Exertional heat illness risk factors and physiological responses of youth football playersT
Susn W.Yrgin*,John J.Dickinsonb,Dwn M.Emrsonc,Jssic Kollrd,Toni M.Torrs-McGhZchry Y.KrrT
aDepartment of Exercise Science,University of South Carolina,Columbia,SC 29208,USA
bPalmetto Health/USC Orthopedic Center,Keenan High School,Columbia,SC 29203,USA
cDepartment of Health,Sport,and Exercise Sciences,University of Kansas,Lawrence,KS 66045,USA
dSurgi-Care Inc.,Boston,MA 02115,USA
eDepartment of Exercise and Sport Science,University of North Carolina,Chapel Hill,NC 27599-8700,USA T
Received 8 June 2018;revised 7 September 2018;accepted 9 October 2018 Available online 7 March 2019
2095-2546/©2021 Published by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/)
Abstract Objective:To determine which intrinsic and extrinsic exertional heat illness(EHI)risk factors exist in youth American football players and observe perceptual and physiological responses of players during events(games and practices).Methods:Cross-sectional cohort study observing 63 youth football players,varying in position.Independent variables were league(weightrestricted(WR,n=27)and age-restricted(AR,n=36))and event type.Dependent variables were anthropometrics,work-to-rest ratio,and wet bulb globe temperature.Descriptive variables included preparticipation examination and uniform con figuration.A subset of 16 players participated in physiological variables(heart rate and gastrointestinal temperature).Data collection occurred on 7 AR and 8 WR nonconsecutive practices and the first 3 games of the season.Results:Mean values for anthropometric variables were higher(p<0.05)in the AR league than the WR league.Work time(x2(1,111)=4.232;p=0.039)and rest time(x2(1,111)=43.41;p<0.001)were significantly greater for games,but ratios were significantly higher for practices(x2(1,111)=40.62;p<0.001).The majority of events(77%)observed were in black and red flag wet bulb globe temperature risk categories.A total of 57%of the players had a preparticipation examination,and up to 82%of events observed were in full uniforms.Individual gastrointestinal temperature and heart rate responses ranged widely and no players reached critical thresholds.Conclusion:Extrinsic(disproportionate work ratios,environmental conditions)and intrinsic(higher body mass index)EHI risk factors exist in youth football.Certain risk factors may be in fluenced by event and league type.National youth football organizations need to create thorough guidelines that address EHI risk factors for local leagues to adopt.
Keywords:Adolescents;Anthropometrics;Core temperature;Heat exchange;Pediatric;Wet bulb globe temperature
1.Introduction
In the past decade,the diagnosis of exertional heat illness(EHI)has increased in athletes,as well as the number of conf i rmed deaths from EHI.1-3Youth and adolescent(<19 years of age)male athletes participating in American football compose the majority of EHI cases that present to emergency rooms.4Recent research reveals that youth football has the highest EHI rate compared with high school and college teams.5Epidemiological research indicates that youth football players sustain EHI at a rate of 1.82 per 10,000 athlete exposures.5Emergency department data reported approximately 1000 EHI cases sustained per year in football players younger than 19 years of age in a sample from the National Electronic Injury Surveillance System.4EHI rates are highest in the preseason regardless of competitive level,5-7but differ between practices and games depending on the level.5
EHI has numerous risk factors,including lack of heat acclimatization,increased body mass index(BMI),illness,and inappropriate work-to-rest ratios.8,9More speci fically,football is an intense sport and this high exercise intensity is the largest driver of increased core body temperature.10,11Football players have additional risk factors,such as their equipment and playing in hot environmental conditions(wet bulb globe temperature(WBGT))during preseason.12-16Although there has been immense research on EHI risk factors in adults4,9,12,13,17-20and high school athletes,5,6,21-24research is lacking for youth football players.5,14Youth football players may have supplementarythermoregulatory predisposing factors25-28and team dynamics.Teams have small rosters,leading to athletes often playing both offense and defense,29which may result in uneven work-to-rest ratios.Youth football leagues vary across the country by organization structure,team demographics,and guidelines/rules.For example,some leagues create teams based on age only,whereas others are based on age plus weight.Leagues can be part of a national organization or independent and may or may not have guidelines on starting dates,practice length,or playing time.These factors in turn can significantlyimpactenvironmentalconditions players are exposed to,14as well as athlete exposures29and possibly the types of players that participate in each league.
