Super-minimal incision kidney transplantation: Report of 6 cases
De-Sheng Li, Yi Wang, Jian Xu, Shan-Bin Zhang, Hong-Tao Jiang, Hou-Qin Liu, Liang Xu, Hui-Ling Gan, Fan-Jun Zeng
Department of organ transplantation; The second Affiliated Hospital of Hainan Medical University Haikou, 571000 China
Keywords:Super-minimal incision Kidney transplantation
ABSTRACT Objective: TReport of 6 cases super-minimal incision kidney transplantation, to further explore its application in renal transplantation. Method: We reviewed the clinical data of 6 cases of SMIKT: operative time, incision size, postoperative pain score, scar score and renal function 1 month after operation. Result: The average operation time of 6 recipients was 95 ± 33min, the average incision size was 6.1 ± 1.1cm, the average pain scores of three days after operation were2.7±0.7, 2.2±0.3, 2.3±0.5. postoperative analgesia with analgesia pump, no use on the second day, one month after operation, the scar score was 6.85 ± 0.58, and the serum creatinine was 98 ± 16umol/L. Conclusion: The length of incision in the study SMIKT was short, little harm to patients, for the receptor with BMI < 25kg / m2, this method can be used. At the same time, the current sample capacity of the study was small and the follow-up time was short, more samples will be needed to enrich the data and further prove its advantages in the future.
1. Introduction
In recent years, with the development of science and technology, kidney transplantation has become the most effective treatment for end-stage renal disease. Since Joseph Murray successfully completed the first renal transplantation in 1954[1], the traditional open surgery has been the mainstream operation, the minimally invasive technique marked by laparoscopic application has revolutionized the operation mode of urology, but the progress of renal transplantation is not obvious[2]. In 2006, Oyen et al[3]. first tried the minimally invasive kidney transplantation (MIKT), later, Kim et al、And kacar et al, also made similar MIKT attempts[4-5]. Similar attempts have been made in China.In July 2018, song tourun, Zeng fanjun, Lin Tao, etc[6]. reported 40 cases of super small incision kidney transplantation (SMIKT) and achieved good results. They mentioned SMIKT for the first time. Under the leadership of Professor Zeng fanjun, our department started to carry out similar SMIKT operation in December 2018, and made relevant attempts. At present, 6 cases of SMIKT have been completed,the preliminary results are summarized as follows:
2. Materials and methods
2.1 Clinical data
We collected 6 patients who received SMIKT from December 2018 to February 2020, with body mass index (BMI) less than 25kg / m2, 4 males and 2 females, aged 23-56 years, with an average age of 39.4 years. All of them had no history of hepatitis, tuberculosis, malignant tumor and other urinary system diseases. The serum creatinine was 723-1631 umol / L, and urea nitrogen was 15.7-39.0 mmol / L. all of them were diagnosed as uremia. The donor kidneys were from 2 relatives and 4 from (Donation after Citizens Death) DCD.
2.2 Surgical technique
2.2.1. Repair of donor kidney
In order to shorten the warm ischemia time, the donor kidney can not be dissociated carefully, so it needs to be trimmed before it can be used for kidney transplantation. It mainly includes the separation of left and right kidneys, the dissociation of artery and vein, and the repair of ureter. The detailed process can be seen in the references[7]. When repairing the kidney, try to remove the fat sac around the kidney and the extra adipose tissue in the hilum area. Carefully ligate the small branches of arteriovenous and the small vessels in the hilum area. The adipose tissue and mesentery around the lower pole of the kidney and the ureter should be retained as far as possible, otherwise the blood supply of the ureter will be affected.
2.2.2. Donor kidney operation
From about 1cm above the junction of bilateral anterior superior iliac spine and the external edge of rectus abdominis, a 5-6cm long oblique incision was made along the outer edge of rectus abdominis (see figure A). (the size of surgical incision was determined according to the transverse diameter of donor kidney). In general, the right incision was used to cut the skin and subcutaneous fat, then the external oblique muscle and the internal oblique muscle fascia were cut in turn, and then entered the iliac fossa at the junction of transverse abdominal muscle and fascia. Pay attention to avoid damage to the peritoneum, cut off the inferior abdominal wall artery and vein, and fully free the spermatic cord (male) or round ligament of uterus (female), bluntly push to the medial side to separate the peritoneum and expose the iliac vessels. The internal iliac artery or external iliac artery was selected as the donor renal artery according to the conditions of the donor and recipient vessels, and the external iliac vein was selected as the reflux vein. The internal iliac artery or external iliac artery and external iliac vein were fully dissociated to take the repaired kidney graft. ① Arterial anastomosis: end to side or end-to-end anastomosis was performed between the transplanted renal artery and the right external iliac artery or internal iliac artery. 6-0 Prolene non-invasive vascular suture was used for continuous suture (see Fig B). ② Venous anastomosis: end to side anastomosis was performed between the renal vein and the external iliac vein, and the 5-0 Prolene non-invasive vascular suture was used for continuous suture (see Fig C). To open the blood flow, the vein should be opened first, and then the artery should be opened. Carefully check whether there are active bleeding points on the surface of the transplanted kidney and the renal hilum area, and then ligate them (see Fig.D and E). ③ Reconstruction of the ureter: after exposing the bladder, the serosa layer and muscular layer were cut about 2cm in turn, and the mucosa layer was exposed, and a small incision was made. The ureter and bladder mucosa were sutured intermittently with 5-0 absorbability, and the ureter was embedded for about 2cm (see Fig. F and G). The drainage tube around the transplanted kidney was placed in the iliac fossa, and the abdominal wall was sutured.
