Treatment of a rotator cuff tear combined with iatrogenic glenoid fracture and shoulder instability: A rare case report
Chen-Hao Chiang,Ting-Chien Tsai, Kuan-Kai Tung,Wei-Hsing Chih,Ming-Long Yeh, Wei-Ren Su
Chen-Hao Chiang, Ming-Long Yeh, Department of Biomedical Engineering, National Cheng Kung University, Tainan 70428, Taiwan
Chen-Hao Chiang, Ting-Chien Tsai, Wei-Hsing Chih, Department of Orthopaedic Surgery, Ditmanson Medical Foundation Chia-Yi Christian Hospital, Chia-Yi 60002, Taiwan
Kuan-Kai Tung, Department of Orthopaedic Surgery, Taichung Veterans General Hospital, Taichung 40705, Taiwan
Wei-Ren Su, Department of Orthopaedic Surgery, National Cheng Kung University Hospital, Tainan 70428, Taiwan
Abstract
Key Words: Frozen shoulder; Bursitis; Arthroscopy; Fracture; Glenoid fracture; Manipulation; Iatrogenic; Case report
INTRODUCTION
Rotator cuff tears accompanied by adhesive capsulitis are common in clinical practice[1-3]. Both problems are prevalent causes of shoulder pain and disability. Manipulation under anesthesia with or without arthroscopic capsular release is an effective operative treatment for a refractory stiff shoulder[3-6]. Rotator cuff repair combined with capsular release can achieve a good functional outcome with a low retear rate[7]. Some severe complications have been reported after the manipulation (e.g., humeral fracture, glenohumeral dislocation, and brachial plexus injury)[3,8]. Therefore, performing an arthroscopic capsular release before a shoulder manipulation is suggested to decrease the incidence of complications[3,9,10]. However, some surgeons still prefer to perform the manipulation before arthroscopy to facilitate the performance of the arthroscopy, and the use of an arthroscope after manipulation could increase the release and address any concomitant problems[9-12]. Furthermore, a high rate of iatrogenic intraarticular damage may occur during the manipulation[13]. The incidence of glenoid fracture after manipulation is rare, according to historical reports[8,14,15]. We present a case of antero-inferior glenoid rim fracture combined with shoulder instability after manipulation for shoulder stiffness. Arthroscopic repair of the glenoid fracture and concomitant rotator cuff tear was performed. A good outcome was achieved with this treatment. Informed consent was obtained from the patient, and she gave permission for her case to be published.
CASE PRESENTATION
Chief complaints
A 58-year-old woman presented to our clinic with a history of right shoulder pain and decreased range of motion (ROM) for more than 1 year.
History of present illness
She had a history of diabetes mellitus and was treated with oral diabetic medication. Adhesive capsulitis was suspected, and a physical therapy program was arranged to increase passive motion. Unfortunately, the ROM and right shoulder function showed no improvement after 2 mo of rehabilitation (Table 1).
History of past illness
She denied history of trauma of the right shoulder. She had a history of diabetes mellitus and was treated with oral diabetic medication.
Personal and family history
The patient herself and her family had not suffer from this symptom before.
Physical examination
There were positive findings for the Hawkin’s and empty can tests. The decreased ROM function is described in Table 1.

Table 1 Functional result before surgery and at the postoperative 2-year follow-up
Laboratory examinations
All laboratory tests revealed no significant result.
Imaging examinations
A magnetic resonance imaging assessment revealed a small-sized full-thickness supraspinatus tear and wall thickening at the inferior capsule of the shoulder. No fractures were identified in the preoperative image evaluation (Figure 1).
FINAL DIAGNOSIS
Before operation, the tentative diagnosis was small-sized full-thickness supraspinatus tear and adhesive capsulitis. After manipulation, the final diagnosis was shifted to small-sized full-thickness supraspinatus tear combined with the glenoid fracture and shoulder instability.
TREATMENT
She was given general anesthesia and placed in the supine position. Brisement manipulation was first performed and begun with forward flexion in internal rotation with light traction, which held the arm close to the axilla to decrease the lever effect. Continuous gentle pressure was applied, and a distinct clicking sound with a givingway sensation was noted mid-way when the arm elevation was at 150 degrees. The Xray was checked, and no proximal humeral fracture or dislocation was found. Then, manipulation for abduction, external rotation, and internal rotation was performed. After the manipulation, an examination revealed grade II laxity during anterior translation for the right shoulder[16].
