Conversion to reverse shoulder arthroplasty fifty-one years after shoulder arthrodesis: A case report
Melissa N Dogger, Annelies F van Bemmel, Tjarco D W Alta, Arthur van Noort
Melissa N Dogger, Annelies F van Bemmel, Tjarco D W Alta, Arthur van Noort, Department of Orthopedic Surgery, Spaarne Gasthuis, Hoofddorp 2134 TM, Netherlands
Abstract
Key Words: Shoulder arthrodesis; Conversion; Reverse shoulder arthroplasty; Electromyography; Case report
INTRODUCTION
Shoulder arthrodesis is a salvage procedure for patients with shoulder dysfunction when other surgical options are limited. Indications include post-traumatic brachial plexus injuries, paralysis of the deltoid muscle and the rotator cuff, chronic infections, failed arthroplasties, and recurrent instability[1,2]. A shoulder arthrodesis may involve an acromiohumeral fusion, a glenohumeral fusion, or a combination of both[1-3]. The shoulder function of a well-positioned arthrodesis is limited and allows the patient to reach his back pocket, groin, and mouth. Generally, only scapulothoracic movements, like elevation and minimal rotations, after an arthrodesis are possible[1,2]. Most patients experience a reduction in pain but few are pain free, with up to one-third experiencing substantial peri scapular pain[1,2,4].
A treatment for a painful arthrodesis is conversion to reverse shoulder arthroplasty (RSA), which has been described as effective for pain relief and promising functional improvements[5,6]. Based on the literature review conducted by the authors of this report, only two reports were found that describe a total of five cases in which the patients received a conversion to RSA[5,6].
Here we present the case and surgical technique of a conversion from a painful shoulder arthrodesis to RSA in a 71-year-old male patient after a 51 years interval. The patient was informed that data concerning the case would be submitted for publication, and written patient consent was obtained. Table 1 outlines a timeline of the patient presentation.
CASE PRESENTATION
Chief complaints
A 71-year-old male patient presented to the orthopedics outpatient department of our hospital with complaints of severe peri scapular pain and limited shoulder function, 51 years post arthrodesis of the right shoulder.
History of present illness
Since the shoulder arthrodesis, the patient has been experiencing peri scapular pain. There was no history of new preceding trauma or injury. Pain progressed throughout the years, present at rest and with activity. Due to the limited range of shoulder motion, the patient experienced problems in activities of daily living. He was unable to reach above shoulder level and particularly the loss of internal rotation bothered him in self-care. Conservative treatment including analgesics and physical therapy was ineffective.
History of past illness
Indication for arthrodesis in the past was persistent posttraumatic posterior instability of both shoulders after failed open stabilizing procedures. In 2017, the patient was treated with a RSA on the left side because of development of a rotator cuff arthropathy. Due to a very good functional outcome of the left shoulder, he had the expressed wish for conversion of the fused right shoulder into RSA as well.
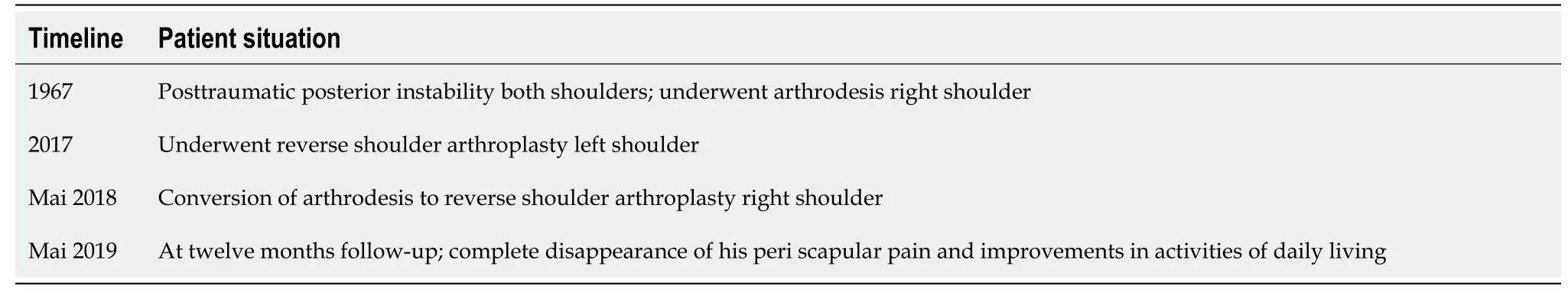
Table 1 Patient timeline
Physical examination
At physical examination the actively achieved elevation was 100º, external rotation and internal rotation to lateral side of his leg. Notable was the peri scapular pain which he experienced during physical examination. He had an Oxford Shoulder Score of 38 (the best score: 12; the lowest score: 60). Sensibility of the axillary nerve was intact and despite general atrophy of the deltoid muscle (in particular the posterior part), contraction of the deltoid muscle was still possible.