To date,no existing literature has examined the risk factors associated with EHI in youth football players beside environmental conditions.14Describing which factors are prevalent in youth players and how their bodies respond to football events(practices and games)may improve prevention strategies and help to develop guidelines for safer participation.Therefore,the primary purpose of our study was to determine which intrinsic(anthropometrics,previous history)and extrinsic(WBGT,work-to-rest ratio)EHI risk factors exist in youth football players.The secondary purpose was to describe the perceptual responses(heat illness symptoms),maximum physiological responses(gastrointestinal temperature(TGI)and heart rate(HR))that youth football players experienced in a warm environment.
2.Methods
2.1.Design
We used a cross-sectional research design to observe youth football teams during 1 season.Data were collected from 2 types of youth football leagues(weight restricted(WR)and age restricted(AR))during 2 types of events(games and practices).Dependent variables included subjects’anthropometrics(age,height,weight,BMI category,and body surface area(BSA)),each team’s work and rest times,environmental conditions measured by WBGT,and perceptual heat illness symptoms.Physiological variables including HR and TGIwere acquired from a subgroup of participants.Additional risk factor history(preparticipation examination,previous EHI,sickle cell trait status,medications,sleep habits,signs of illness,and uniform con figuration),preseason and regular season start dates,and event times were collected for descriptive purposes.
2.2.Participants
Youth football players(n=63)from local recreational leagues in the southeastern region of the United States participated in this study.The youth players in these leagues were 13 years of age or younger and were not participating on an interscholastic team.The convenience sample was recruited during the team parent meetings for each league before the season began.There were twenty-seven of 80 participants from the WR league(34%)and thirty-six of 100 from the AR league(36%)who volunteered to participate.The WR league included participants from 4 teams of speci fic weight and age categories.Each player within this league format had to be within the weight range before the season began to be eligible for that division.Additionally,at each game,participants had to weigh in with full pads and meet requirements to play that day.The AR league had 11 teams with participants from 8 teams separated only by age ranges with no weight speci fications.There were no exclusions to participate in the study.However,for those interested in participating in the TGIportion of the study,exclusions(i.e.,less than 80 lbs)were followed per manufacturer instructions.30Of the 63 youth football players,16 participants(8 from each league)met the criteria and participated.The University of South Carolina’s Institutional Review Board approved the protocol before recruitment.An informational team meeting was held before the preseason began for each league.This meeting included describing the study and the risks involved and answering questions from the parents and athletes.Those interested in participating signed consent and assent forms.
2.3.Measurements and instrumentation
2.3.1.Risk factor history
League websites were examined to determine if preparticipation examinations were mandated.Preseason start dates,regular season start dates,practice times,and game times were also examined.The results were con firmed with the league’s director.A baseline survey asked participants to self-report any past EHI history,general sleep habits,and known sickle cell trait history.Players also completed a short survey at each observed game and practice asking about sleep(time to bed and time of waking)and general illness symptoms( flu,diarrhea,vomiting,fever,or malaise)within the last 24 h and 48 h,respectively.Researchers recorded uniform con figurations on activity logs for each practice and game(1(helmet only),2(helmet and shoulder pads),3(full uniform)).
2.3.2.Anthropometrics
Age was self-reported in whole years.Participants were weighed in shorts only on the first day of practice as a baseline measure using a digital scale(TBF-300A;Tanita,Arlington Heights,IL,USA),and height was measured using a portable stadiometer(ShorrBoard Weight and Measure,Olney,MD,USA).These variables were used to calculate BMI and then categorized(underweight,healthy,overweight,and obese)by Centers for Disease Control and Prevention delimiters.31,32BSA was calculated with the Mosteller formula.33
2.3.3.Work-to-rest ratio
In relation to EHI,work represents any activity or drill that could result in metabolic heat generation,and rest represents the opportunity to optimize heat loss.Researchers recorded the time of day each team began and ended an activity or drill(i.e.,work)on activity logs.Any time a team had a break(i.e.,rest),the beginning and ending times were recorded.Activity logs were filled out at all events(n=11).The team’s work and rest times were averaged together to represent the leagues’experience as a collective identity.A work-to-rest ratio was calculated using the number of minutes the teams engaged in work divided by the number of minutes of rest.
