In-Stent Thrombosis after Antiplatelet Therapy Conversion while Awaiting Coronary Bypass
Nathan Burke,BS ,Tawanna Charlton,MS ,Hussam Hawamdeh,MD and Ki Park,MD,MS
1 Division of Cardiovascular Medicine,University of Florida College of Medicine,Gainesville,Florida,USA
Abstract
Keywords:Acute myocardial infarction/ST-elevation myocardial infarction; antiplatelet therapy; genetics; platelet biology; drug-eluting stent; drugs/pharmacotherapy
Abbreviations:CABG,coronary artery bypass grafting; DAPT,dual antiplatelet therapy; IST,in-stent thrombosis; IVUS,intravenous ultrasound; OR,odds ratio; PCI,percutaneous coronary intervention; RCA,right coronary artery;STEMI,ST-elevation myocardial infarction; TIMI,Thrombolysis in Myocardial Infarction.
Introduction
In-stent thrombosis (IST) is a rare yet potentially catastrophic complication following percutaneous coronary intervention (PCI) that may occur despite optimal stent placement.In addition to the technical aspects of PCI in preventing future complications,the use of dual antiplatelet therapy (DAPT) is a key component in maintaining stent patency following the procedure.The challenges in using DAPT include suboptimal platelet reactivity,bleeding risk,and the high cost of certain antiplatelet therapies.Our case highlights the complexity of P2Y12receptor antagonist therapy and the subsequent consequences of poor metabolization.
Case Report
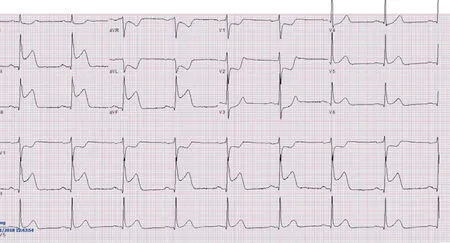
Figure1 Admission 12-Lead Electrocardiogram.
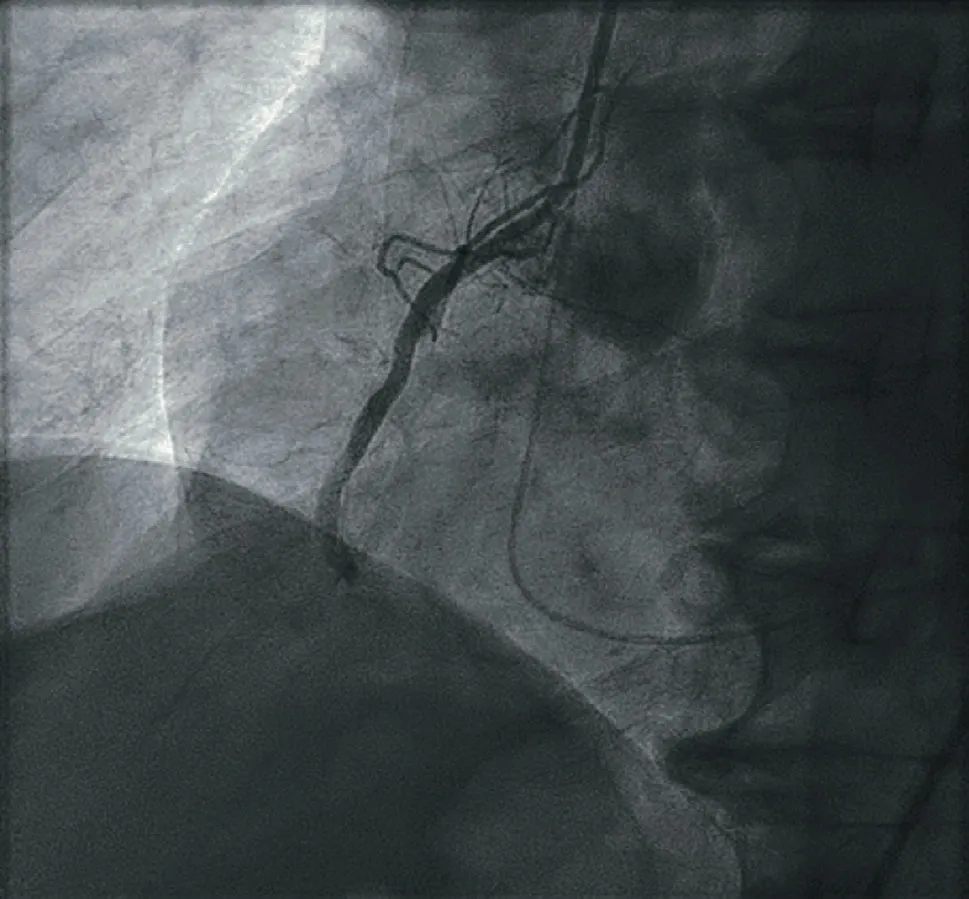
Figure2 Posterior Left Ventricular Angiography before Stenting.
