A scoping review of vestibular paroxysmia: An acute disabling clinical entity
Santosh Kumar Swain, Nibi Shajahan, Satybrata Acharya
Department of Otorhinolaryngology, IMS and SUM Hospital, Siksha “O” Anusandhan University, K8, Kalinganagar, Bhubaneswar, 751003, Odisha, India
ABSTRACT The pathogenesis of vestibular paroxysmia (VP) is the neurovascular cross-compression of cranial nerve Ⅷ with short episodes of vertigo as the common symptom. The exact etiological and clinical profiles of the patients with VP are uncertainly reported in literature. It is general thought that loop of the anterior inferior cerebellar artery and posterior inferior cerebellar artery (less commonly), vertebral artery, or a vein is involved in compressing cranial nerve Ⅷ. Ephaptic neural discharges at the proximal end of cranial nerve Ⅷ, which is covered by oligodendrocytes, are thought to be the mechanism for VP. Patients with VP often suffer from brief vertiginous attacks of several episodes in a single day,and nystagmus is seen during the vertiginous episodes. Cranial magnetic resonance imaging could reveal the arterial compression of cranial nerve Ⅷ. The important differential diagnosis of VP includes vestibular migraine, Meniere’s disease, benign paroxysmal positional vertigo, superior canal dehiscence syndrome, epileptic vertebral aura, paroxysmal brainstem attacks (in multiple sclerosis or after brainstem stroke), transient ischemic attacks and panic attacks. The vertiginous attacks can be ceased by administration of a low dose of carbamazepine. Carbamazepine or oxcarbazepine, even in low doses, can be efficient to relieve VP, and they have the same efficiency both in adults and in children.
KEYWORDS: Vertigo; Vestibular paroxysmia; Neurovascular crosscompression; Carbamazepine
1. Introduction
Vestibular paroxysmia (VP) is an uncommon episodic peripheral vestibular disease causing acute or sudden brief attacks of vertigo or disequilibrium with or without the presence of auditory and vegetative clinical symptoms[1]. VP is a disabling clinical entity and a treatable etiology for vertigo with characteristic clinical presentations secondary to neurovascular compression of cranial nerve Ⅷ complex. VP was first described by Jannetta in 1975,who termed this disorder as disability positional vertigo[2]. The term “vestibular paroxysmia” was first coined by Brandtet al.in 1994[3]. The duration of vertigo lasts for a fraction of a second to few minutes with or without aural symptoms such as tinnitus, hypo,or hyperacusis. The frequent episodes of VP greatly trouble the daily life of patients. Pressure due to arteries or rare veins at the cerebellopontine angle causes a segmental dysfunction of cranial nerve Ⅷ. Neurovascular cross-compression of cranial nerve Ⅷleads to “disabling positional vertigo”[4]. The main symptom of the VP is frequent attacks of vertigo lasting for seconds to minutes,which occurs at rest time, in certain head positions. The symptom varies from positions and responds to low dose sodium channel blocking antiepileptic drugs such as carbamazepine[5]. Detailed patient history and imaging are helpful for the diagnosis. Magnetic resonance imaging (MRI) can reveal the neurovascular compression of cranial nerve Ⅷ. The majority of VP cases with disabling symptoms could be treated medically. The objective of this review is to familiarize readers with the complex and rare clinical entity of VP and its disabling symptoms.
2. Methodology
articles. The search term is paroxysmal vertigo. Abstracts were identified and analysed. The prevalence, etiopathology, clinical presentations, diagnosis, and current treatment of VP were reviewed and summarized.
3. Epidemiology
As VP is a rare disease (the incidence<1 per 2 000 persons), there is no adequate information regarding the incidence and prevalence of VP documented in the medical literature[6]. Similarly, there are little data available regarding the lifetime prevalence. This may be due to the poor documentation, non-availability of gold standard investigations for confirmation, and similar symptoms with other vestibular diseases. The mean age of VP patients was 51 years (range 25-67 years)[7]. The VP was also recorded in the pediatric age group with clinical presentations similar to adults.The children with VP have a good long-term prognosis with spontaneous remission with age. As far as we know, there is no epidemiologic evidence regarding a genetic contribution towards VP and sporadic studies regarding the symptom complex and audiovestibular outcome[8]. VP constitutes for 3.7% of 17 718 consecutive patients at the outpatient departments of the German center for vertigo and balance disorders[6]. The incidence of the vertigo episodes with changes of position or hyperventilation has been documented in 50% of the VP patients, where 28% of cases happened at the rest time while only 22% are with provocation[1].In approximately 75% of the VP patients, unsteadiness of the gait has been recorded[1]. The presence of sensorineural hearing loss along with vertigo has been documented in 50% to 95% cases of VP[9].
