Highly cross-linked versus conventional polyethylene inserts in total hip arthr oplasty, a five-year Roentgen stereophotogrammetric analysis randomised controlled trial
Justin van Loon, Daniël Hoornenborg, Inger Sierevelt, Kim TM Opdam, Gino MMJ Kerkhoffs, Daniël Haverkamp
Justin van Loon, Daniël Hoornenborg, Inger Sierevelt, Daniël Haverkamp, Department of Orthopaedic Surgery, Xpert Orthopedie Amsterdam/Specialized Center of Orthopedic Research and Education, Amsterdam 1101EA, Netherlands
Justin van Loon, Kim TM Opdam, Gino MMJ Kerkhoffs, Department of Orthopaedic Surgery, Amsterdam University Medical Centres, Location Academic Medical Center, Amsterdam 1105AZ, Netherlands
Abstract
Key Words: Highly cross-linked polyethylene; Primary total hip arthroplasty; Polyethylene wear; Roentgen stereophotogrammetric analysis
INTRODUCTION
Since the introduction of total hip arthroplasty (THA) in the 1960s, the incidence of this procedure has been increasing. Although THA is one of the most successful orthopaedic procedures, the main causes of late revisions are wear, and the resulting osteolysis causing aseptic loosening of the implant[1].
Therefore, the search to minimise wear continues and several bearing couplings over time have been tried, of which polyethylene (PE) with a ceramic head still remains the best option[2]. However, wear still occurs due to existing friction, resulting in progressive loss of material and the presence of microparticles. These PE particles induce a foreign-body reaction, which results in osteolysis[3]. The number of wear particles produced, the material used, and its morphological form determine the severity of the aforementioned reaction[4]. In response to this problem of PE wear, a highly cross-linked PE (HXLPE) has been developed. Following irradiation, freeradicals are formed, creating cross-links in the PE, which are increased by heating and reduce wear[5]. Depending on the type and dose of irradiation and the type of PE used as the control group, wear can be decreased by 42%-100% compared to traditional PE[6].
To determine the performance of an implant, a standardised and reliable method is required to measure wear. Stillinget al[7]demonstrated that wear in different directions combined with volume wear of acetabular inserts can be calculated accurately using Roentgen stereophotogrammetric analysis (RSA). As wear is one of the most important reasons for revision in THA, and therefore an indicator of long-term survival, HXLPE could reduce the number of revisions needed in the future. To prove this,in vivoanalyses with RSA are needed to confirm that thein vitroresults are confirmed in the real setting.
The objective of this randomised controlled trial (RCT) was to compare the wear of two different inlays, the HXLPE (REXPOL) and conventional PE acetabular inserts with similar ceramic head articulation, within the first five years after implantation.
Our hypothesis was that total 3D wear after five years in the REXPOL group would be less than that in the conventional PE group.
MATERIALS AND METHODS
Ethical approval/registration
This single center RCT was granted ethical approval by the local ethics committee review board of the Slotervaart Medical Center (registration number: NL23524.048.08; Dutch trial register: NL5605). The design and reporting of this study were conducted in accordance with the Consolidated Standards of Reporting Trials (CONSORT) principles.
Study design
This was a single center, double-blind RCT comparing HXLPE (REXPOL, Smith and Nephew) to standard PE acetabular inserts (Standard PE, Smith and Nephew) with similar ceramic head (Biolox, Smith and Nephew) articulation. Both the patients and investigators were blinded with regard to the group patients were assigned to. RSA analysis was performed in a blinded mode. Randomisation was performed by the use of numbered opaque envelopes, containing the prescribed PE insert. The orthopaedic surgeon randomly received those envelopes and opened them prior to the procedure.
Eligibility
Between January 2011 and January 2014, patients undergoing THA in the Slotervaart Medical Center were included in this study after completing an informed consent if they met the inclusion criteria (Table 1).
Sample size
Previous RSA studies showed a high degree of sensitivity and accuracy of measurements of migration; relatively small patient groups showed a statistically significant outcome[8]. Standard PE has a linear wear rate of around 0.06-0.08 mm/year, whereas REXPOL is expected to show almost no wear over five years. A recent publication on five-year wear results in THA measured by RSA, revealed a mean 3D wear of 0.23 mm (95%CI: 0.17-0.29) for HXLPEvs0.41 mm (95%CI: 0.32-0.50) for conventional PE[9]. Based on this difference in wear of 0.18 mm, a SD of 0.21 and a power of 80%, a sample size of 21 patients was required in each group, to identify a statistically significant difference at the 0.05 significance level.