An 81-year-old man with a medical history of hypertension and hyperlipidemia presented to the emergency department with weakness and discomfort in his left arm that developed after exertion.Electrocardiogram revealed inferior ST elevation(Figure1).The patient was given 180 mg of ticagrelor and transferred to our primary PCI facility.On arrival,the patient was hypotensive with intermittent atrioventricular block.Right coronary artery (RCA) occlusion was suspected.Because of the patient’ s tenuous hemodynamic status,RCA angiography was performed before left coronary angiography and revealed the culprit mid RCA occlusion (Figure2).A workhorse wire was advanced into the RCA and used to cross the suspected lesion.A 2.0 mm × 12 mm compliant balloon was then used to predilate the mid RCA occlusion.An intravascular ultrasound (IVUS) catheter was then advanced to determine the size of the vessel.Evidence of thrombus in the posterior left ventricular branch was present.An aspiration thrombectomy catheter was advanced,and aspiration of the thrombus was performed,with minimal thrombus retrieved.A 3.25 mm × 28 mm drug-eluting stent was deployed and advanced.A 3.25 mm × 15 mm noncompliant balloon was used to postdilate the middle portion of the stent.IVUS catheter inspection revealed a well-apposed and expanded stent(Figure3) without evidence of vessel complication and no edge dissection.Postdeployment angiography conf irmed successful stenting of the mid RCA,with restored Thrombolysis in Myocardial Infarction (TIMI) 3 f low (Figure4).
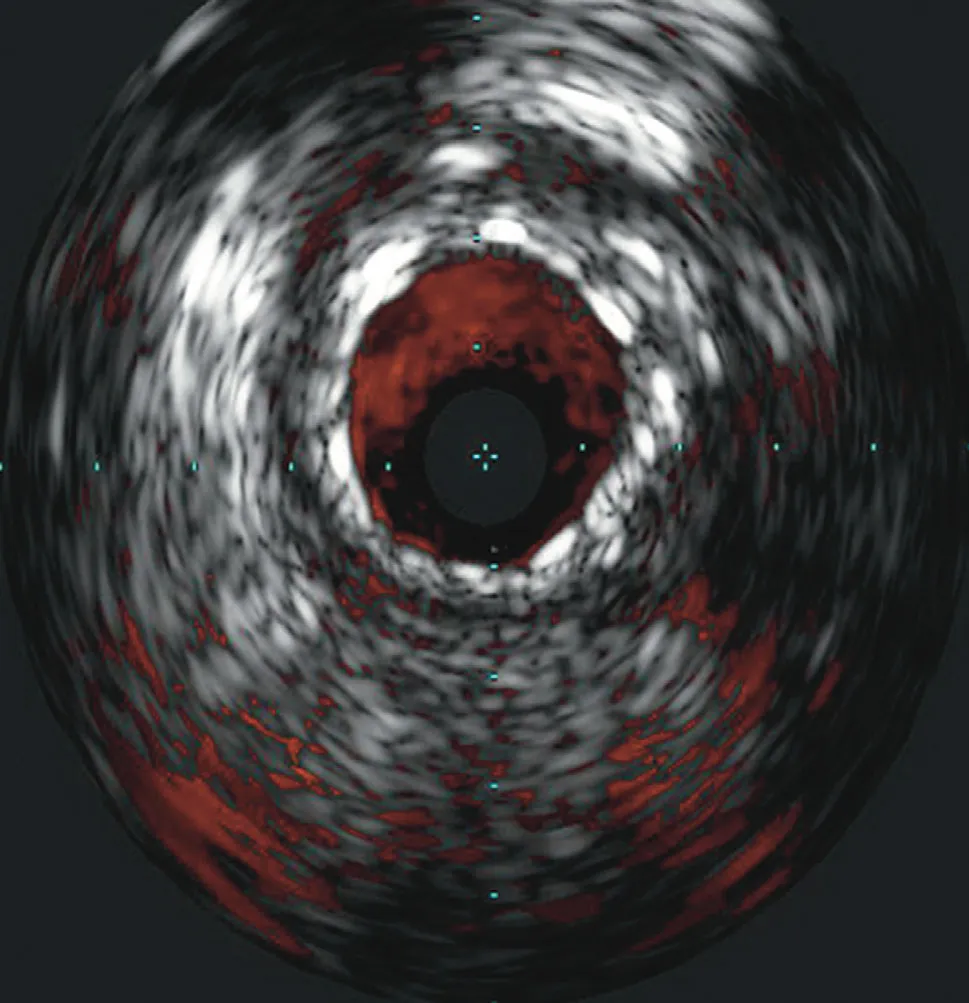
Figure3 Intravascular Ultrasound Catheter Conf irmation Following Stent Placement.

Figure4 Right Coronary Angiography after Stenting.