Shoulder arthroscopy was then performed with the patient in the beach-chair position, starting from the standard posterior portal. A fresh fracture of the anteroinferior rim of the glenoid was noted (Figure 2). The size of the fragment was measured by a laser-marked device about 5 mm and 15 mm in the anterior-posterior and superior-inferior directions, respectively. Due to hypermobile anterior translation of the glenohumeral joint, fracture fixation was decided. Anteroinferior and accessory anterosuperior portals were establishedviaan outside-in technique. Three 2.8-mm Twinfix Ti suture anchors (Smith & Nephew, Andover, MA, United States) were set in place at the lower edge, upper edge, and middle of the fractured glenoid for fixation of the fractured glenoid rim (Figure 2). After fracture fixation, the anterior translation test found no instability. Then, a complete capsular release was performed arthroscopically[8]. Repeated examinations showed good stability with full ROM. The fixed glenoid fracture was checked again arthroscopically and showed good stability with no displacement. Arthroscopic rotator cuff repair was then performed by two 5.0-mm Twinfix Ti suture anchors (Smith & Nephew) as the double-row suture technique in the subacromial space (Figure 2).
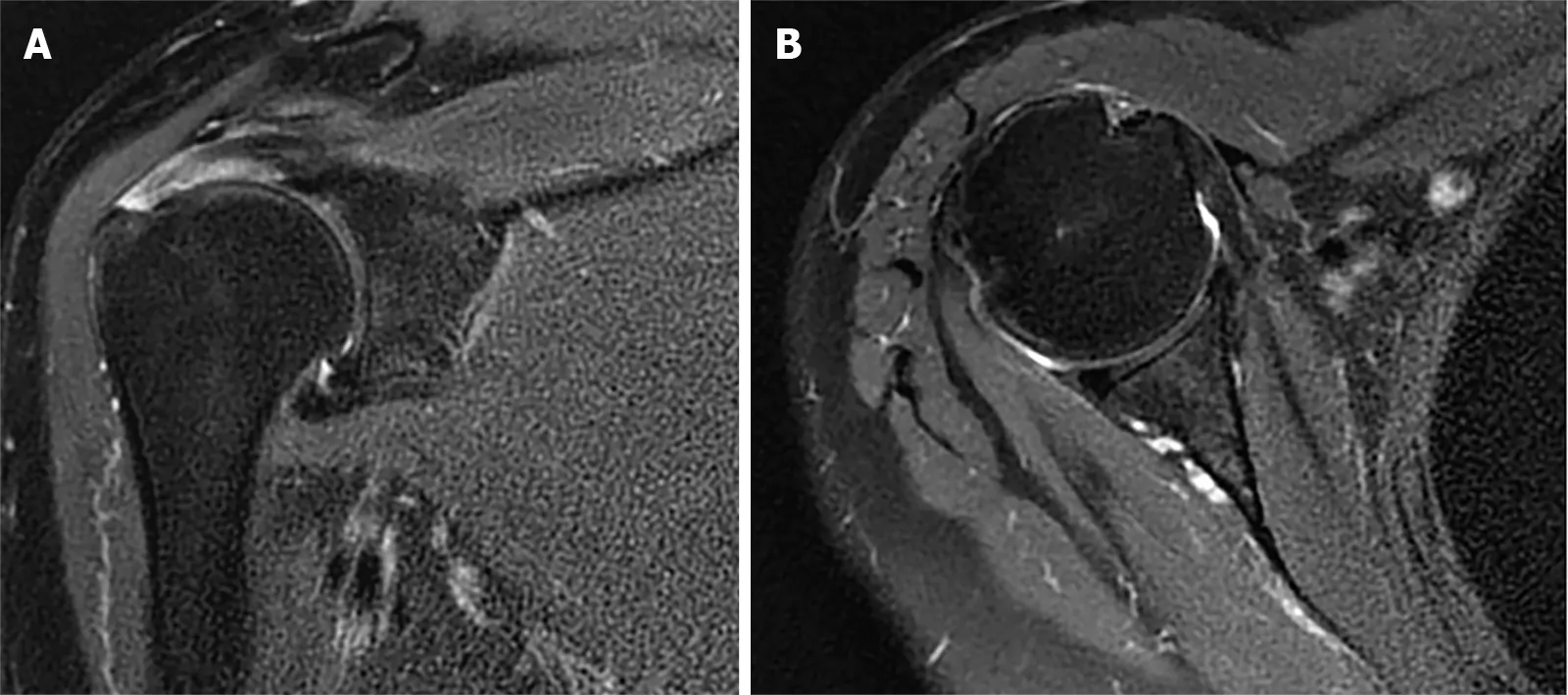
Figure 1 Magnetic resonance imaging of the right shoulder before surgery.
