Risk factors of Clostridium difficile infection in ICU patients with hospital-acquired diarrhea: A case-control study
Majid Akrami, Hadiseh Hosamirudsari, Yousef Alimohamadi, Samaneh Akbarpour, Leyla Mehri, Akram Khalili Noshabadi, Mahnaz Sarabi, Majid Neshat
1Department of Anesthesiology, Baharloo Hospital, Railway Square, Tehran University of Medical Sciences, Tehran, Iran
2Department of Infectious Diseases, Baharloo Hospital, Railway Square, Tehran University of Medical Sciences, Tehran, Iran 3Anitimicrobial Resistance Research Center, Institute of Immunology and Infectious diseases, Iran University of Medical Sciences,Tehran, Iran 4Occupational Sleep Research Centre, Baharloo Hospital, Tehran University of Medical Sciences, Tehran, Iran
5Intensive Care Unit, Baharloo Hospital, Railway Square, Tehran University of Medical Sciences, Tehran, Iran
ABSTRACT Objective: To identify the risk factors of Clostridium difficile infection (CDI) in diarrheal patients admitted to the intensive care unit (ICU) in Tehran Baharloo Hospital.Methods: A case-control study was conducted on ICU patients with hospital-acquired diarrhea. A total of 101 patients were divided into two groups: the case group (CDI positive, n=47) and the control group (CDI negative, n=54). The baseline information such as use of antibiotics, other drugs administration, treatments before diarrhea,laboratory results, and vital signs of the two groups were compared.Besides, logistic regression model was used to assess the correlation between CDI positivity and mortality.Results: Hospital stay length, ICU stay length, duration from admission to diarrhea onset, and nasogastric feeding duration,mechanical ventilation rate and its duration were significantly different from these of the control group (P<0.05). The frequency of proton pump inhibitor and carbapenem in the case group was significantly higher than that of the control group (P<0.05). In addition, age had a significant effect on the mortality of CDI patients.Conclusions: Patients with older age, longer duration of hospital or ICU stay, longer duration of endotracheal feeding and/or intubation were more susceptible to CDI. In addition, proton pump inhibitor and carbapenem use influenced the gut microbiome diversity and increased the CDI risk in patients.
KEYWORDS: Clostridium difficile; Carbapenem; ICU; Risk factor
1. Introduction
As a Gram-positive anaerobic and spore-forming bacteria[1],Clostridium difficile(C. difficile) is the most common infectious cause of diarrhea in ICU. Patients with predisposing factors that disrupt the normal flora in gastrointestinal tract are susceptible to the colonization ofC. difficileinfection (CDI)[2,3]. The predisposing factors include broad-spectrum antibiotics, aging, hospitalization(especially in ICU), renal failure, hypoalbuminemia, nasogastric feeding, comorbidities, and invasive gastrointestinal procedures[4,5].Protone pump inhibitor (PPI) is a possible cause of CDI[5]. The administration of antibiotics is a major cause of severe colitis in ICU[6]. Various researches reported different antibiotic classes associated with CDI. In one research cephalosporin and clindamycin were reported as the most common cause[7], but another study reported fluoroquinolone[8]. Studies on the CDI risk factors are limited in Iran. The most recent one is a cross-sectional study on the CDI antibiogram and its risk factors[9]. Other researches are mainly on epidemiology, antibiotic susceptibility, and molecular studies[10-14]. This case-control study aims to identify the associated factors of CDI in ICU patients with hospital-acquired diarrhea.
2. Materials and methods
2.1. Ethics approval
The study was approved by the Ethics Committee of Tehran University of Medical Sciences. The approval code is 96-03-30-4399.
2.2. Study design
The current case-control study was conducted at the Baharloo Hospital, a general hospital with 330 beds. Patients admitted to ICU between July 2017 to February 2019 were selected. These patients were diagnosed as acute diarrhea, with loose stools at least 3 times within 24 h. They were followed-up until the discharge or death.Patients were excluded if they had colectomy, chronic renal failure,inflammatory bowel disease, hepatic failure, laxatives concurrently,or had diarrhea within 72 h following ICU admission.