4. Etiopathology
Analogous to hemifacial spasm, trigeminal neuralgia, and glossopharyngeal neuralgia, the episodic vertigo of VP occurs due to neurovascular cross-compression of the vestibular cochlear nerve at the root entry area[3]. Aberrant or atherosclerotic dilated and elongated blood vessels at the cerebellopontine angle may lead to segmental pressure inducing central demyelination. A loop of the anterior inferior cerebellar artery is often involved, while the posterior inferior cerebellar artery and the vertebral artery or a vein is rarely engaged in the compression of cranial nerve Ⅷ.Besides, elongation and increased looping, vascular malformation,or ectasia of the artery at the posterior fossa can lead to cranial nerve Ⅷ compression. The variability of the severity reflects cranial nerve Ⅷ possesses different parts such as superior vestibular nerve,inferior vestibular nerve, and cochlear nerve. The mechanism for acute attack in VP is ephaptic depolarization. Repetitive pathological compression or pressure exerting to the nerve by a blood vessel is thought to provoke demyelination with succeeding hyperexcitability leading to ephaptic depolarization[10]. The vessels are mostly arteries, however, evidence has shown that neurovascular compression can also be caused by venous vessels[11]. The course of cranial nerve Ⅷ is divided into a central and peripheral part. The part of the cranial nerve between point of entry and site of its myelination is called the root entry zone. This root entry zone is myelinated by oligodendroglia. The root entry zone is also susceptible to developing neurovascular compression. Vestibular symptoms such as vertigo occur due to high degree of the impingement of the vestibular branch of cranial nerve Ⅷ. The long-standing cross-compression of the vestibular nerve may lead to “cross-talk” where the impulse travels through other neurons to cochlear nerve, resulting in tinnitus and higher loudness by fibers within a compressed cochlear nerve[12].Tinnitus is often described as “typewriter tinnitus”[12].
5. Clinical presentations and diagnosis
This neurovascular cross-compression syndrome may be relieved spontaneously because skull bone and vascularity of the brain grows at different rates[13]. The common symptoms of the VP are brief attacks of the spinning or non-spinning vertigo which stays for a fraction of second or a few minutes and associated with or without other aural symptoms such as tinnitus, hypo, and hyperacusis. The brief attacks occur 30 times or more per day. Arteries and veins(less) at the cerebellar pontine angle are the origin of the segmental pressure towards cranial nerve Ⅷ. The symptoms in VP are triggered by direct pulsatile compression and ephaptic paroxysmal transmission between neighboring inter-axonal nerves, and possibly leading to demyelinated axons[1]. Medical history, systematic clinical neurological examination, and neuro-otological examinations are required for assessment of the patients with VP. The mentioned examinations include positioning maneuvers, stepping test for vertigo or imbalance and gait examination with Frenzel’s glass for spontaneous nystagmus, head impulse test for pathological vestibuleocular reflex, head-shaking test for prevocational nystagmus,screening for central ocular motor diseases by testing saccades,smooth pursuit and fixation suppression of the vestibule-ocular reflex. Patients often present with short attacks of VP similar to the hemifacial spasm and trigeminal neuralgia. The VP and facial spasm may be seen through vascular compression of vestibular and facial root entry zone[14]. The clinical symptoms are aggravated by direct pulsatile compression of the artery. Auditory symptom during vertiginous attacks of the VP is an important reliable indicator of the affected side. Otological examinations show normal external ear and tympanic membrane. Tuning fork test shows sensorineural hearing loss in the affected ear. Neuro-otological examination reveals no spontaneous or gazes induced nystagmus. This disorder has negative impact on patient’s daily life and may lead to anxiety. It also has negative impact on family members of the patients, which might worry that it may lead to serious consequences such as brain tumors.As many clinicians are not aware of this condition, patients may be referred to different medical specialists and face several unnecessary investigations. The VP contributes approximately 4% of all the etiologies of vertiginous attacks at a referral center for vertigo and balance problems[1]. The frequent episodes of vertiginous attacks of VP greatly impair the children’s participation in social activities and lower his or her quality of life. In the course of the VP, measurable vestibular and/or cochlear dysfunctions progresses during the attack instead of the attack-free interval. The neurophysiological function tests include audiogram, caloric test, acoustic evoked potentials, and test for subjective visual vertical.
