-associated protein 4 (ipilimumab and tremelimumab),PD-1 (pembrolizumab and nivolumab),and PD-L1 (atezolizumab,avelumab,and durvalumab) are promising treatment strategies that can be applied across numerous solid tumors[70].Pembrolizumab is a therapeutic antibody that blocks PD-1,and has shown promising anti-tumor activity in advanced GC[71].Although ICIs show great therapeutic benefits,substantial GI side effects such as colitis and GI bleeding can limit their use[72].However,due to immunosuppression,which is regulated by MDSCs,some patients with cancer may develop resistance to ICIs[73].Therefore,it is important to inhibit MDSC proliferation and migration to the TME by different strategies,such as anti-CXCR2 monoclonal antibody,to enhance PD-1 efficacy[74].
CORONAVIRUS-19 AND MDSCS
In this age of coronavirus-19 (COVID-19),we would be remiss not to address what is currently known about activation of the host’s immune response,in particular MDSCs,by severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2).Plasmacytoid DCs(pDCs) are the major source of tissue-derived type 1 IFNs in response to tissue antigens and activation of DAMPs.Typically,intracellular Toll-like receptors (TLRs)found on endosomes that mediate this pathway evolve to defend the cell against viral pathogens[75].Thus,we queried whether coronavirus infections might be modulated by pDCs residing in the GI tract.Apparently,SARS-CoV-2 induces a massive anti-viral response by secretion of IFN-α from pDCsviaTLR7[76].The severity of COVID-19 infection might correlate with the activation of endosomal TLRs on pDCs in the GI tract and increased myeloid cell polarization to MDSCs.If this occurs,the cellular immune response to the virus could be rendered ineffective,suggesting that those with severe disease exhibit higher levels of MDSCs than those with mild disease.Indeed,the limited studies available of COVID-19 patients have shown that the MDSC population expands in those with severe disease[77,78].Although T cell exhaustion from the cytokine storm that COVID-19 patients display is the leading cause for severe disease,massive production of immune suppressor cells also explains the lymphopenia occurring in many of these patients[79,80].A better understanding of what controls MDSCs will facilitate not only therapeutic treatments but may ultimately help to predict who will respond to vaccination.Whether patients who recover from these infections are predisposed to chronic disorders,such as autoimmune diseases and cancer,will require long-term follow up of these patients over decades.

Table 2 Potential therapeutic strategy for targeting myeloid-derived suppressor cells
CONCLUSION
This review article provides a better understanding of the role and mechanism of action of MDSCs in GI malignancies.MDSCs are one of the most important elements in the TME.In patients with GI cancer,MDSCs can lead to immunosuppression,and they play an important role in premalignant cell transformation,tumor growth,and metastasis.A higher number of MDSCs at tumor sites and peripheral blood is correlated with higher mortality rates,risk of relapse,and tumor progression.Therefore,monitoring circulating MDSC levels might have prognostic and predictive value in patients with GI malignancies.The benefit of targeting treatment against MDSCs as a combination therapy has been shown.Consequently,a better comprehension of the role and mechanism of action of MDSCs in the TME may aid in the development of novel immune-targeted therapies.Further prospective studies are needed to understand the characterization and clinical value of MDSCs and more selective anti-MDSC therapies with improved therapeutic outcomes.
 World Journal of Gastrointestinal Oncology2021年1期
World Journal of Gastrointestinal Oncology2021年1期
- World Journal of Gastrointestinal Oncology的其它文章
- Internal hemorrhoid harboring adenocarcinoma:A case report
- Efficacy and safety of intraoperative radiotherapy in rectal cancer:A systematic review and meta-analysis
- Diagnostic performance of narrow-band imaging international colorectal endoscopic and Japanese narrow-band imaging expert team classification systems for colorectal cancer and precancerous lesions
- Mining The Cancer Genome Atlas database for tumor mutation burden and its clinical implications in gastric cancer
- Survival outcomes and prognostic indicators for gastric cancer patients with positive peritoneal wash cytology but no peritoneal metastasis after radical gastrectomy
- Laparoscopy-assisted transanal total mesorectal excision for lower rectal cancer:A feasible and innovative technique