2.3. Immunosuppressions and postoperative managements
Antibody induction (Baliximab) or Rabbit anti human thymocyte immunoglobulin (i.e. Funing) + adrenocortical hormone(Prednisolone) was used in the early postoperative immunosuppression regimen, and then Tacrolimus + Mycophenolate mofetil capsules (Xiaozhi) or Mycophenolate sodium enteric coated tablets (MIFF) + Prednisone were used for maintenance. Patients were encouraged to get out of bed early, and analgesia was given at the same time. The analgesia pump (sufentanil 150ug + tropisetron 5mg + saline 100ml) lasted for 2-2.5ml/h, and 0.5-1ml/time was added for a single time, and the interval was 15min. Generally, it was stopped the next day after operation.
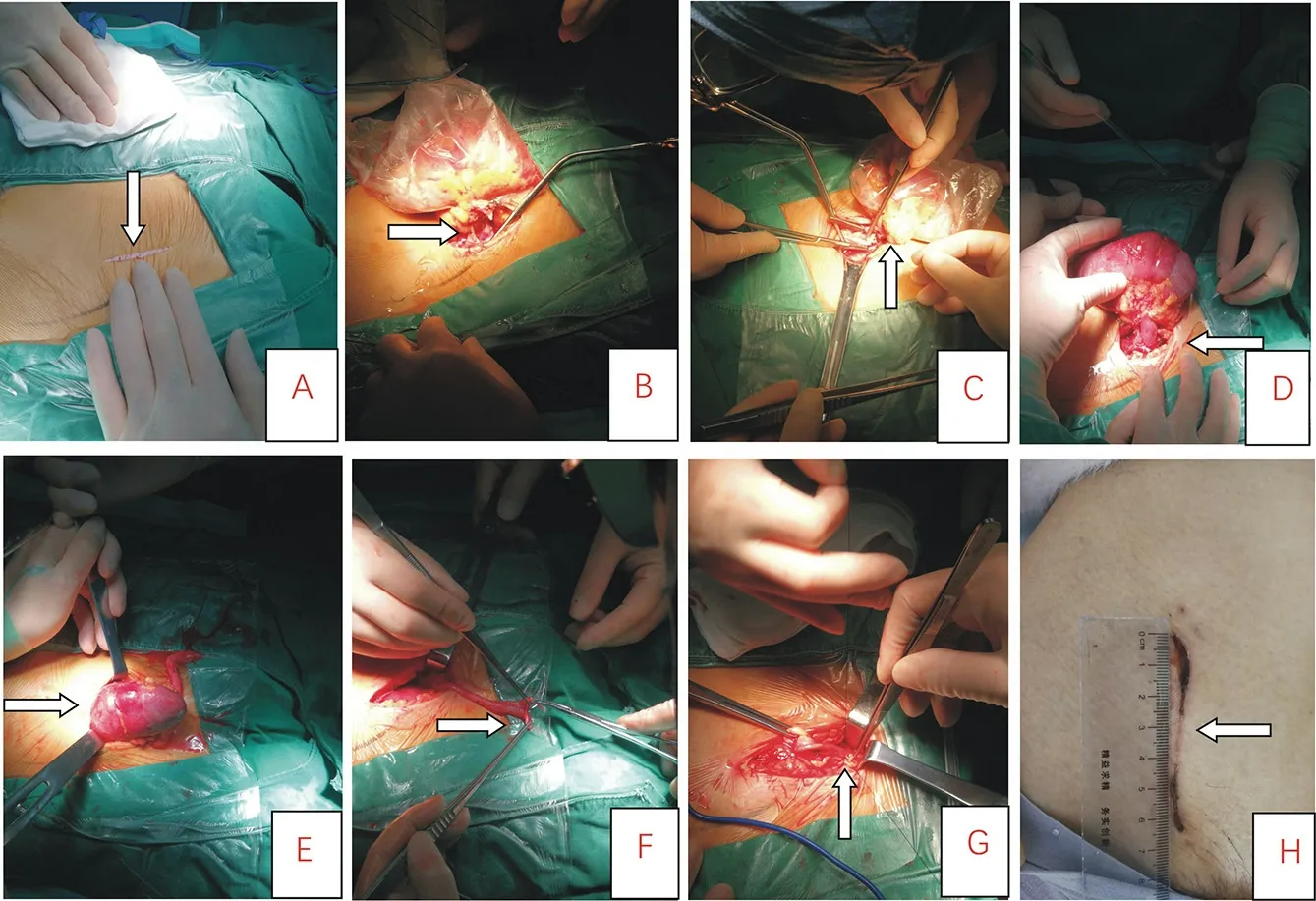
FigureA: shows the operation incision as shown by the arrow; figure B:shows the renal artery anastomosis; figure C :shows the renal graft vein anastomosis; figure D :shows the transplanted kidney and its filling arteries and veins after the blood flow is opened; figure E:shows the transplanted kidney has been put into the abdominal cavity; figureF: the correction of ureter; figure G: ureteral anastomosis; figure H: surgical incision 15 days after renal transplantation.