Subsequent left coronary angiography revealed high-grade complex distal left main coronary artery disease.As the patient remained stable,no PCI was performed at that time and the patient was transferred to the cardiac critical care unit.Transthoracic echocardiography revealed an ejection fraction of 45- 49% with inferior wall akinesis.The patient was referred for coronary artery bypass grafting(CABG),which he initially refused and elected for an outpatient high-risk PCI.The patient was discharged in a stable condition 2 days later while receiving ticagrelor and low-dose aspirin.Four days following discharge,the patient presented to the emergency department with recurrent angina.A cardiothoracic surgeon was consulted,and the patient agreed to proceed with inpatient CABG.Because of concern for perioperative bleeding risk,the patient was switched from ticagrelor to clopidogrel therapy per cardiothoracic surgeon request.Before ticagrelor was stopped,the patient was given clopidogrel with an initial dose of 300 mg and then 75 mg daily.The patient remained in the hospital,and CABG was scheduled to be performed 4 days after admission.The day before surgery,4 days after conversion from ticagrelor to clopidogrel therapy,he developed an inferior ST-elevation myocardial infarction (STEMI) (Figure5).A cardiothoracic surgeon was contacted,and the patient was transferred to the cardiac catheterization laboratory for emergent angiography,which revealed IST.Balloon angioplasty and aspiration of the RCA thrombus was performed (Figure6).Optical coherence tomography revealed the presence of thrombus inside the stent without evidence of edge dissection or other cause of stent thrombosis.TIMI 3 f low was restored,and the patient returned to the cardiac intensive care unit in stable condition to await CABG,which was successfully performed the following day.CYP2C19genotype assessment was ordered to assess the cause of the IST.Genotyping revealed the presence of two copies of theCYP2C19*2loss-of-function allele in theCYP2C19gene,indicating that the patient was a poor clopidogrel metabolizer.Thus,subtherapeutic levels of the active clopidogrel metabolite led to an increased risk of stent thrombosis.