The following criteria are used or proposed for the diagnosis of the VP, such as (1) Brief attacks of rotational to- and fro vertigo with a duration of seconds to minutes; (2) Frequency of attacks dependent on the particular head positions; (3) Hypoacusis or tinnitus occurs continuously, or only during the attack period; (4) Measurable vestibular or auditory deficits by neurophysiological methods;(5) Effectiveness of carbamazepine[15]. The detail of the clinical diagnostic criteria was described by Hüfneret al.[16]. The diagnosis of VP is often based on typical history.
The International Classification of Vestibular Disorders has classified VP into two categories, namely definite VP and probable VP. This classification is useful for the diagnosis and response to medical treatment[17,18]. It is worth noting that the diagnosis is different for the two types of VP. The clinical diagnostic criteria of definite VP are as following: Patients suffers from a minimum of five vertigo attacks and fulfills one criterion of each category of (A)-(E). (A) Vertigo attacks: Vertigo attacks (rotatory as well as to and fro vertigo) with short duration (seconds to minutes), which cease spontaneously; (B) Vertigo triggers: Attacks occur in rest time,induced by a specific head and/or body position, or by a specific change of head and/or body position; (C) Accompanying symptoms:Attacks are accompanied by at least one of the following additional symptoms: Unsteadiness of stance and/or gait, lateralized tinnitus,decreased hearing function, or subjective sensory irritations, such as a feeling of pressure within or around one ear; (D) Additional criteria: The diagnostic procedures together with the anamnestic aspects reveal a neurovascular compression of cranial nerve Ⅷon MRI scans including constructive interference in steady-state sequences, hyperventilation-induced nystagmus, detectable progress of vestibular deficit over the course of the disease, or patients responded positively to treatment. (E) Exclusion: Any other possible pathology or disease explaining the symptoms are found. In probable VP, patients suffered from a minimum of five vertigo attacks and the fulfilled criterion (A) and additionally at least three criteria out of the categories (B)-(E).
6. Differential diagnosis
The patients of VP often present with brief and frequent paroxysms of vertigo. Before making the diagnosis of VP, several diseases should be excluded. The important differential diagnosis of the VP includes benign paroxysmal positional vertigo (BPPV),central positioning vertigo, Meniere’s disease, multiple sclerosis with the involvement of the brainstem, vestibular migraine, panic attacks, perilymph fistula, episodic ataxia type 2, and vertebral artery occlusion syndrome[19]. Positional maneuvers or Dix-Hallpike test are helpful for the diagnosis of BPPV. Regards to central positioning vertigo, it lasts as long as the position of the patient is maintained. In case of Meniere’s disease, the duration of vertigo stays for 20 min to 20 h. Carbamazepine is helpful for multiple sclerosis, and high-resolution MRI of brain can confirm the diagnosis of multiple sclerosis. Though a positive outcome supports the definite diagnosis of VP, the exact specificity of this drug response for confirming the diagnosis still needs to be proved.Vestibular migraine is often distinguished by related migrainous symptoms and never occurs as serious multiple episodes per day.In case of perilymph fistula, symptoms are usually aggravated by pressure change such as sneezing, coughing, heavy weight lifting,and loud noise. Episodic ataxia type 2 is usually associated with cerebellar signs and gazed evoked nystagmus and often seen in children. In case of vertebral artery occlusion syndrome, nystagmus is induced by constant head rotation on the left or right and can be confirmed by angiography. Multiple sclerosis often leads to brainstem paroxysmia with clinical symptoms similar to those of VP.Benign paroxysmal vertigo and vertebrobasilar artery insufficiency are also important causes for paroxysmal and brief vertigo, which can be excluded through the findings of the Dix-Hallpike test and magnetic resonance angiography. Meniere’s disease and vestibular migraine can be excluded from VP based on the patient’s history,clinical presentations, audiometric findings, and responsiveness to carbamazepine (Table 1)[18,20,21]. VP is a rare central vestibular disease which may respond to carbamazepine and can be excluded by the electroencephalography if it does not show epileptiform discharges.