2.3.4.Environmental conditions
A portable WBGT device(4600 Heat Stress Meter;Kestrel Meters,Birmingham,MI,USA)was used to measure environmental conditions.The average and maximum WBGT values were analyzed to determine the typical and highest heat stresses experienced by players.24The average WBGT was calculated using all measurements obtained(1 measurement every 15 min)during all events.The maximum WBGT was derived by extracting the highest WBGT measurement recorded for that event and then averaged.Average results were compared with the American College of Sports Medicine recommendation chart to determine frequencies in each flag risk category.20The green risk category was any event played at less than 24.0˚C and the yellow category was any event played at 24.0˚C-25.9˚C.The red category events were played at 26.0˚C-29.0˚C and the black flag risk categories were any events played at more than 29.0˚C.20
2.3.5.Perceptual and physiological variables
A total of 14 selected items from an Environmental Symptoms Questionnaire(ESQ)24,34,35evaluated common EHI signs and symptoms for each event.Ingestible TGIsensors(HQ Inc.,Palmetto,FL,USA)were used to measure TGIduring selected practices(n=3)and games(n=3).30The youth ingested the sensors in the morning(approximately 6 h before the start of the event)to ensure the sensor reached the intestines.HR chest straps(Polar Electro Inc T31,Lake Success,NY,USA)were used to monitor HR simultaneously with TGI.The maximum TGIand HR were derived by extracting the highest measurement recorded for each player during each event and then averaged.
2.4.Procedures
Data collection occurred on 7 AR or 8 WR nonconsecutive practices and the first 3 games of the season for both leagues.The WR had 2 practices on Day 8.Anthropometric data and risk factor history were collected before the first day of practice.Sleep habits and general illness symptoms were collected before every practice and game.WBGT was recorded throughout each practice or game in approximately 15-min intervals.During practices and games,researchers noted the uniform con figuration and logged work and rest time intervals for each team.Immediately after each practice and game,subjects completed the ESQ.
A subset of football players(n=16)agreed to participate and completed data collection.At 3 predetermined practices and 3 games,the TGIand HR were measured.Parents were given speci fic instructions to have their youth ingested the sensor during the morning hours(i.e.,with breakfast)to ensure proper location within the intestines.On the day of the practice or game,a baseline TGIwas measured to con firm the sensor had reached the intestines(i.e.,to ensure a nonerroneous measurement).Participants were instructed to practice and play normally.During practices,TGIand HR were checked at approximately 15-to 20-min intervals throughout the 2-h practice.During games,the TGIand HR were recorded when the athlete returned to the sideline and at timeouts.
2.5.Statistical analyses
Descriptive statistics were calculated for all dependent and descriptive variables.The average and maximum WBGT were used to describe environmental conditions experienced by leagues.24Independentttests compared means between leagues for anthropometrics variables.Independentttests were also used to determine differences between leagues and events for WBGT and between events for ESQ scores.The Kruskal-Wallis test was used to compare overall work time,rest time,and ratios for each event type.Pearson’srcorrelation coef ficients were used to determine if relationships existed for HR and TGIwith work-to-rest ratio,WBGT,and BMI.Maximum physiological variables from all 16 players at each football event were used to represent thermal strain.24No statistical comparisons were made for physiological variables because the data sets were incomplete.Signi ficance was seta prioriatp=0.05.Statistical Analysis Software(Version 4.3;SAS Institute,Cary,NC,USA)was used for all analyses.
3.Results
3.1.Risk factor history
Preparticipation examination mandates,start dates,and times for practices and games differed depending on the league(Table 1).Of the 63 players participating in the study,thirty-four completed a baseline questionnaire.About onequarter(26%)reported experiencing symptoms in the heat consistent with an EHI(i.e.,struggling,faint,dizzy,nauseous,and falling down)in a previous season,but zero reported an actual previous EHI episode.When the participants were asked if they were taking a medication,29%indicated yes.There were no clari fications of medication type provided by the players.One player(3%)was sickle cell trait positive as con firmed by a parent.Players reported an average of 8.7±1.3 h of sleep on the baseline questionnaire and 9.4±0.3 h of sleep on the prepractice/pregame questionnaire.Players reported symptoms consistent with a general illness within 48 h of a practice or game 9%of the time(range:0-22%).Players in 1 league we observed in the study wore shorts and T-shirts for their first 2 practices,added helmets for the third practice,and then wore full uniforms for the remaining practices and games(72.7%).In the other league we observed,players wore helmets only for the first 2 days and then proceeded to full uniform for the remaining practices and games(82%).