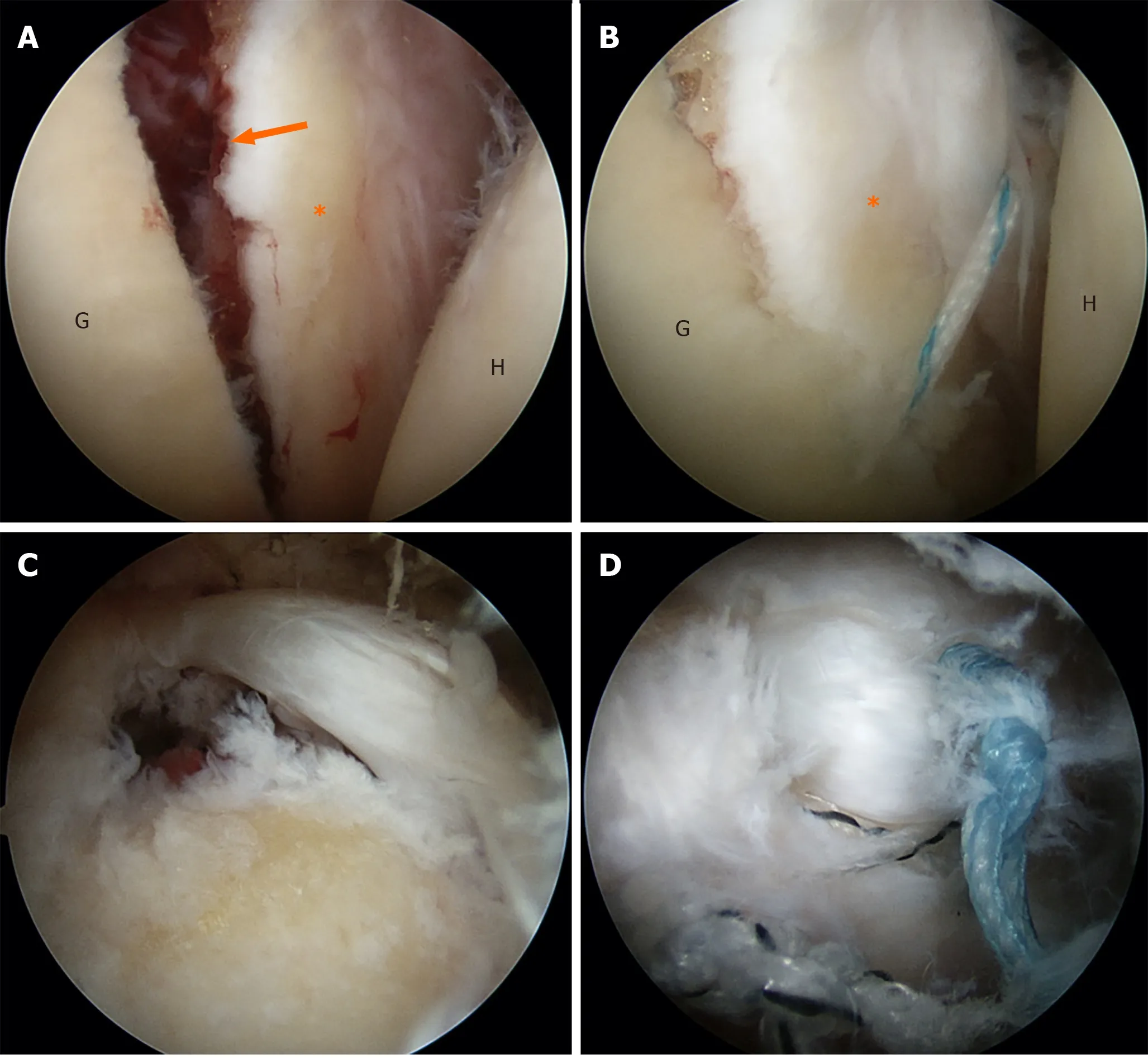
Figure 2 Intraoperative photographs.