Discussion
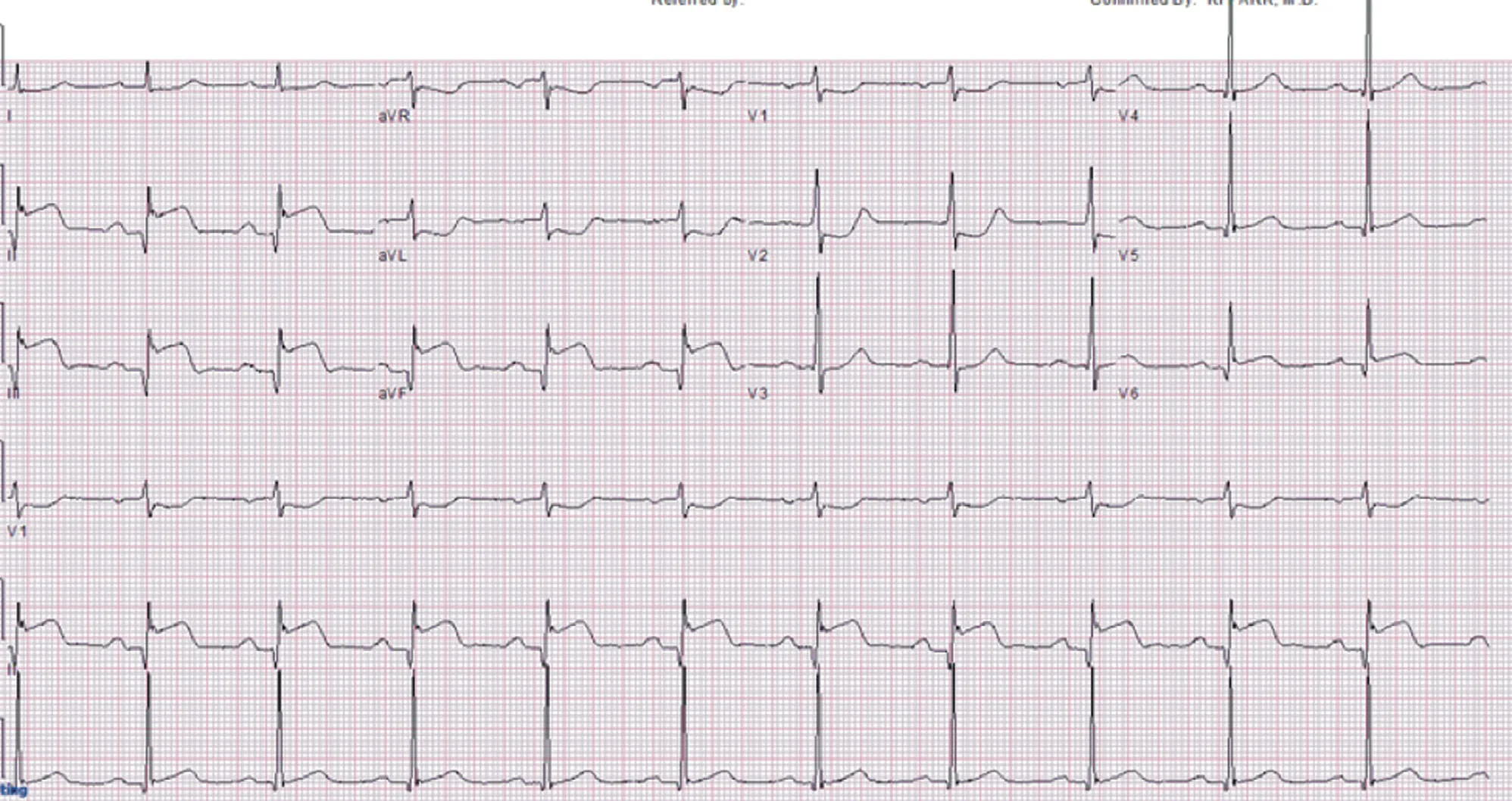
Figure5 Inferior ST-Elevation Myocardial Infarction,4 Days after Conversion from Ticagrelor to Clopidogrel Therapy.