Table 1 Descriptive values for anthropometrics and risk factors by league.
3.2.Anthropometrics
The overall and league demographics are provided in Table 1.Mean values for anthropometrics variables were higher(p<0.05)in the AR league than in the WR league.The BMI category percentages in the WR league were 3.7%underweight(n=1),66.7%healthy(n=18),18.5%overweight(n=5),and 11.1%obese(n=3).For the AR league,the percentages were 2.8%underweight(n=1),61.1%healthy(n=22),8.3%overweight(n=3),and 27.8%obese(n=10).
3.3.Work-to-rest ratio
The average work and rest time are provided with ratios in Table 2 by league.Work time was significantly greater for games than practices(98±18 minvs.89±25 min;x2(1,111)=4.232,p=0.039),as were rest time(29±15 minvs.9±6 min;x2(1,111)=43.41,p<0.001).However,work-to-rest ratios were significantly higher for practices((13±7):1vs.(4±1):1;x2(1,111)=40.62,p<0.001).
3.4.Environmental conditions
The maximum and average WBGT conditions are presented in Fig.1 by league and events.Of the practices and games observed(n=11)in each league,9%(n=2)were held in black flag conditions,68%(n=15)were held in red flag conditions,18%(n=4)were held in yellow flag conditions,and 5%(n=1)were held in green flag conditions,according to the American College of Sports Medicine WBGT risk table.20The average(t=0.468,p=0.641)and maximum(t=0.662,p=0.534)practice WBGT compared with game WBGT were not significantly different.However,there was a significant difference(t=4.402,p<0.001)for the WR league’s average WBGT compared with the AR league in games and all events.Upon further analysis with pairwise comparisons,the WR league’s average and maximum WBGT was significantly higher(t=11.158,p<0.001)than the AR league’s WBGT during games.There were no other significant comparisons(p>0.05).T

Table 2 Work time,rest time,and work-to-rest ratios for all youth football teams,by league and event type(mean±SD).
3.5.Perceptual and physiological responses
The average practice and game ESQ score were 8±7(0-42)and 7±8(0-30)(mean±SD(minimum-maximum)),respectively.There were no significant differences between events(t=1.121,p=0.263).During games,individual TGIand HR responses ranged from 37.5˚C to 39.3˚C and 80 bpm to 224 bpm,respectively.Practices ranged from 36.8˚C to 39.2˚C and 75 bpm to200bpm,respectively,for the same variables.Maximummeasurements for physiological variables are presentedinFig.2.There were no significant correlations between physiological variables and work-to-rest ratio,WBGT,or BMI(allp>0.05).

Fig.1.Maximum WBGT(A)and average WBGT(B)between games(n=3)and practices(n=8)for each league.Red flag(dotted line),black flag(solid line)American College of Sports Medicine recommendations.20The maximum WBGT was derived by extracting the highest WBGT measurement recorded for each event and then averaged;the average WBGT was calculated using all collected measurements for each event.*p<0.05,compared with AR league determined by independent t tests.Agg=aggregate;AR=agerestricted;WBGT=wet bulb globe temperature;WR=weight-restricted.
4.Discussion
4.1.Risk factor history
Preparticipation examinations are recommended for youth who participate in sports,36yet very few recreational youth leagues require them.One league within our study required preparticipation examinations and the other did not.Preparticipation examinations allow pediatricians to assess the youth’s medical and family history to determine if any conditions may predispose him or her to unnecessary risk during sports.36Almost one-third of our participants indicated that they were currently taking medications.Certain medications have the potential to change body temperature,9decreasing the heat storage capacity of the youth player.