OUTCOME AND FOLLOW-UP
After surgery, the patient was immobilized in a simple sling, and gentle passive pendulum exercise was allowed for 6 wk, followed by active-assisted ROM exercises coupled with a comprehensive strengthening program. A computed tomography scan revealed healing of the fracture 3 mo after surgery (Figure 3). More aggressive training for strengthening and overhead lifting began from month 4, in accordance with the recovery of ROM and strength.
At the 1-year and 2-year postoperative follow-ups, functional outcomes had improved beyond the baseline preoperative measures, and the patient was satisfied with the surgical outcome (Table 1 and Figure 4).
DISCUSSION
Manipulation under anesthesia or arthroscopic capsular release is effective in treating a refractory stiff shoulder. For cases with coexisting rotator cuff tears, arthroscopic capsular release for the stiff shoulder combined with repair for the rotator cuff tear can achieve a good result[7]. Therefore, in cases of a stiff shoulder combined with a rotator cuff tear, surgeons can use an arthroscope to evaluate and address possible injuries and to perform additional capsular release, in addition to the manipulation procedure. Although there was no evidence to show that aggressive treatment for the coexisting problems could achieve a better outcome than manipulation only, it is reasonable to suggest that a better outcome can be achieved if all the problems can be treated in a minimally invasive manner, rather than with open surgery. This kind of aggressive treatment would be more suitable for patients with a strong motivation for rehabilitation and would result in a shorter treatment time than treating both of the problems separately or nonoperatively[1].
The management of the glenoid fracture remained controversial. Magnussenet al[17]reported a case with glenoid fracture during manipulation. The fracture healed only after immobilization without any surgical treatment. On the other hand, glenoid rim fractures often lead to chronic shoulder instability, and avulsion fractures of more than 5 mm with the instability of the glenohumeral joint may require operative stabilization[18,19]. Patients with glenoid fracture treated with arthroscopic anchor or screw fixation can also achieve uneventful healing and good functional results[20]. Arthroscopic fixation for glenoid fracture can minimize soft tissue dissection and manipulation. Additionally, with stable fixation and a reduced glenoid fossa, early rehabilitation can be allowed, complications related to malunion can be avoided, and good functional outcomes are more likely.
The reported results for arthroscopic repair of rotator cuff tears only and of tears combined with Bankart lesions have been similar and good[21,22]. The conditions in our case may be similar to those of a rotator cuff tear combined with a Bankart lesion. The treatment for both sites may have outcomes similar to those of rotator cuff repair only. Although the results are affected by capsule release, we would be more confident in allowing the patient to begin early motion rehabilitation if the glenoid fracture could be fixed together with the rotator cuff.
CONCLUSION
We would like to suggest that surgeons who experience a giving-way sensation after an obvious popping sound perform a radiographic check-up or an arthroscopic exam. Additionally, shoulder instability tests could be performed to evaluate possible instability. Arthroscopic fixation for an iatrogenic glenoid fracture and repair of a coexisting rotator cuff tear can provide stability needed for early rehabilitation. Fracture healing and good functional outcomes can be achieved.
