Vedolizumab in Crohn’s disease with rectal fistulas and presacral abscess: A case report
Heng Yeh, Chia-Jung Kuo, Ren-Chin Wu, Chien-Ming Chen, Wen-Sy Tsai, Ming-Yao Su, Cheng-Tang Chiu,Puo-Hsien Le
Abstract
Key Words: Vedolizumab; Crohn's disease; Rectoprostatic fistula; Rectal pre-sacral fistula; Pre-sacral abscess; Case report
INTRODUCTION
Fistula affects up to 50% Crohn’s disease (CD) patients within 20 years of initial diagnosis[1,2]. It includes perianal, rectovaginal, enterocutaneous and internal fistula, but no rectoprostatic fistula or rectopresacral fistula were reported. The treatment of fistula usually requires a combination of medical and surgical approach[3]. As far as medical treatment is concerned, tumor necrosis factor (TNF) antagonists are most effective to treat fistulizing CD[4]. However, some studies also noted the beneficial effect of vedolizumab for fistulizing CD[5,6]. We presented the patient of CD, complicated with rectoprostatic fistula, rectopresacral fistula and presacral abscess. He had complete fistula closure and deep remission after transverse colostomy and vedolizumab treatment for six months.
CASE PRESENTATION
Chief complaints
Low abdominal pain and intermittent bloody stool for 6 mo.
History of present illness
A 47-year-old man has decompensated liver cirrhosis, child B, hepatitis C virus (HCV) and alcoholism related, complicated with hypoalbuminemia, hyperbilirubinemia, coagulopathy, thrombocytopenia, splenomegaly and esophageal varices, Form 1. He complained low abdominal pain and intermittent bloody stool for 6 mo. Appendicitis was diagnosed in local hospital, and he received appendectomy on 16thNovember 2019. However, he suffered from progressive low abdominal pain, bloody stool, dizziness, and intermittent fever up to 38 °C for four days. He also mentioned body weight loss 20 kg within one year. He was brought to our emergent department.
History of past illness
Decompensated liver cirrhosis, child B, hepatitis C virus infection and alcoholism.
Personal and family history
Appendicitis was diagnosed in local hospital, and he received appendectomy on 16thNovember 2019.
Laboratory examinations
Lab data revealed hemoglobin 10.1 g/dL, platelet 66000/μL, white blood cell 7700/μL, segment 68.7%, lymphocyte 23.7%, international normalized ratio (INR) 1.5, aspartate aminotransferase (AST) 55 U/L, alanine aminotransferase (ALT) 95 U/L, total bilirubin 2.1 mg/dL, albumin 2.38 g/dL and CRP 22.81 mg/L. Cytomegalovirus (CMV) immunoglobulin (Ig) M, CMV DNA, Epstein-Barr virus (EBV)-VCA IgM, EBV DNA, human immunodeficiency virus (HIV) antibody (Ab), amebic Ab, Clostridium difficile toxin, culture forSalmonella,ShigellaandCampylobacterwere all negative. Positive CMV IgG, EBV-VCA IgG, stool pus stool and occult blood were noted.
Imaging examinations
Colonoscopy showed terminal ileal shallow ulcer (Figure 1A) and multiple complex rectal fistula tracts (Figure 1B and C) on 10thDecember 2019. Magnetic resonance imaging (MRI) noted decompensated liver cirrhosis with ascites (Figure 2A), rectoprostatic fistula (Figure 2B), rectopresacral fistula (Figure 2C) and pre-sacral abscess (Figure 2D) on 21thDecember 2019. Pathology revealed acute on chronic inflammation with granulation tissue, compactable with CD (Figure 3A). Besides, there was positive result of CMV immunohistochemistry (IHC) staining (Figure 3B), which was performed with a monoclonal antibody directed against the CMV pp65 antigen (Novocastra™ lyophilized mouse monoclonal antibody; Leica Microsystems, Wetzlar, Germany).
FINAL DIAGNOSIS
He was diagnosed to have CD and CMV colitis by endoscopy and pathological findings. The CD activity index (CDAI) was 526 points and Harvey-Bradshaw index (HBI) was 22 points. He also had rectoprostatic fistula, rectopresacral fistula and presacral abscess diagnosed by MRI findings.