A previous history of an EHI and a lack of sleep are individual risk factors that have been examined in adult populations.8,20Even though a previous history of EHI was not directly assessed in our study,participating youth did not seem to understand what constituted an EHI episode but reported symptoms alluding to previous occurrences(i.e.,struggling,faint,dizzy,nauseous,and falling down).Survey research has indicated a similar lack of knowledge among high school football players.24As previously reported,37sleep habits in our subjects were good throughout the study observation period.This EHI risk factor was not evident in our players and instead seems to manifest itself as youth enter high school.38
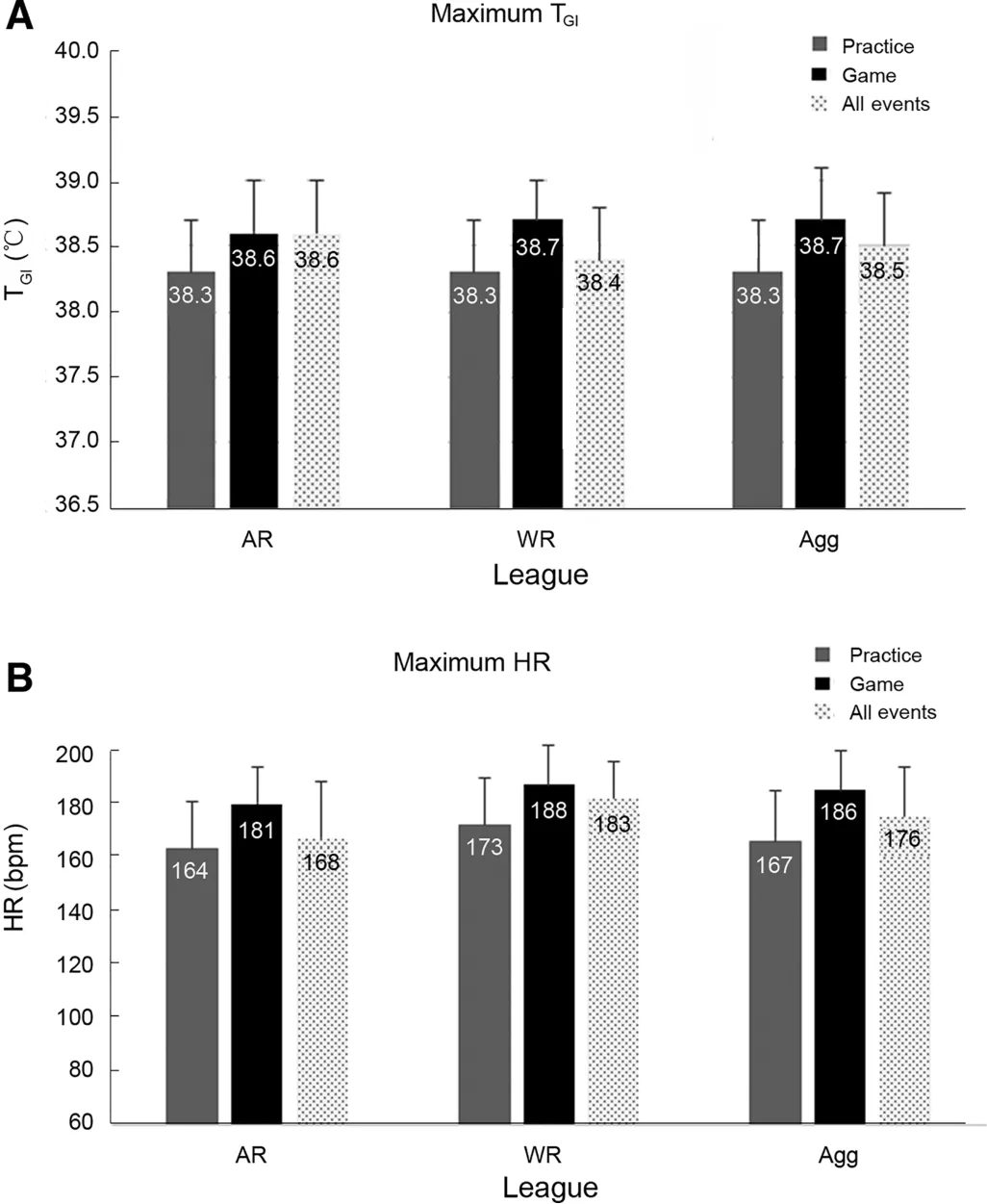
Fig.2.Maximum TGI(A)and maximum HR(B)between games(n=3)and practices(n=3)for each league.TGIand HR were derived by extracting the highest measurement recorded for each player during each event and then averaged.Agg=aggregate;AR=age-restricted;HR=heart rate;TGI=gastrointestinal temperature;WR=weight-restricted.