7. Investigations
A battery of audiovestibular tests and MRI should be done in all patients of VP. MRI reveals labyrinthine artery loops around cranial nerve Ⅷ in the case of VP. The routine audiological evaluation includes pure tone audiometry and immittance evaluation. It reveals the hearing status of the patients and also rules out the middle ear problems. The incidence of sensorineural hearing loss has been documented in 50% to 100% of the patients[22]. The absence of hearing loss may be due to less or lack of impingement on the cochlear/auditory branch of cranial nerve Ⅷ. The presence of vestibular symptoms only indicates a higher degree of the impingement of the vestibular branch of cranial nerve Ⅷ. The auditory brainstem response (ABR), electronystagmography (ENG)/videonystagmography and MRI are often used for investigations for VP, however, the consensus regarding the result or findings are absent. The abnormality report in ABR has been documented,which ranges from 0% to 85%[21,23]. In VP patients, ABR shows prolongation ofⅠ-Ⅲ inter-peak latency which is the common finding. ENG report abnormality is seen in approximately 93%of the patients with VP[24]. The ENG test shows unilateral caloricweakness and spontaneous nystagmus. It also shows positive results for positional vertigo in Dix-Hallpike maneuver. The Dix-Hallpike test shows positional vertigo which is different from BPPV. However,the BPPV is not associated with abnormalities in optokinetic test and Gaze[25]. The vestibular evoked myogenic potential often reveals lower amplitude in affected ear. MRI documentation of the neurovascular cross-compression of cranial nerve Ⅷ supports the diagnosis of VP (100% sensitivity in adult age). However, the diagnosis of the VP is based on clinical presentations[26]. In adult persons, the data indicates insufficient specificity for neurovascular cross-compression in MRI (65%)[27]. MRI is helpful to rule out vestibular schwannoma which also can cause vertiginous attacks,as well as central pathologies like multiple sclerosis. Both highresolution 3D T2-weighted imaging with 3D time-of-flight angiography and 3D T1-weighted gadolinium-enhanced sequences are highly useful for detection of neurovascular compression. This combined tool can be a successful guide for this neurosurgical intervention and also predict the treatment outcome[28].
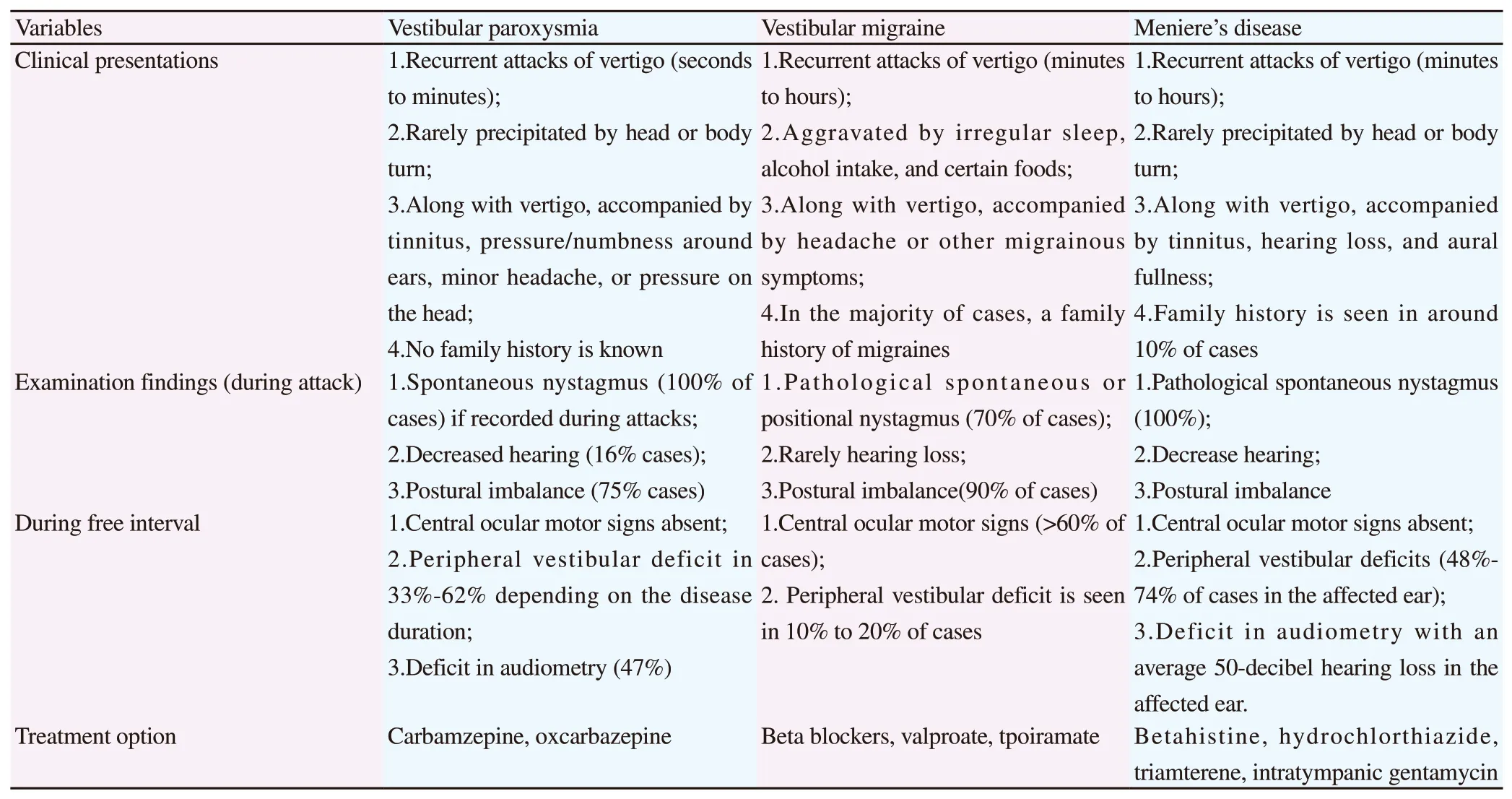
Table 1. Differential diagnosis of the vestibular paroxysmia[19,21,22].
8. Treatment
The medical treatment of VP with a low dose of carbamazepine(200-600 mg/d) or oxcarbazepine (300-900 mg/d) is often effective[29]. Though a positive outcome supports the definite diagnosis of VP, the exact specificity of this drug response for confirming the diagnosis still needs to be proved. One study on the progress of the disease in 32 patients who took carbamazepine or oxcarbazepine for three years revealed a decrease in the attack frequency (lowered to 10%) and a reduction in