TREATMENT
He refused percutaneous abscess fine needle aspiration, and we kept Tazocin for abscess treatment for 27 d. Because of positive CMV IHC staining result, he also received intravenous ganciclovir for 17 d and then valganciclovir po treatment for two months. Transverse colostomy was performed for stool diversion on 25thDecember 2019. He couldn’t tolerant azathioprine due to pancytopenia and vedolizumab (300 mg 8 wk) was prescript since 22thJanuary 2020.
OUTCOME AND FOLLOW-UP
Follow-up sigmoidoscopy showed mucosal healing without any fistula tract (Figure 1D) on 9thJuly 2020. The pathologist reported minimal inflammatory activity (Figure 3C). Lower gastrointestinal series mentioned no more fistula tract (Figure 4) on 21thJuly 2020. There was no more rectoprostatic or rectopresacral fistula (Figure 5A) and pre-sacral abscess (Figure 5B) in MRI. After vedolizumab treatment for 6 mo, the CDAI was 42 points and HBI score was 0 point. His body weight body also increased 20 kg, back to the same level before the episode.
DISCUSSION
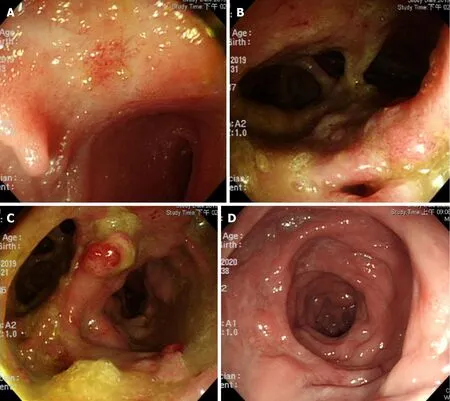
Figure 1 Endoscopic findings. A: Terminal ileal shallow ulcer at diagnosis; B and C: Multiple rectal fistula tracts with inflammation; D: Mucosal healing without fistula tracts six months after vedolizumab treatment, severe months after diagnosis.
Fistulizing CD results in not only high morbidity but also impaired health-related quality of life[4]. Biologics combined with surgical intervention seems to be the best resolution. Although Infliximab has strongest evidence in fistulizing CD treatment[7,8], vedolizumab also showed its efficacy in some studies[5,6]. However, vedolizumab has better safety profiles (less severe adverse events and infections) in real world studies[9,10].
Intra-abdominal abscess occurs in up to 20% of patients with CD[11,12]. Adequate percutaneous drainage combined with early adalimumab treatment achieves up to 74% successful rate[13]. In this case, it was difficult to drain the presacral abscess and patient refused, too. Therefore, we chose vedolizumab with transverse colostomy in treating the complex rectal fistula and presacral abscess without abscess drainage.
This patient received vedolizumab treatment one month after confirmed the diagnosis. Earlier initiation of biological treatment shortly after diagnosis (less than one year) in patients with moderately to severely active CD leads to improved longterm clinical outcomes[14]. Besides, early stool diversion with transverse colectomy and early anti-viral treatment for CMV infection were crucial to achieve the good outcome in this case.
CONCLUSION
Vedolizumab with loop transverse colostomy was effective in treating CD with complex rectal fistulas with pre-sacral abscess. Besides, early biological and anti-CMV treatments might also lead to the favorable outcome.

Figure 2 Magnetic resonance imaging at diagnosis. A-D: Liver cirrhosis (A) with ascites rectoprostaticfistula (B) rectopresacral fistula (C) with abscess presacral abscess (D).

Figure 3 Patholog. A: Ulcer with acute on chronic inflammation and granulation tissue at diagnosis; B: Pathological presentations of cytomegalovirus (CMV) infection, immunohistochemistry stain (20 × objective) was performed with 1:200 diluted Novocastra™ lyophilized mouse monoclonal antibody against CMV pp65 antigen and showed strong focal CMV immunoreactivity with brownish areas; C: Minimal inflammatory cells infiltration six months after vedolizumab treatment, severe months after diagnosis.

Figure 4 Lower gastrointestinal series showed no more rectal fistula tract.