Imaging examinations
Conventional radiographs (Figure 1) and computed tomography (Figure 2) showed a shoulder arthrodesis with glenohumeral and acromiohumeral consolidation and normal bone stock of the glenoid. As part of the preoperative workup, electromyography (EMG) was performed and showed normal motor unit activity and recruitment in all three parts of the deltoid muscle.
FINAL DIAGNOSIS
Complete cessation of peri scapular pain and structural improvements in daily activity after conversion of shoulder arthrodesis to RSA, after a 51 years interval.
TREATMENT
Surgical technique
At the time of surgery, the patient had an interscalene block with general anesthesia, and was positioned semi-inclined in the beach chair position. After a stab incision the superior screw, through the acromion into the humeral head, was removed. The original anterior incision was used and a deltopectoral approach performed. The layers could nicely be mobilized without obstruction of an excessive amount of fibrosis. In contrast with a sufficient deltoid muscle (Figure 3), the quality of the rotator cuff was very poor with an absent superior cuff and a fibrotic, very thin subscapularis muscle. After removal of the screw which penetrated the formal glenohumeral joint, an osteotome was used to split the acromion from the humeral head. The “glenohumeral” osteotomy was performed under 10º of caudal inclination, a neutral version and one centimeter lateral from the original joint line, creating a longnecked scapula (Figure 4) in order to minimize scapular notching and improve rotations. An uncemented RSA (DELTA XTEND, DePuy Synthes, Raynham, Massachusetts, United States) was now implanted in a standard fashion (Figure 5).
OUTCOME AND FOLLOW-UP
Postoperatively the patient was placed in a shoulder immobilizer for 6 wk. The patient was allowed to move passively and actively guided for 6 wk direct postoperatively. The postoperative course was otherwise uneventful. At 12 mo follow-up, the patient was very happy with respect to the outcome, with complete disappearance of his peri scapular pain (visual analogue scale score 0 in rest and exercise) and structural improvements in activities of daily living like eating with knife and fork, wiping his buttocks with his right hand, carrying more heavy objects with his right hand. Nevertheless, his shoulder function was rather poor with an active forward elevation of 50º, internal rotation to Th12 and absence of external rotation (neutral position) (Figures 6-8). The deltoid muscle had an intact function in the anterior and lateral part, the posterior part was atrophic (Figure 6). He had an Oxford Shoulder Score of 23, and a Subjective Shoulder Value of 60%. Conventional radiographs showed a correct position of the RSA (Figure 5B). The patient was very satisfied with the outcome and assured the necessity of the surgery.