Surgical procedure
All THAs were performed in the Slotervaart Medical Center in the standardised way using a straight lateral approach, according to the surgical technique described by the manufacturer of the implants. All patients received the same uncemented acetabular cup (EP-FIT PLUS, Smith and Nephew) and a titanium uncemented Zweymuller femoral stem implant (SL-PLUS, Smith and Nephew) with the same ceramic head articulation (Biolox, Smith and Nephew). As inclination of > 45˚ gives more wear, the navigated position of the cup is aimed to be between 40 and 45˚ of inclination and 15 to 25˚ of anteversion[10,11]. In these series, computer navigation was used to determine this position (CT free navigation Galileo, Plus Orthopedic AG, Switzerland). The liner used was either a HXLPE liner (REXPOL, Smith and Nephew) or a standard PE liner (Standard PE, Smith and Nephew). Leg length and femoral offset were aimed to be identical to the contralateral side. In addition to this procedure, at least five wellscattered tantalum markers were installed (ø 1.0 mm) with a specially designed insertion instrument into the bone around the stem component to obtain skeletal landmarks.
RSA outcomes
Patient demographics were recorded at baseline. RSA evaluations were performed postoperatively, after receiving the same standard rehabilitation program, within one week, at 6 wk, 3 mo, 6 mo, 12 mo, 24 mo and 60 mo after implantation. RSA measurements were performed as described in the guidelines of Valstaret al[8], in the supine position using a uniplanar calibration box (Medis CarbonBox nr. 011, Medis Specials, Leiden, Netherlands). Analysis of the radiographic images was carried out with the model-based RSA Software, version 4.1 (RSAcore, Dept. of Orthopaedics, LUMC, Netherlands). The RSA system resulted in anteroposterior and lateral views of the hip simultaneously. The RSA at four to seven days postoperatively was used as a baseline. By using the implanted tantalum balls that were fixed in the bone around the implant, the position of the implant relative to the bone was accurately assessed using a model-based RSA technique (Figure 1). With this technique the 2D head penetration as a measure of linear wear was measured in millimetres by the proximal-distal migration (A-axis) and medial-lateral migration (B-axis). Using this penetration, the thickness of the inlay could be calculated in millimetres. Additionally, the anteriorposterior migration (C-axis) was measured to calculate 3D head penetration, to determine the volume. The volume of the PE inlay was determined (in mm3/year) to measure the number of millimetres of linear wear/year. Normally wear occurs in the upward direction, in a cylindrical shape. However, as the wear is not only in a neat upwards direction, but also in other angles or directions, a corrected volume was also calculated, according to the formula of Hashimoto[12]. This formula has been validated as the most accurate way to determine volume wear from linear wear[13].

Table 1 Inclusion and exclusion criteria
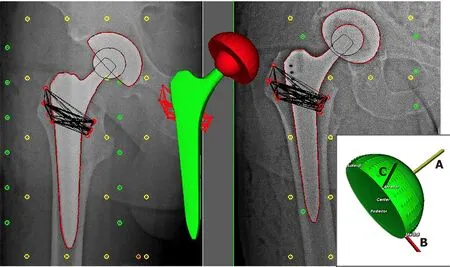
Figure 1 Model of Roentgen stereophotogrammetric analysis technique.
Functional outcomes
The pain and activity of daily living (ADL) domains of the Hip Injury and Osteoarthritis Outcome Score (HOOS) were assessed pre-operatively, and after five years by a research nurse[14]. The HOOS was constructed to assess patient-relevant outcomes in five separate subscales: Pain, symptoms, ADL, sport and recreation function and hip-related quality of life. The sum scores of the domains in this questionnaire are transformed into a zero to 100, worst to best scale. Another functional questionnaire assessed, was the Harris Hip Score (HHS)[15]. This questionnaire was focussed on pain and function, completed by range of motion and deformity. The maximum of 100 points is the best possible outcome.
Statistical analysis
Statistical analyses were performed with IBM SPSS Statistics version 26.0 (IBM Corp., Armonk, NY, United States). After confirmation of normal distribution, continuous variables are presented as mean ± SD. Categorical data are described as numbers with accompanying proportions. A mixed model analysis was performed to evaluate the amount of wear between both groups during follow-up. The effect of the different inlay was considered as a model factor and interaction with the follow-up time was evaluated to assess the differences in progression of wear in both inlays. The difference in wear at final follow-up was assessed by the Student’st-test. To assess the differences of the PROMs between the inlay groups after five years, univariate as well as multivariate regression analyses were performed to adjust for potential confounders such as demographics. The differences were significant if thePvalues were less than 0.05. All statistical methods in this study were performed by a biomedical statistical expert (Inger N Sierevelt).
RESULTS
A total of 51 consecutive patients were included in this study at baseline. Figure 2 shows a flow chart of the patients during this study. Seven patients were excluded, and the remaining 44 patients were included in our analysis; 22 in the REXPOL and 22 in the Standard PE insert group. During follow-up, five patients in the REXPOL group and three in the Standard PE group were lost to follow-up. The patient demographics and baseline characteristics of both groups were comparable and are shown in Table 2. No significant differences were seen in cup sizes between the two groups and no revisions were needed during follow-up in either group.
RSA migration
The total wear of the inlay measured from baseline showed less wear in all directions in the REXPOL group, which was significant in the REXPOL group in the lateromedial direction. All results of total wear measured from baseline are shown in Table 3. Due to a significant interaction between cup type and follow-up time, the wear pattern during follow-up of the REXPOL and Standard PE inlay were analysed separately. These wear patterns over the years showed greater wear in all directions in the conventional PE group, which is shown in Figures 3-6. The corresponding wear rates over this time period in Table 4 show that in all directions and volumes calculated, conventional PE had significant wear rates, whereas REXPOL did not show this outcome over time. The RSA images showed no signs of osteolysis.
Functional outcomes
The functional questionnaires were obtained at five years, to detect potential differences in functional outcomes. These results are shown in Table 5, with no significant differences observed.
DISCUSSION
The main finding of this study is that total 3D wear was less in the REXPOL group than in the standard PE group, with significant less wear in the medial direction after five years. Moreover, the wear rates in the medial and proximal direction and in both volume and corrected volume were significant in the standard PE group, but not in the REXPOL group.
Severalin vivostudies have shown that HXLPE can reduce wear in comparison with normal PE inlays in THA[16]. However, only one study investigated the results of REXPOLin vivo, without randomisation and RSA analysis[17]. The outcomes in that study supported our findings of reduced wear in the REXPOL group, with approximately 70% less wear at the five-year follow-up. Therefore, this study is the first to present randomised clinical RSA data regarding the REXPOL liner.
In otherin vivostudies using RSA, a systematic review performed by Callaryet al[18]showed that only 12 cohorts comprising 260 THAs have compared the outcomes of HXLPEvsnormal PE. Their recommendations on standardisation of reporting RSA outcomes are applied in our study. However, the studies included in their review assessed different inlays and not all of them were randomised. Thus, our study contributes to their statement that more longer-term standardised studies are needed to improve our understanding of the factors related to wear. Moreover, this will provide a better indication of the chance of osteolysis and as a result loosening of the cup and revision in the longer term.