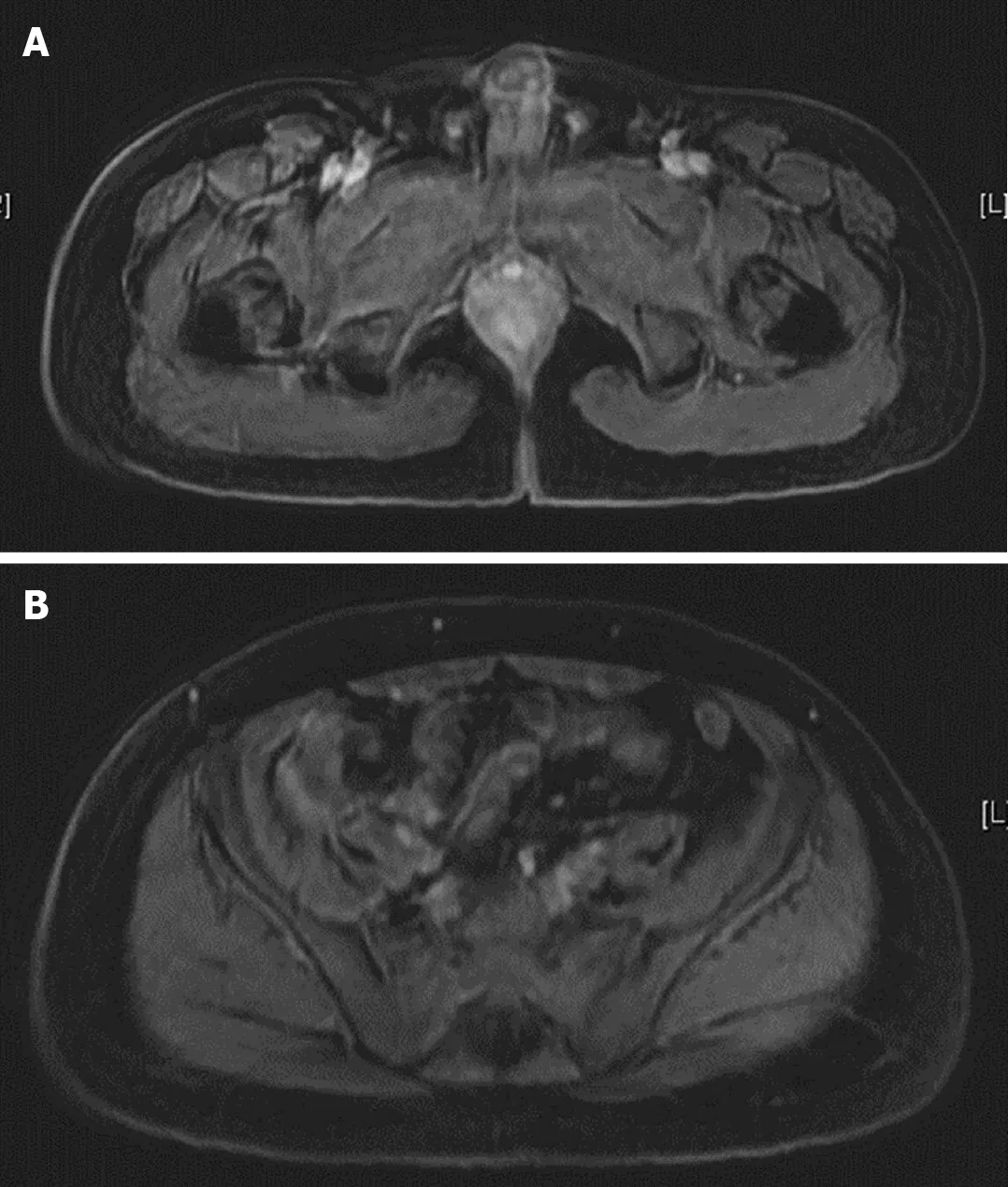
Figure 5 Magnetic resonance imaging seven months after diagnosis. A: No more rectal fistula tract; B: No more pre-sacral abscess.
 World Journal of Gastroenterology2021年5期
World Journal of Gastroenterology2021年5期
- World Journal of Gastroenterology的其它文章
- Liver injury in the era of COVID-19
- Changes in gut microbiota composition and diversity associated with post-cholecystectomy diarrhea
- Histopathology and the predominantly progressive, indeterminate and predominately regressive score in hepatitis C virus patients after direct-acting antivirals therapy
- Comparative study of indocyanine green-R15, Child-Pugh score, and model for end-stage liver disease score for prediction of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt