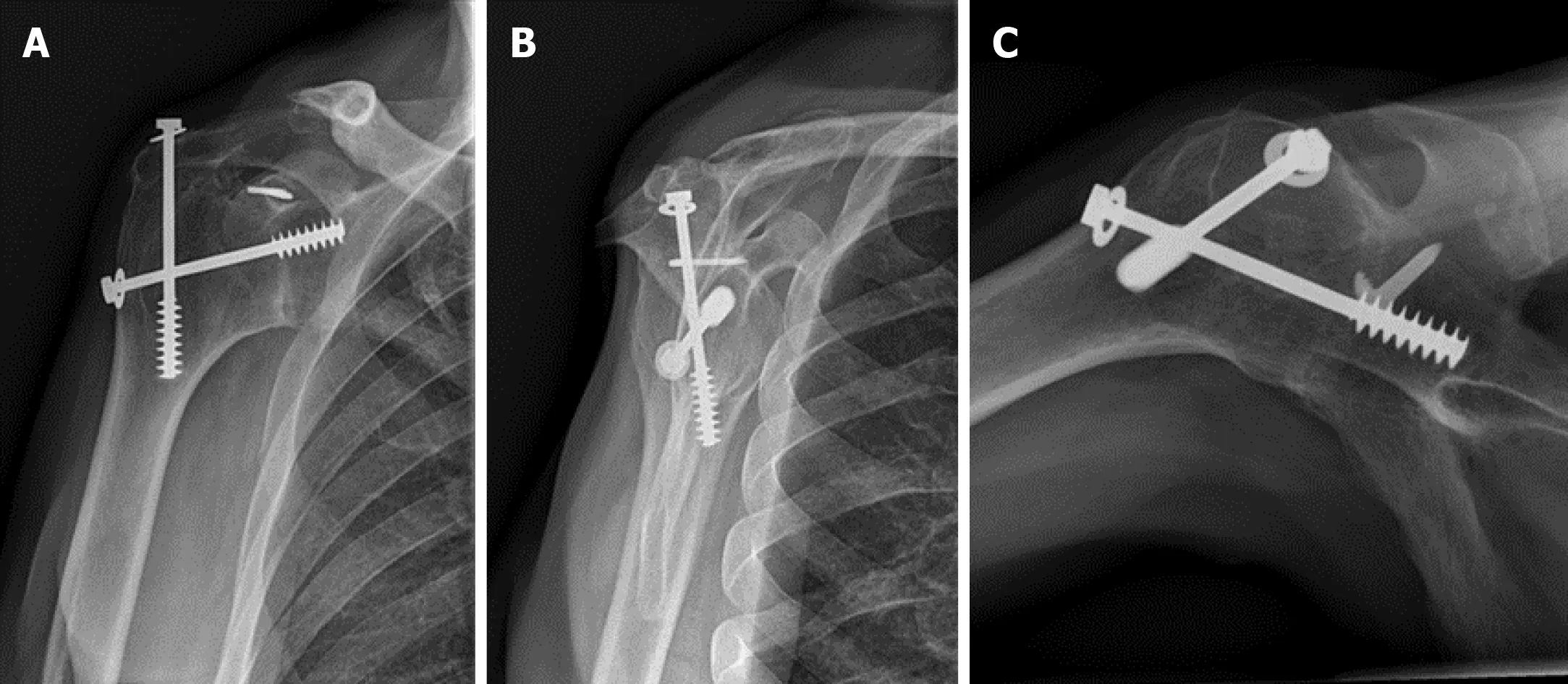
Figure 1 Conventional radiographs demonstrating the glenohumeral and acromiohumeral consolidation.