A total of 101 patients were selected for further analysis. At the onset of diarrhea, stool samples were collected for stool examination and culture.
2.3. Diagnosis and grouping
Hospital-acquired diarrhea was defined as loose stools for three or more times in 24 h. Diarrheic patients with positive CDI were assigned to the case group. The patients who had hospital-acquired diarrhea without CDI served as the control group.
2.4. C. difficile detection
Stool samples from 101 patients were sent to the hospital laboratory for smear, culture, andC. difficiletoxin assay. Glutamate dehydrogenase (GDH) method with sensitivity and specificity as 100.0% and 92.8% respectively[15,16] was used for CDI detection.The Clostridium K-set (Coris Bio concept-Belgium) was applied.
2.5. Data collection
Data were obtained from medical records, physical examinations,and ICU report sheets. The data included age, gender, length of hospital stay, usage of antibiotics, PPI or H2blocker administration,duration of mechanical ventilation, and nasogastric feeding.
Acute Physiological and Chronic Health Evaluation II score was used to predict the severity of underlying diseases. Patients with acute nosocomial diarrhea were categorized into two groups based on the GDH results:C. difficleassociated diarrhea (the case group)and non-C. difficleassociated diarrhea (the control group).
2.6. Statistical analyses
Statistical analysis was performed using SPSS 16 edition (SPSS Inc., Chicago, IL). Variables with a normal distribution were expressed as mean ± SD and compared using Student’st-test.Variables with a non-normal distribution were described as median and interquartile range (IQR). To compare categorical variables, theχ2test or Fisher’s test was performed. Multivariate logistic regression analysis including all potential risk factors for CDI was performed to estimate the correlation between CDI and mortality. Data were adjusted for age, sex, antibiotic use, diabetes mellitus, and duration of nasogastric feeding. The significant level was set at α=0.05.
3. Results
Among these 101 samples, 47 were positive (the case group),and 54 samples were negative (the control group). The baseline characteristics of the case group and the control group were summarized in Table 1. There was no significant difference between the two groups in baseline variables except for hospital stay length, ICU stay length, duration from admission to diarrhea onset, and nasogastric feeding duration (P<0.05) (Table 1).Treatments before onset of hospital-acquired diarrhea are presented in Table 2. The rate of intubation, duration of intubation, and duration of nasogastric feeding in the case group were significantly more than that in the control group (P<0.05) (Table 2). Except for the PPI, there was no significant difference in drug usage between the case and the control group (Table 3).
There was no significant difference in the use of antibiotics except for carbapenem (Table 4). The leukocytosis, folate serum levels, and complicated diarrhea were significantly higher in the case group than the control group (P<0.05). Other variables on the onset day of diarrhea were not significantly different between the two groups on the onset day of diarrhea (Table 5). According to the results of multiple logistic regression, only age had a significant impact on the mortality of CDI patients (Table 6).
4. Discussion
C. difficileis a common pathogen of hospital-acquired infection,with high mortality and morbidity[17]. CDI is caused by multiple predisposing factors including intubation, nasogastric feeding, and antibiotic use. Mechanical ventilation could change the patient’s normal flora and lead to CDI. Nasogastric feeding could also result in changes in intestinal microflora[5,18]. Antibiotic-associated diarrhea is known for disrupting the balance of normal gut microbiota. In this study, we found that ICU stay length of the case group is longer than that of the control group (P<0.05), which were similar to other studies[19-21].
We also found that the duration of endotracheal intubation and nasogastric feeding in the case group was also significantly longerthan the control group (P<0.05). Contamination of diet and low fiber diet may decrease the intestinal acidity and causeC. difficilecolonization[22]. The longer duration of endotracheal intubation or nasogastric feeding, patients are more prone to CDI. Other studies have also shown that there is a significant association between nasogastric feeding and incidence of CDI[1,18,22,23]. The critically ill patients, who need mechanical ventilation, are faced with several comorbidities and nosocomial infections such as pneumonia.These conditions increase the number of gut neutrophils and their permeability.