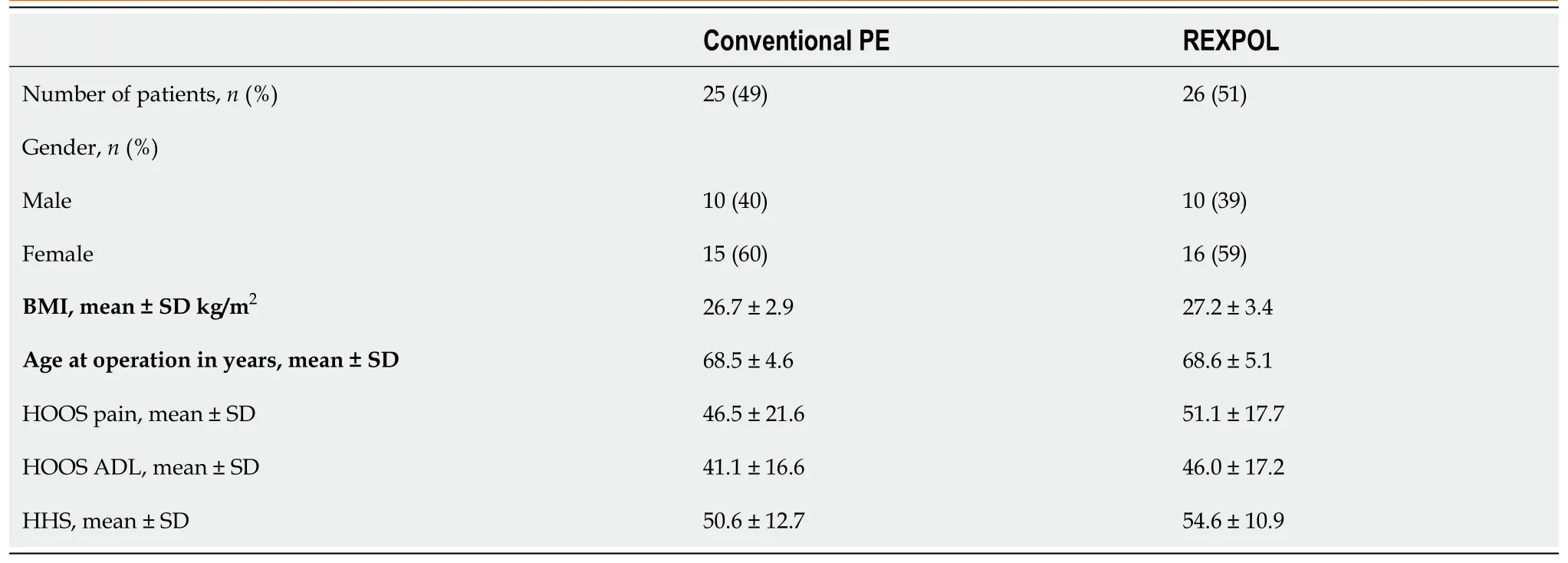
Table 2 Patient and baseline characteristics

Table 3 Total wear in all directions at the five-year follow-up, presented as mean with ranges

Table 4 Mean wear rates per year, presented as mean with ranges

Table 5 Functional outcomes at the five-year follow-up, presented as mean with 95%CI
A literature review by Dumbletonet al[19]showed that a threshold for wear of 0.05 mm/year would eliminate osteolysis. Although both standard PE and REXPOL showed wear rates below this threshold in our study, the long-term wear of REXPOL is still unclear. Long-term results were reported in the study by Broomfieldet al[20]using another brand of HXPLE with the same low wear rates at 12 years. Rates of 0.03 mm/year were seen in the standard PE group and 0.003 mm/year in the HXLPE group, with higher wear rates in patients with osteolysis. Their long-term outcomes were supported by several studies showing ten-year or longer wear rates in favour of HXLPE[21-23]. Moreover, the study by Oparaugoet al[24]clarified the correlation between wear debris-induced osteolysis, volumetric wear-rates and revision.

Figure 2 Flow chart of follow-up.

Figure 3 Wear of the inlay in the medial direction in mm over time (months).
Despite this correlation, subsequent concern was raised that HXLPE microparticles would show increased bioactivityin vivoas this had been observed inin vitrostudies, since these particles are smaller than conventional PE[25-27]. However, thein vivostudy by Lachiewiczet al[28]showed that at 10 to 14 years, small osteolytic lesions were also seen with HXLPE. Broomfieldet al[20]supported this outcome and showed 50% osteolysis after 12-years with conventional PEvs4% with HXPLE, which was statistically significant. This shows that HXLPE wear particles are not more biologically active than conventional PE and may not elevate the risk of osteolysis.