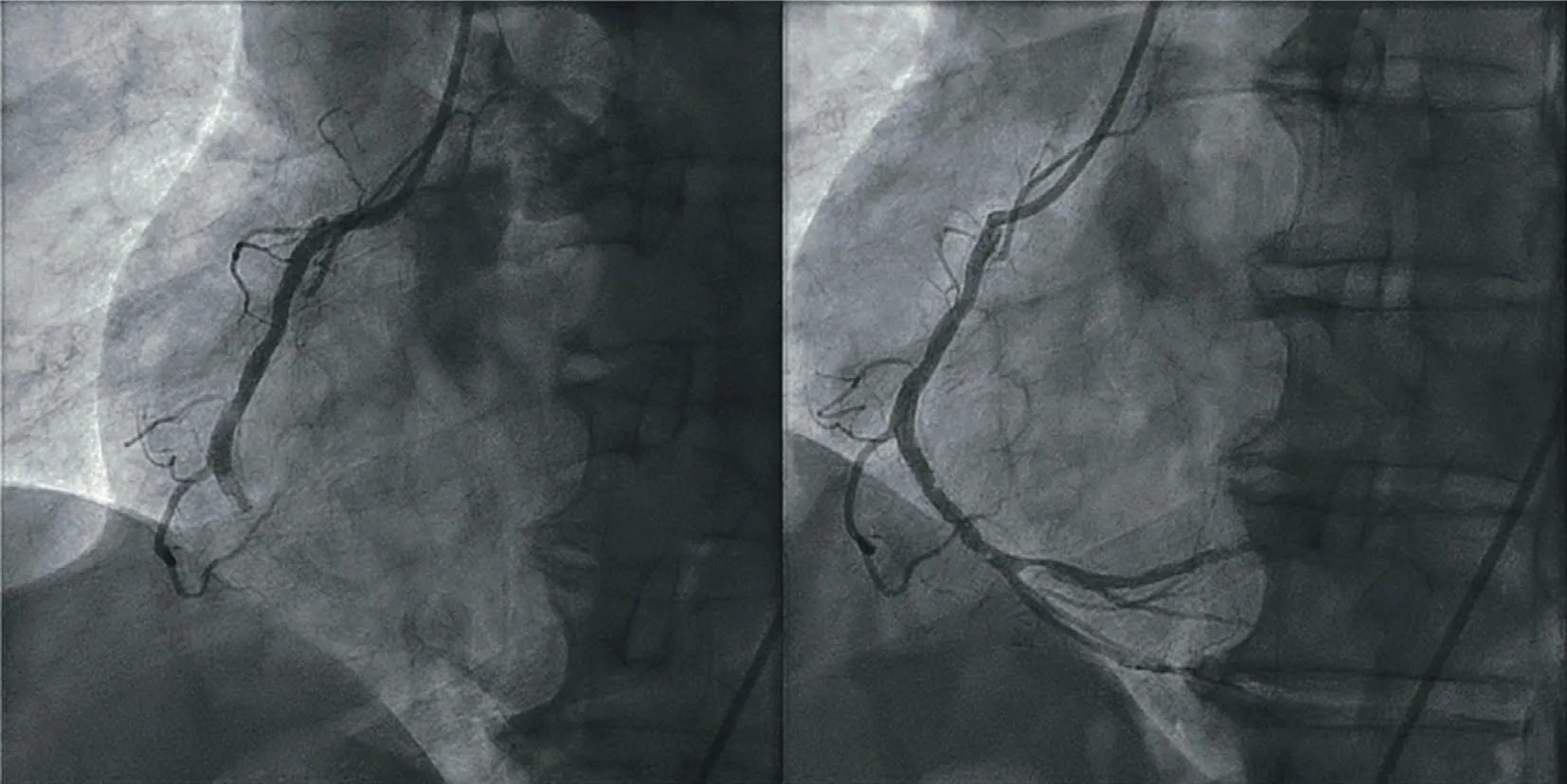
Figure6 Before (left) and after (right) Balloon Angioplasty and Aspiration of the Right Coronary Artery Thrombus.