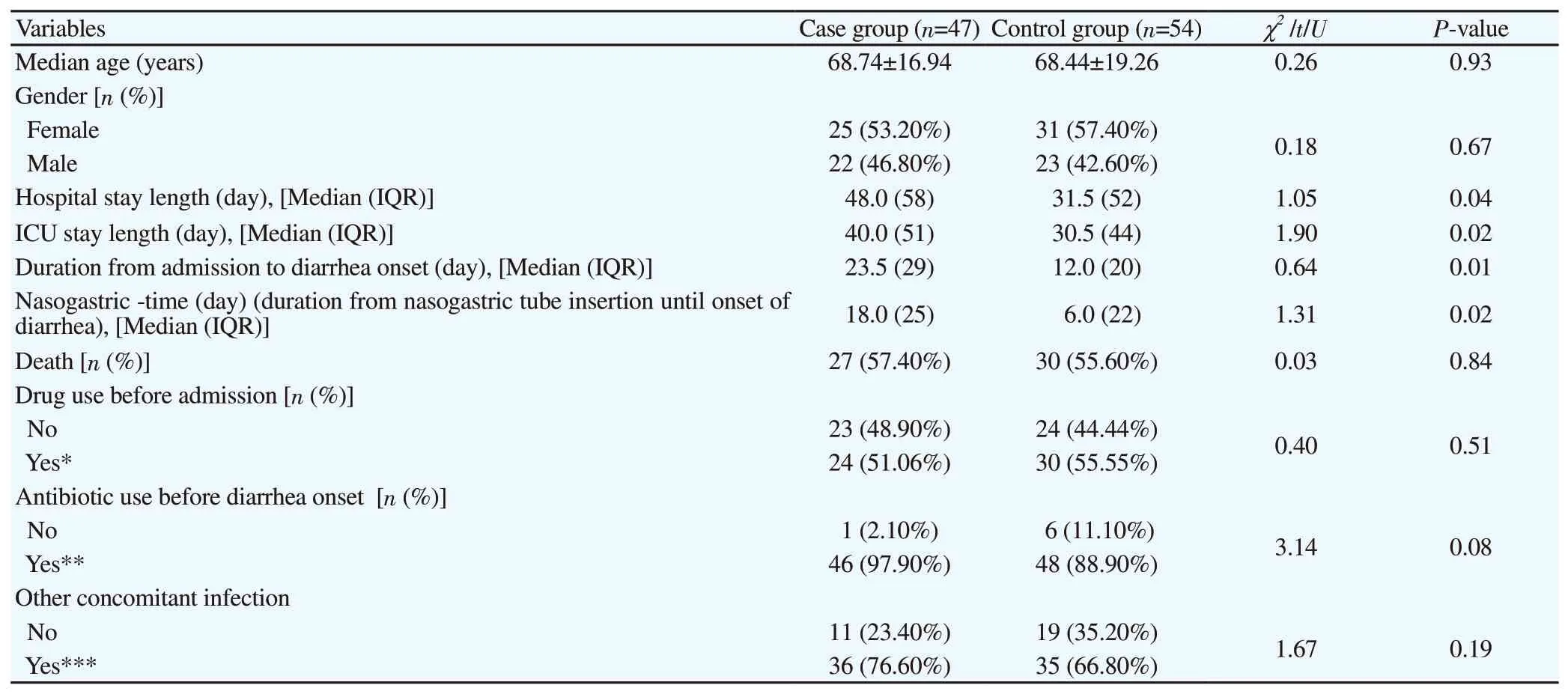
Table 1. Characteristics of patients with hospital-acquired diarrhea.