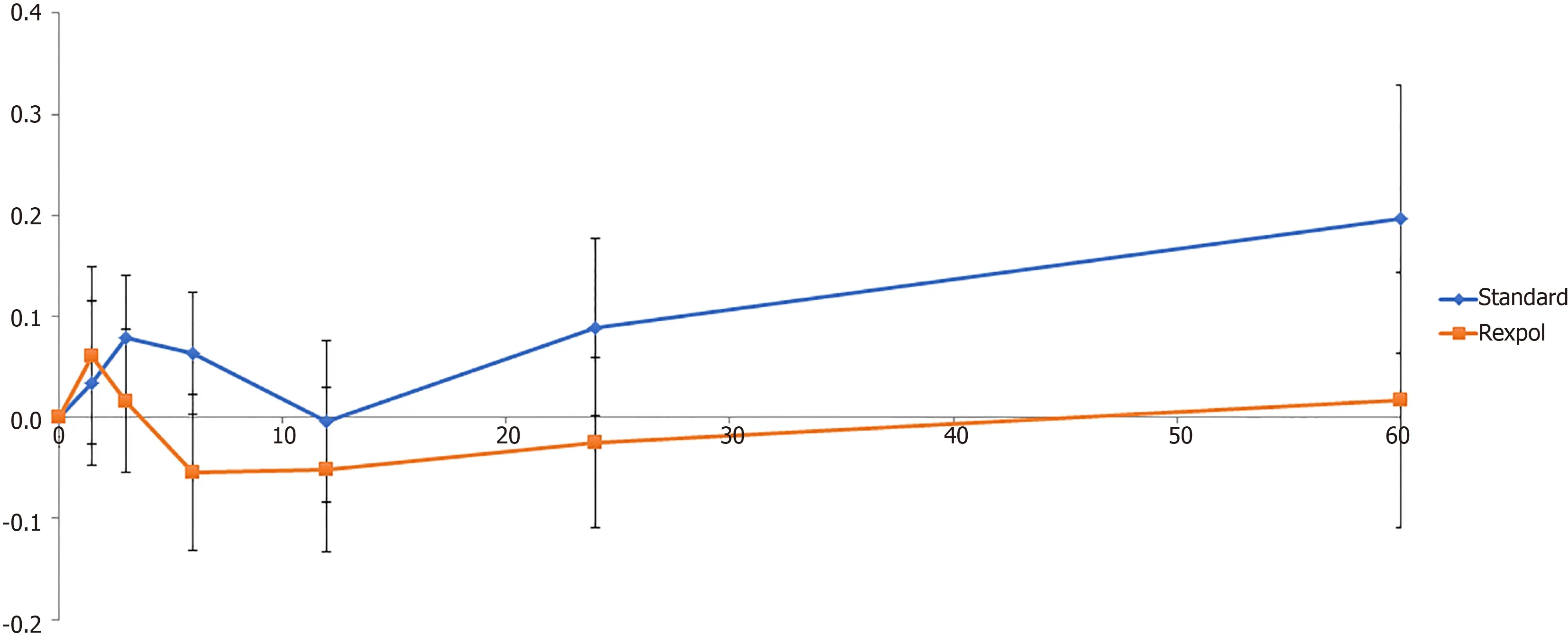
Figure 4 Wear of the inlay in the proximal direction in mm over time (months).

Figure 5 Volumetric wear of the inlay in mm3 over time (months).
As osteolysis is one of the main reasons for loosening of the cup, the aforementioned results on long-term reduction of osteolysis become even more clinically relevant if a reduction in revisions is seen over time. The study by Hannaet al[29]showed less wear in the HXLPE group and as a result no osteolysis or revisions at 13-years in the HXPLE group with an implant survival rate of 100%vs86% in the conventional PE group. De Steigeret al[30]also confirmed this in a large observational study and showed a 16-year cumulative revision rate of 11.7% with conventional PEvs6.2% with HXLPE. The aforementioned outcomes confirm that the lower wear rates of HXLPE as seen in our study can reduce the risk of osteolysis when compared to conventional PE and can also reduce revision rates in the longer term.
By measuring wear as the slope of the amount of penetration in the different directions, some negative results on wear are seen in this study. These negative wear rate outcomes have been reported in previous studies[1,31-35]. However, this may be due to lower wear rates of HXLPE being harder to accurately measure compared to conventional PE. Although RSA is considered the best way to measure wear of a prothesis, it has an accuracy range of 0.022 mm to 0.086 mm, depending on the direction of measurement. In the case of HXPLE with even lower wear rates, it becomes more challenging to determine small amounts of wear[36]. Therefore, it becomes more important to have large cohorts to detect significant differences. As our study was carried out with small cohorts, the wear results should be interpreted while bearing this in mind. The expectation is that in the longer term these wear rates can be calculated more accurately for HXLPE, because they will be determined outwith the threshold. Since our RSA analysis was performed while in the supine position, another explanation of the negative wear rates is subluxation of the femoral head while lying. However, this was not confirmed by the review conducted by Callaryet al[18]who showed no differences between the studies on supine or standing RSA. To overcome problems of negative wear results, long-term results of HXLPE wear are needed.