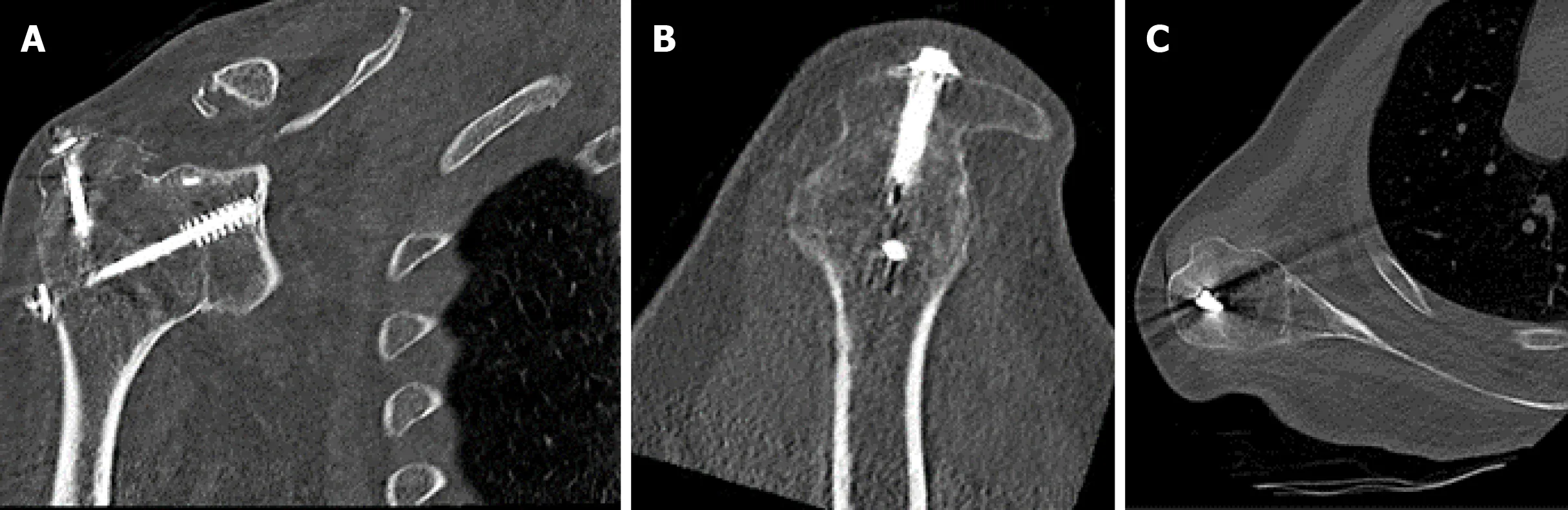
Figure 2 Preoperative Computed Tomography scan demonstrating the glenohumeral and acromiohumeral consolidation.

Figure 3 Deltopectoral approach.
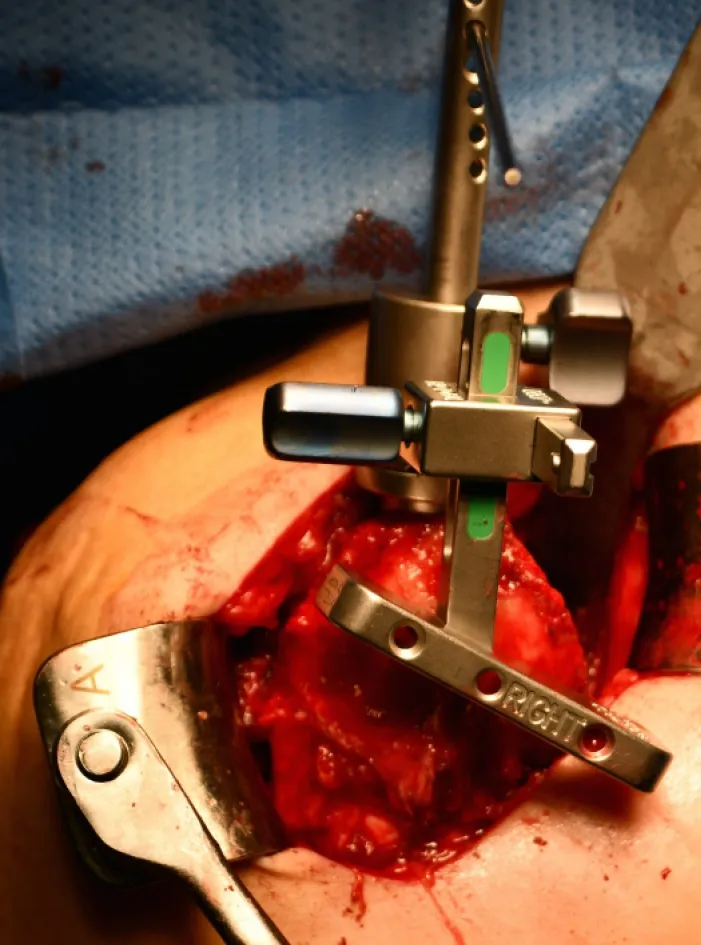
Figure 4 The glenohumeral osteotomy.