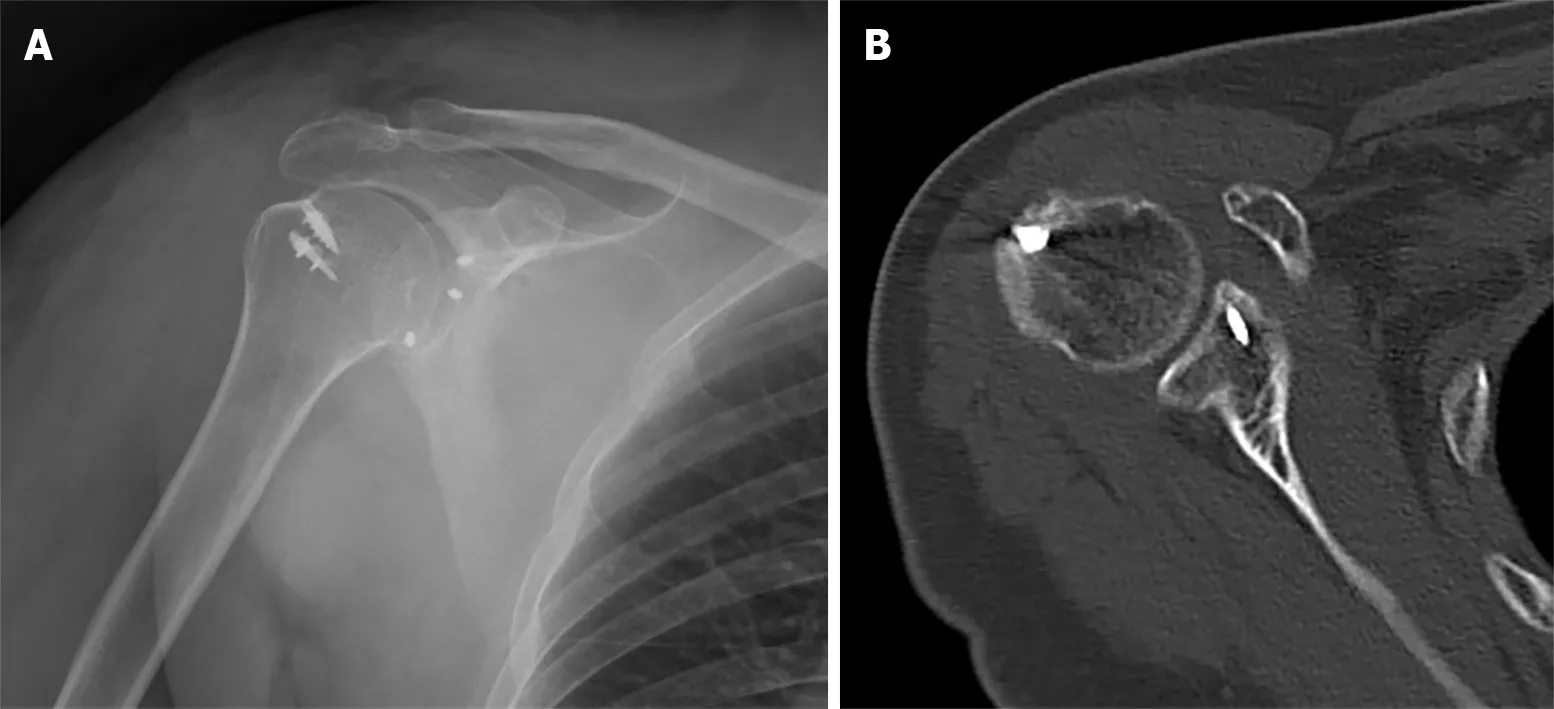
Figure 3 Radiograph at the 3-mo follow-up.

Figure 4 Timeline of the case.
ACKNOWLEDGEMENTS
We thank Huang HK, MD and Lin CH, MS (Department of Orthopaedics, Ditmanson Medical Foundation Chia-Yi Christian Hospital, Chiayi, Taiwan) for assistance with this case report.
 World Journal of Orthopedics2020年11期
World Journal of Orthopedics2020年11期
- World Journal of Orthopedics的其它文章
- Radiographic evaluation of vascularity in scaphoid nonunions: A review
- Does proximal femoral nail antirotation achieve better outcome than previous-generation proximal femoral nail?
- Patients’ perspectives on the conventional synthetic cast vs a newly developed open cast for ankle sprains
- Proximal fibular osteotomy: Systematic review on its outcomes
- Müller-Weiss disease: Four case reports
- Modified surgical treatment for a patient with neurofibromatosis scoliosis: A case report