Uniforms are a considerable risk factor because they increase physiological strain in hot conditions during full and partial conf i gurations.15The youth teams involved in our study wore partial uniforms during the first week of practices before full pad con figurations were added at the beginning of their second week.However,both leagues approached integration differently,and full uniform con figurations were never removed after incorporation despite environmental conditions in red flag conditions(26˚C-29˚C).39Youth take longer to acclimatize to the heat.40Not allowing players to fully make adaptations before adding increased stressors(uniforms)increases EHI risk.
4.2.Anthropometrics
Anthropometric differences existed between leagues,revealing that players in the AR league were taller,heavier,and had a higher BMI and larger BSA than players in the WR league.League formation in fluences the types of players who participate,thereby impacting risk factors within a league.Larger athletes may be forced to participate in a different league or drop out owing to the dif ficulty of “making weight”for games.Nevertheless,we found some portion of players(approximately 30%)in each league who were either overweight or obese according to criteria set forth by the Centers for Disease Control and Prevention.Our proportion of players was lower than in previous research,41possibly owing to a smaller sample size.Overweight and obese categories are a risk factor that both leagues’organizations should consider when developing safety guidelines.Players with a high BMI are at risk for an EHI because of greater metabolic heat production during football.42
It is also important to remember that,although they are not inferior,prepubertal athletes thermoregulate differently than adults.28Evaporative sweat is the principal means of heat dispersal during exercise in hot climatic conditions for adults.However,prepubertal boys have a lower overall sweat rate,lower sweat output per gland,and decreased sensitivity of sweat gland output in response to a given ambient temperature.40With evaporative heat loss minimized,prepubertal boys instead rely heavily on conductive and convective heat loss mechanisms.During thermoregulation,greater BSA as compared with mass results in a greater exchange of heat.28,43Yet in hot temperatures this relationship is detrimental because the higher gradient from ambient temperature to skin reduces heat loss.28Maturational thermoregulatory differences in youth players lead to a slightly longer acclimatization process.40
4.3.Work and rest variables
Leagues had a greater work-to-rest ratio during practice compared with games.Work length,without adequate time to rest and particularly in high-intensity situations,is a primary risk factor of exertional heat stroke and exertional sickling.8,9,20Adequate rest time should be a priority for this population during practicesand games to encourage heat dissipation and provide fair playing time.An informal study of the National Football League reported an average 10:1 ratio during games,44whereas a high school scrimmage had a 6:1 ratio.45The National Football League ratio is much greater than our game data owing to inherent differences,yet the high school ratio was similar to ours.Only 1 other study has examined practice exercise and rest intervals in a football team,which was at the collegiate level.Even though it was not a primary outcome measure,a 6:1 ratio could be calculated from the data given in the study.46Our practice ratio was,surprisingly,much higher for youth football players.The difference could be explained by a more accurate assessment of intervals by global positioning system units as compared with our observational timing of the whole team,yet our data call for attention to be drawn to the youth football population.Coaching and medical staff should plan to make work-to-rest ratios during practice closer to what the youth athlete will experience during games.Appropriate ratios are especially important on days with hot environmental conditions to help decrease EHI risk in this population.14,25
4.4.Environmental conditions
Leagues in our study participated in events with stressful environmental conditions,as is typical in the southeast.Both leagues participated in games or practice during 1 black flag condition20(WBGT of>29˚C).These temperatures could primarily be attributed to the start date of practices.Practices began in early August for WR leagues,similar to colleges and high schools;this time is the hottest of the year across the nation.Research clearly indicates that the majority of EHI occurs in the summer months when the temperatures are at the highest,12,47particularly the first one-half of August.14However,owing to starting 25 days later in August,players in AR leagues experienced milder maximum WBGT conditions.Some of the more alarming temperatures were during WR games in which a maximum WBGT of 34˚C was recorded.The difference in temperatures that players in the WR and AR leagues experienced was due the time the games or practices were scheduled.The WR leagues played their games were between 9:00 a.m.and 2:00 p.m.,the hottest part of the day.14AR leagues played their games or practiced during evening hours(6:00 p.m.to 8:00 p.m.).The timing of football practices and games may play a significant role in EHI rates5and therefore should be considered when scheduling events.