Figure 6 Corrected volumetric wear of the inlay in mm3 over time (months).
According to the outcomes in favour of HXLPE, this study confirms that the use of inlays such as the REXPOL, is preferred in THAs.
风险投资在近年“共享经济”的飞速发展中被人所熟知,是投资中介向特别有潜能的高新技术产业投入风险资本后,实现利益共享、风险共担的一种投资方式。大学生创业遇到的最大问题就是资金不足。以Dormi为例,在校创业阶段,有政府提供的项目资金与学校举办相关活动的奖金。在转型进入更大市场时,依靠前期盈利与创始团队家庭支持是不够的,必须寻求社会资金的帮助。对于风险投资公司来说,他们也希望寻找到有发展潜力的中小型项目,通过早期“资本换股权”,从而在未来公司成熟后以更高价格将股权卖出获得收益[2]。
Limitations
The clinical outcomes of our study were measured to assess any major drawbacks of standard PE or HXLPE at the five-year follow-up. As improvement from baseline was seen in both groups with no significant differences between the groups, no practical disadvantages were seen by preferring one inlay over the other. As the study was not powered by clinical outcomes, further research is needed to investigate these outcomes.
Implications for further research
This study showed, for the first time, that REXPOL resulted in less wear in the shortterm in a randomised setting by RSA. Therefore, further investigation of wear over a longer period should be performed, to confirm that REXPOL can reduce the risk of osteolysis and consequently reduce revision rates in THA. Also, more research needs to be carried out to overcome problems of minimal differences in wear rates. In addition, research on other variables that influence wear such as activity, weight and surgical factors such as inclination of the acetabular component should be performed.
CONCLUSION
Total 3D wear is less with REXPOL inlay than with conventional PE inlay in THAs after five years. This study confirmed, for the first time, that the REXPOL HXLPE inlay is preferred to the standard PE inlay.
ARTICLE HIGHLIGHTS
Research background
Highly cross-linked polyethylene (HXLPE) inlay in total hip arthroplasty (THA) is thought to result in lower wear rates in vivo, compared to conventional polyethylene.
Research motivation
More in vivo studies are needed, especially those using Roentgen stereophotogrammetric analysis (RSA), to confirm the advantage of HXLPE over conventional polyethylene (PE).
Research objectives
The objective of the study was to compare wear of the HXLPE (REXPOL) and conventional PE acetabular inlay with similar ceramic head articulation, within the first five years after implantation.
Research methods
A double-blind randomised controlled trial was performed to compare wear of REXPOL, a HXLPE, with conventional PE within the first five years after implantation using RSA.
Research results
The HXLPE (REXPOL) inlay showed less wear in the latero-medial direction. Significant wear rates of the conventional PE inlay were seen in the latero-medial and center-proximal direction and in volume and corrected volume, whereas the REXPOL inlay did not show this outcome over time.
Research conclusions
Total 3D wear is less with the REXPOL (HXLPE) inlay than with the conventional PE inlay in THAs after five years.
Research perspectives
Further investigations into the long-term wear and factors that might influence wear rates should be conducted, to confirm that HXLPE (REXPOL) can reduce the risk of osteolysis and consequently reduce revision rates in THA. In addition, an investigation of the impact of wear reduction by HXPLE on the functional outcomes of patients is required.
 World Journal of Orthopedics2020年10期
World Journal of Orthopedics2020年10期
- World Journal of Orthopedics的其它文章
- Trochanteric bursitis information on the internet; can we trust the information presented?
- Conversion to reverse shoulder arthroplasty fifty-one years after shoulder arthrodesis: A case report
- Long-term effect of intrathecal baclofen treatment on bone health and body composition after spinal cord injury: A case matched report
- Early clinical outcome and learning curve following unilateral primary total knee arthroplasty after introduction of a novel total knee arthroplasty system
- Mortality following combined fractures of the hip and proximal humerus
- Association of vitamin D and knee osteoarthritis in younger individuals