the severity and duration of the attack[30]. If these drugs fail to respond, other sodium channel blockers like phenytoin or valproic acid will be alternative options, however, there are rare studies available to support this opinion. VP is a medically treatable disease of disabling positional vertigo, and surgery is rarely indicated. The effectiveness of the micro-vascular decompression in cranial nerves Ⅴ, Ⅶ, Ⅸ, has been well-proved in medical practice. There are few centers are doing micro-vascular decompression of the eighth cranial nerve such as superior or inferior vestibular nerve at its entry zone. Micro-vascular decompression leads to relief of the vertigo in majority of the cases where medical treatment fails. The surgical treatment in the form of the micro-vascular decompression similar to that of the trigeminal neuralgia or hemifacial spasm is done for intractable cases of VP.The micro-vascular decompression should be avoided as, on the one hand, there is a chance of brainstem infarction because of the intraor postoperative vasospasm and on the other hand, it is often difficult to decide the affected-side with certainty[29].
9. Conclusion
VP is a rare cause of vertigo which attributes to neurovascular cross-compression of the eighth cranial nerve leading to vertiginous spells. The diagnosis of the VP is often missed by clinicians because of its rarity, similarity to other peripheral and central causes for vertigo, and episodic type of vertigo with the absence of clinical findings. A detailed patient history, neuro-otological examination and imaging will rule out probable differential diagnosis and reach to correct diagnosis. The affected side is often difficult to determine unless associated with cochlear symptoms or other cranial nerves involved such as facial nerve. High-resolution MRI often confirms the side of the lesion. The goal of the treatment is to control vertigo.Vertigo is the most disabling symptom of VP managed commonly by medical treatment. Micro-vascular decompression is reserved for intractable vertigo with caution.
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contributions
S.K.S. conceived the concept, collected data. S.K.S., N.S., and S.A.interpreted data and prepared the manuscript. All authors read and approved the final manuscript.
 Journal of Acute Disease2020年6期
Journal of Acute Disease2020年6期
- Journal of Acute Disease的其它文章
- Rectosigmoid perforation after high-pressure air jet exposure: A case report
- Acute ascites as a clinical manifestation of dengue: A case report
- Risk factors of COVID-19 infection among policemen: A case-control study
- Risk factors of Clostridium difficile infection in ICU patients with hospital-acquired diarrhea: A case-control study
- Clinical features, management and outcomes of pediatric pleural empyema: A retrospective, multicenter cross sectional study
- Expert consensus on emergency diagnosis and treatment procedures for acute upper gastrointestinal bleeding