This case highlights potential challenges when one is evaluating patients who present with IST.It is important to consider intracoronary imaging during PCI in patients presenting with acute coronary syndrome,particularly STEMI.The most predictive risk factors for early IST (within 30 days)include the premature discontinuation of use of P2Y12inhibitors (odds ratio [OR] 36.5),undersized stents (OR = 13.46),coronary artery dissection(OR = 6.19),low TIMI f low after PCI (OR = 5.24),and coronary artery disease greater than 50% proximal to the lesion (OR = 4.15) [1].The use of intracoronary imaging facilitates optimization of PCI and reduces the risks of stent underexpansion and malapposition.As we performed intracoronary imaging during the initial PCI and again during the recurrent STEMI with IST,we determined that mechanical factors related to stent deployment were not responsible for IST.With respect to this and the timing of the recurrent IST,altered genetic response to clopidogrel metabolization was suspected to play a role in IST.The studied recovery of platelet function following withdrawal of ticagrelor between 48 hours and 5 days is consistent with the recurrent STEMI 4 days after conversion from ticagrelor to clopidogrel therapy in this case (with conf irmed intake of clopidogrel due to inpatient administration) [2].SeveralCYP2C19genetic polymorphisms are known to contribute to poor active metabolite generation and subsequent thrombotic events in patients taking clopidogrel.The most common mutations leading to poor clopidogrel metabolism areCYP2C19*2andCYP2C19*3loss-of-function alleles [3,4].Standard-of-care DAPT currently includes the administration of ticagrelor or prasugrel,active metabolite inhibitors of the P2Y12receptor,to bypass the risk of thrombotic events that may be in part due to these polymorphisms.With the advances in genetic testing technology,rapid genetic testing for mutations that lead to clopidogrel resistance are now widely available.Although routine testing for CYP2C19 mutations is not indicated at this time,in select cases genetic testing may be considered,especially in patients with a history of stent thrombosis after PCI,such as our patient [5,6].Genotyping patients after PCI for acute coronary syndrome may also provide useful prognostic data for predicting cardiovascular risk of both ischemic and bleeding events [6].While preventive genetic testing is not routinely recommended for patients undergoing PCI,ongoing clinical trial data are needed to determine the ideal patients who are most likely to benef it from genotype testing.
Conclusion
IST is an uncommon but potential fatal complication of PCI.General considerations for the cause of IST include suboptimal stent deployment and suboptimal response to antiplatelet therapy.Our case highlights the importance of intracoronary imaging to exclude mechanical stent-related features that could lead to IST.Conf idence in stent optimization leads to the further differential of suboptimal response to antiplatelet therapy; in our case,this testing led to the proven diagnosis of poor clopidogrel metabolizer status and prompt change to more eff icacious antiplatelet therapies.
Funding Information
None
Disclosures
None
 Cardiovascular Innovations and Applications2020年4期
Cardiovascular Innovations and Applications2020年4期
- Cardiovascular Innovations and Applications的其它文章
- Comparison of Clinical Value between Right Distal Radial Artery Access and Right Radial Artery Access in Patients Undergoing Coronary Angiography or Percutaneous Coronary Intervention
- Epicardial Adipose Tissue in Patients with Obstructive Sleep Apnea:A Systematic Review and Meta-analysis
- Comparison of Segmentation Algorithms for Detecting Myocardial Infarction Using Late Gadolinium Enhancement Magnetic Resonance Imaging
- Current Management Strategies in Patients with Heart Failure and Atrial Fibrillation:A Review of the Literature
- lmpact of MitraClip Program on the Volume and Outcomes of Mitral Valve Surgery:A Single-Center Retrospective Study
- Clinical Analysis of Transcatheter Embolotherapy for Congenital Pulmonary Arteriovenous Fistulas in Children