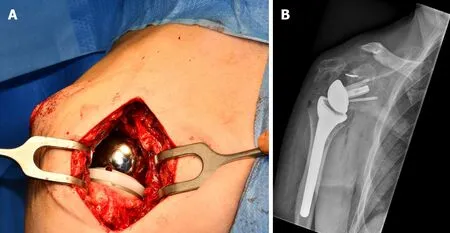
Figure 5 The implanted reverse shoulder arthroplasty.
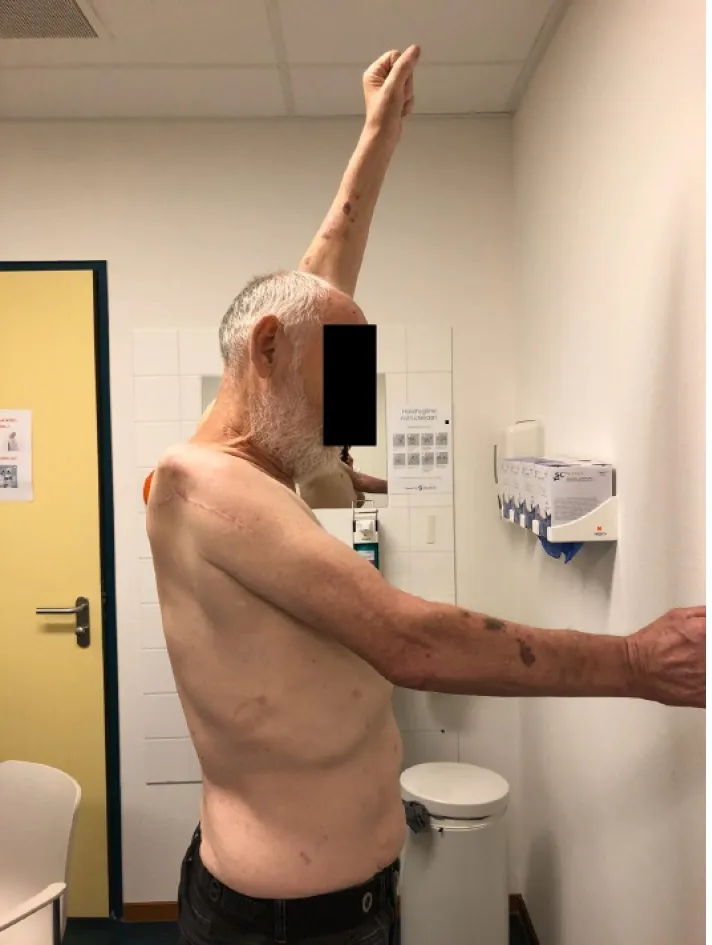
Figure 6 The active forward elevation of 50º after 12 mo postoperatively.

Figure 7 The internal rotation toTh12 12 mo postoperatively.

Figure 8 No external rotation 12 mo postoperatively.
DISCUSSION
Shoulder arthrodesis for recurrent instability is a salvage procedure to regaining stability and some degree of function[1,2]. However, after the arthrodesis not all patients are pain free. Our patient still experienced peri scapular pain and severe limitation of active range of motion. The conversion of a shoulder arthrodesis into a RSA, has been described as an alternative and promising treatment for managing pain and achieve better functional results[5,6].