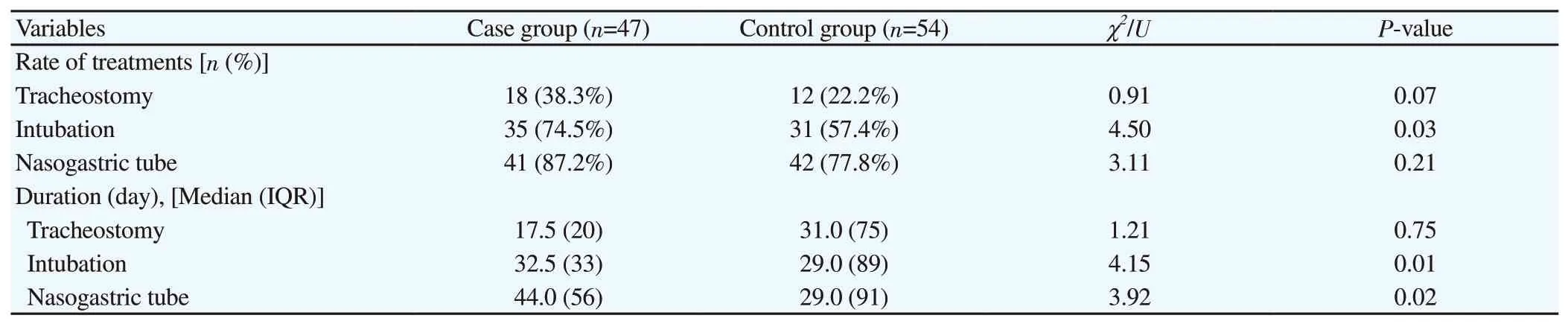
Table 2. Treatment and duration before onset of hospital-acquired diarrhea.
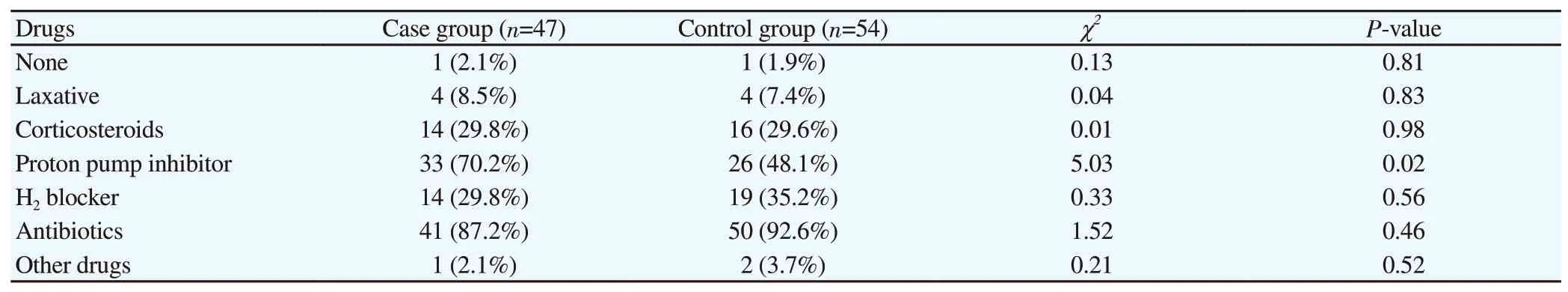
Table 3. Drugs administered before onset of hospital-acquired diarrhea [n (%)].
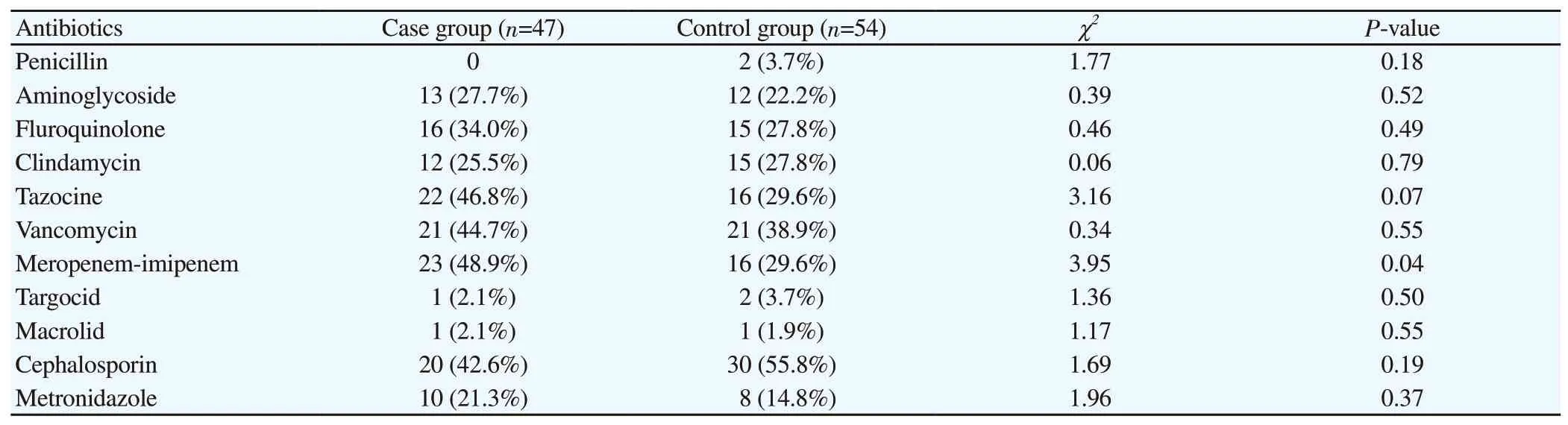
Table 4. Antibiotic used before diarrhea onset [n (%)].