4.5.Perceptual and physiological responses
Perceptual response to thermal strain(as measured by ESQ scores)did not differ between games and practices.Yet the score ranges for practice and games were both wide,with some players reporting scores upwards of 42(of a maximum of 70).These scores indicate a higher number of heat-related symptoms experienced,with greater severity.Players routinely experienced symptoms such as headaches,dizziness,nausea,and feeling hot.Other symptoms reported were thirst,tiredness,and trouble concentrating.This study was the first time an ESQ had been used in the youth football population,but the average and range of scores were similar to those of high school football players during preseason practices.24
GIs also varied widely depending on event type and the time point within the event.Of those players who participated in this portion of the study,56%(n=9)reached a TGIof 39˚C or higher at least once during the observation period,but no players reached a TGIindicative of exertional heat stroke(40.5˚C).9Previous research has examined natural fluctuations in physiological variables during football practices,16,19,24,46but not during game situations or in the youth football population.Our results can provide a descriptive foundation of responses for future research.There were no correlations between the physiological variables and environmental conditions or anthropometrics.Typically,there is a relationship with anthropometrics with TGI,with higher TGIin larger individuals,13,16,46but our sample size was small and relatively homogeneous owing to temperature sensor criteria,which may explain the lack of correlations.
4.6.Limitations
Work and rest timeswere monitored for the team as a whole and,therefore,cannot accurately represent what an individual player may have experienced.Physiological variables were measured only in a subset of players and events and,therefore,do not provide a complete picture of the thermal strain in this population.Practice times and lengths were determined by the league or the coach and,therefore,were not consistent across events.One league cannot fully represent a league type;therefore,future research should include more leagues of each type(AR and WR)to con firm the differences we found and provide the capability to expand comparisons to more variables.Recommendations(Table 3)can be made based on the dependent variables from the current study and previous literature.However,future research should also examine a greater number of players over the first 2 weeks of practices to provide better descriptions of thermal stress during the preseason in this population.

Table 3 Recommendations based on dependent variables.
5.Conclusion
Extrinsic and intrinsic EHI risk factors do exist in youth football leagues.Some leagues do not mandate a preparticipation physical,which removes the pediatrician’s ability to screen for sport-speci fic injury risk.Even at this young age,a previous history of EHI,thermoregulatory-affecting medications,and the presence of general illnesses during football are possible.Once full uniforms were integrated,they were not removed for environmental conditions.WR and AR leagues in fluence the anthropometrics of players who participate in those leagues,with overweight and obese players still being prevalent in both types.During practices,ratios indicate that players work more with little rest,which is of concern when leagues practice in hot conditions.Rest break guidelines similar to those adopted by organizations in older competitive leagues should be used by youth football coaches.Some player’s experienced TGItemperatures of greater than 39˚C,but all remained below the EHI threshold for both practices and games.National leagues need to take steps to ensure their handbooks include accurate heat safety information and comprehensive guidelines for local leagues to adopt.
Acknowledgments
We would like to acknowledge the hard work and significant time commitment of all the research assistants who helped during data collection.We would also like to thank the players and their parents for their willingness to participate in the study and patience during data collection.Last,we recognize Ross Hayden for his help with statistical analysis.This work was supported in part by the University of South Carolina’s College of Education Internal Grant Program.The study was also supported in part by the Master’s Grant program of the Datalys Center for Sports Injury Prevention and Research.Funding sources did not in fluence the study design,data collection,analysis,or writing of the manuscript.
Authors’contributions
SWY and JJD developed the research questions,study design,planned and executed data collection,aided in the statistical analysis,interpreted the analysis,and drafted the manuscript;DME,JK,and TMTM helped with study design,executed data collection,interpreted the analysis,and helped to draft the manuscript;ZYK conducted the statistical analysis,interpreted the analysis,and helped to draft the manuscript.All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
 Journal of Sport and Health Science2021年1期
Journal of Sport and Health Science2021年1期
- Journal of Sport and Health Science的其它文章
- Response to:Caution needed when interpreting muscle activity patterns during extremely low pedaling cadenceT
- Caution needed when interpreting muscle activity patterns during extremely low pedaling cadenceT
- Muscular activity patterns in 1-legged vs.2-legged pedalingT
- Cardiorespiratory and muscular fitness associations with older adolescent cognitive controlT
- A person-centered approach to achievement goal orientations in competitive tennis players:Associations with motivation and mental toughnessT
- Inter-individual differences in the responses to aerobic exercise in Alzheimer’s disease:Findings from the FIT-AD trialT