In patients with a RSA, the deltoid muscle becomes the primary mover of the shoulder. Due to fibrosis and atrophy after arthrodesis, the function of the rotator cuff muscles is absent[4,6]. Therefore, the deltoid muscle function is critical to shoulder function after RSA[7,8]. Liet al[8]have suggested that preoperative EMG measurements of the deltoid muscle will help to predict the postoperative outcome of RSA. They found that postoperative shoulder strength after RSA was increased in patients with greater EMG activity of the middle deltoid. In an EMG study of Walkeret al[4], an important role for the anterior part of the deltoid is suggested. Lädermannet al[9]concluded that if partial deltoid function remains, RSA can produce reliable improvements in functional outcomes without an increased risk of dislocation. To obtain preoperative information of the activity and the quality of the deltoid muscle, we performed an EMG, which showed normal motor unit activity and recruitment in all three parts of the deltoid muscle.
A few previous case reports described conversion of a shoulder arthrodesis into hemiarthroplasty and total shoulder arthroplasty[10-13]. Patients achieved minimal functional improvement and mild to moderate pain remained. To the best of our knowledge, only two case reports of conversion of a shoulder arthrodesis into RSA are published[5,6]. No cases reported such a long interval (51 years) between arthrodesis and conversion to RSA.
Table 2 shows the patient characteristics and functional outcomes at different follow-up of patients from both studies[5,6]. Altaet al[6]found that activity in two-thirds of the deltoid was sufficient to create a stable arthroplasty, with impairment of the anterior part in three of the four patients. Only one patient preoperatively had a completely intact deltoid muscle. Nevertheless, after conversion to RSA the elevation of that patient improved with 40 degrees but postoperative elevation did not reach above shoulder height[6]. The young patient in Toneyet al[5]achieved excellent elevation of 160 degrees after conversion to RSA, with an intact deltoid muscle. However, this patient was not free of pain. In Altaet al[6], all patients experienced decreased pain, but only one patient noted a pain score of zero. Most important for our patient was his complete ceasing of peri scapular pain, and he was very pleased with the improvement in internal rotation. Despite an intact axillary nerve and anterior part of the deltoid, he lost postoperatively active forward elevation, which could be related with the timeframe between arthrodesis and reverse arthroplasty. However, the patient is a highly motivated patient who continued in a determined way with active exercises.
The importance of a complete intact deltoid muscle and the role of the anterior part seems debatable. In our opinion, the activity of the deltoid muscle can be assessed by judging the tension of the muscle during physical examination. Additional information on the deltoid muscle by performing an EMG can be considered. More cases with conversion of arthroplasty to RSA are needed to predict the outcome of shoulder function from the activity of the three parts of the deltoid muscle.
CONCLUSION
Conversion from shoulder arthrodesis to a RSA can be performed safely, with a possibility for peri scapular pain relief; even after a longstanding arthrodesis. Improvements in activities of daily living were noticed by our patient despite loss of active forward elevation.

Table 2 Outcomes of previous studies with patients who underwent conversion of arthrodesis to reversed shoulder arthrodesis
ACKNOWLEDGEMENTS
We would like to thank the patient for being so willing to participate in the case report. Thanks are also due to Schager M, our native speaker, for her help with the language and grammar.
 World Journal of Orthopedics2020年10期
World Journal of Orthopedics2020年10期
- World Journal of Orthopedics的其它文章
- Trochanteric bursitis information on the internet; can we trust the information presented?
- Long-term effect of intrathecal baclofen treatment on bone health and body composition after spinal cord injury: A case matched report
- Highly cross-linked versus conventional polyethylene inserts in total hip arthr oplasty, a five-year Roentgen stereophotogrammetric analysis randomised controlled trial
- Early clinical outcome and learning curve following unilateral primary total knee arthroplasty after introduction of a novel total knee arthroplasty system
- Mortality following combined fractures of the hip and proximal humerus
- Association of vitamin D and knee osteoarthritis in younger individuals