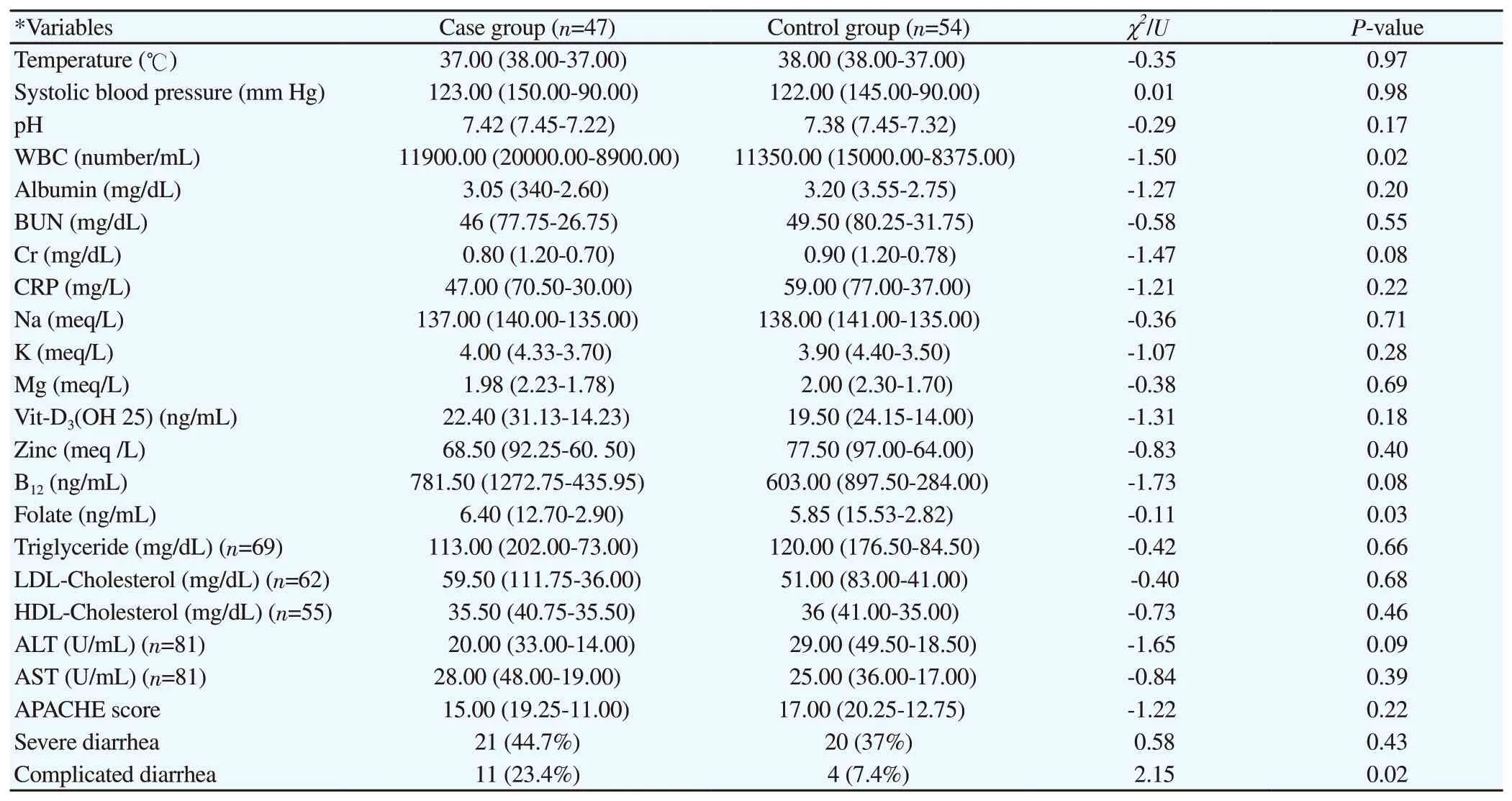
Table 5. Laboratory results and vital signs on the first day of diarrhea onset.
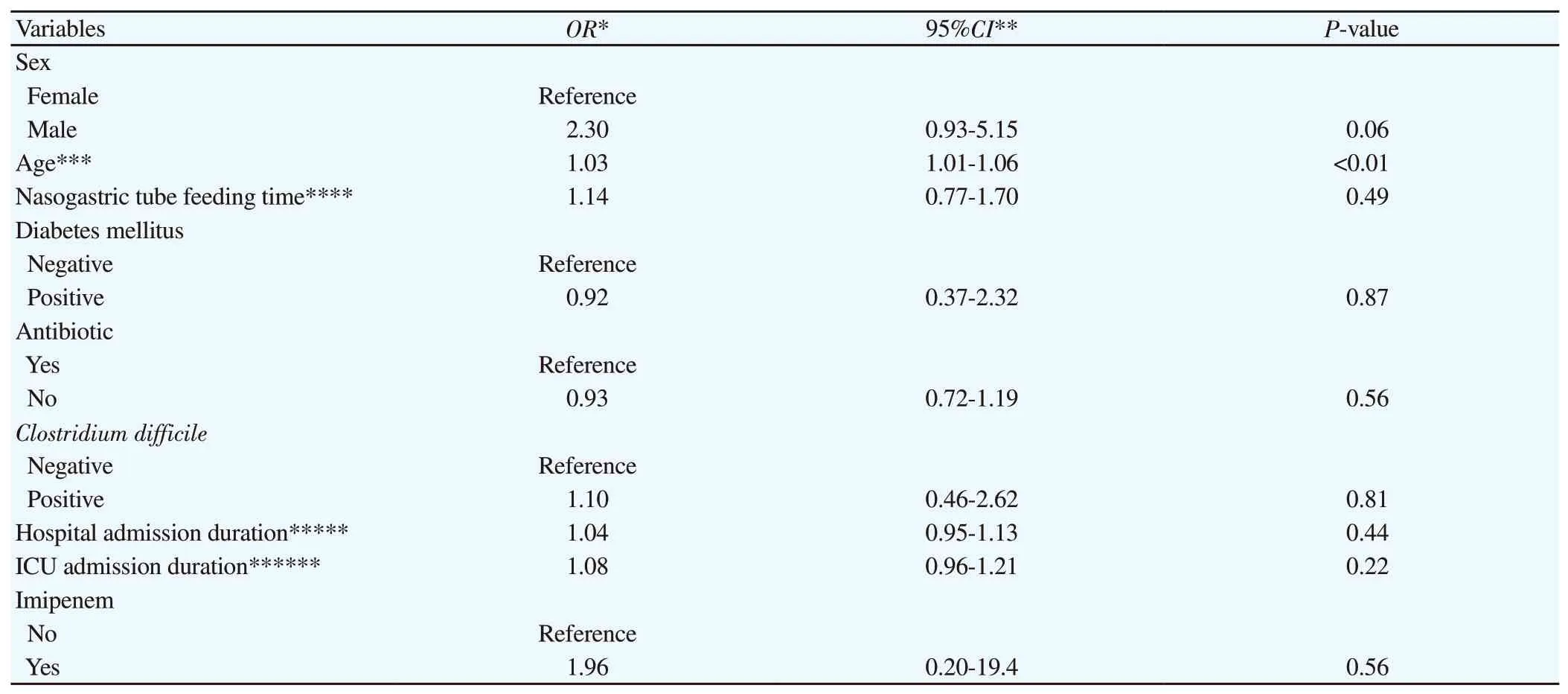
Table 6. Result of logistic regression.
The present study showed that the duration from admission to diarrhea onset in the case group is longer than that in the control group (P<0.05). The longer the admission duration is, the more nasogastric feeding, endotracheal intubation, and contamination of feeding diet patients receive. These factors are predisposing factors of CDI[1,5,18,22].
Our study showed that the use of PPI in the case group is significantly higher than the control group (P<0.05), which is similar to other researhes[2,3,24-26]. PPI use can decrease gut microbial diversity by changing gastric pH[5,27]. Antibiotic administration could cause CDIviatwo ways: Firstly, the decreased clostridia and bacterioid will increase after carbapenem discontinuing[8]; Secondly,critically ill patients might also have been treated with other antibiotics before starting carbapenem. Such patients might have advanced infections and prolonged inflammation, which increases risks for CDI[2]. This study also showed that the administration of carbapenem in CDI positive patients was significantly higher than CDI negative patients (P<0.05). Cançadoet al.also reported that carbapenem resulted in increased CDI risk in ICU patients significantly[6]. In addition, Chianget al.revealed that carbapenem along with prolonged mechanical ventilation was an important risk factor for CDI[2]. Ebrahim-Saraieet al.found that carbapenems,cephalosporins, and fluoroquinolones were the most common antibiotics causing CDI[9]. Bartolettiet al.found that meropenem was more efficient than tigecycline[28]. However, recommendation by international database up-to-date is different from our findings.According to up-to-date (2020), clindamycin, fluoroquinolone, and cephalosporins are the most frequent antibiotics for developing CDI whereas carbapenem is not dominant[7].
Possible reasons for diarrhea include non-infectious diarrhea such as ileus, atonic bowel, and high infusion rate of feeding material[29].Other infectious infections (i.e.apart fromC. difficile) such as norovirus, toxigenic strains of clostridium perfringens,Klebsiella oxytoca,Staphylococcus aureus, andBacteroides fragilisare possible causes for diarrhea. However, they remain undefined due to limited available studies[30].
In this study, significant differences in age and APACHE II score between the case and the control group were not detected (P=0.936 and 0.225 respectively). The result also showed no significant difference in mortality. The high mortality in both groups was because that these patients are old with considerable underlying diseases. High mortality may be related to comorbidities, age,chronic underlying diseases, the severity of illness. And multicentre and prospective studies on mortality of CDI in ICU are needed.
Our study is a case-control study and focuses on endotracheal intubation, nasogastric feeding, and carbapenem use. There are some limitations in our studies. This study was carried out in a single center with limited laboratory facilities and with small sample size. Bigger sample size is needed for further study. Besides, most patients were old with multiple comorbidities, and that is why the death rate of both groups was very high. Finally, all medical records were obtained from our center and some factors such as previous antibiotic use might could be neglected.
Conflict of interest statement
The authors report no conflict of interest.
Acknowledgments
The authors acknowledge Somayeh Roshangaran, Neda Kadfar,Sakineh Takin, Masoumeh Jarban, and the staff working in the ICUs of Baharloo Hospital.
Authors’ contributions
M.A. and H.H. study design, data collection, data analysis, and manuscript preparation, and final edition. Y.A., S.A., L.M., A.K.N,M.S., M.N. had role in manuscript preparation and data analysis.
 Journal of Acute Disease2020年6期
Journal of Acute Disease2020年6期
- Journal of Acute Disease的其它文章
- Rectosigmoid perforation after high-pressure air jet exposure: A case report
- Acute ascites as a clinical manifestation of dengue: A case report
- Risk factors of COVID-19 infection among policemen: A case-control study
- Clinical features, management and outcomes of pediatric pleural empyema: A retrospective, multicenter cross sectional study
- A scoping review of vestibular paroxysmia: An acute disabling clinical entity
- Expert consensus on emergency diagnosis and treatment procedures for acute upper gastrointestinal bleeding