3. Result
The average age of 6 recipients was 39.4 years old, and the average BMI was 20.6 kg / m2. After the blood flow was opened, the transplanted kidney was filled rapidly and the renal artery pulse was good. The average cold ischemia time of donor kidney was 3.3 ± 1.2 h, the average operation time was 95 ± 33 min, the average intraoperative blood loss was about 75 ± 25 ml, and the average urinary time was 3 ± 2 min. The pain score on the day of operation was 2.7 ± 0.7, the pain score on the first day after operation was 2.2 ± 0.3, and the pain score on the second day after operation was 2.3 ± 0.5 (the analgesic pump had been stopped), and the pain score did not increase significantly. All the incisions healed in one stage,no fat liquefaction was found,the average incision length was 6.1 ± 1.1cm.Color Doppler ultrasound showed that the transplanted kidney and renal vessels had no obvious abnormality. One month after operation, the Vancouver Scar score was 6.85 ± 0.58. During the follow-up of more than 1 month, no DGF and acute rejection occurred in the transplanted kidney, and the function of the transplanted kidney recovered well, with an average creatinine of 98 ± 16umol / L.
4. Discussion
With the development of science, surgical technology and instruments have made great progress. The concept of minimally invasive surgery has been deeply rooted in all fields of surgery. Kidney transplantation technology is widely accepted by people. At present, the commonly used methods of kidney transplantation are as follows: 1. Open kidney transplantation: ① traditional operation is Gibson incision or hockey stick incision; ② small incision renal transplantation; 2. Minimally invasive kidney transplantation, such as robot assisted laparoscopic kidney transplantation RKT: ① robot assisted laparoscopic total extraperitoneal renal transplantation; ② robot assisted laparoscopic total intraperitoneal renal transplantation. Despite the rapid development of minimally invasive surgical techniques and transplantation immunity in the field of renal transplantation, the progress is not obvious as far as kidney transplantation itself is concerned[2]. At present, the traditional Gibson incision is still the main and mainstream way of kidney transplantation. As a traditional open surgery, its incision is long and the wound surface is large. In addition, the application of postoperative immunosuppressant can further improve the incidence of surgical complications such as incision infection and poor wound healing. In recent years, some scholars began to try minimally invasive renal transplantation, including robot assisted laparoscopic renal transplantation (RKT). In theory, small incision renal transplantation does not belong to the scope of minimally invasive renal transplantation, but it has its advantages and disadvantages compared with RKT. Scholars at home and abroad have also made relevant attempts. In 2006, Oyen et al. [3] tried MIKT for the first time, followed by Kakar et al[4]. also made similar attempts, both of which did not limit BMI. Kim et al[5]. limited the patients with BMI < 25 kg / m2 to receive MIKT. Song tourun, Zeng fanjun, Lin Tao et al[6]. in 2018 also considered that the BMI value of SMIKT was less than 25 kg / m2. Compared with the traditional Gibson incision, SMIKT can significantly shorten the operation time, reduce the postoperative pain and analgesic drug use, and the short-term incision cosmetic effect is significantly better, and achieves good clinical effect. The inclusion criteria were BMI < 25 kg / m2and the average BMI was 20.6 kg / m2. The main consideration is BMI > 25 kg / m2, the receptor is too fat, the surgical field is not easy to be exposed, it is difficult to complete the ultra-small incision[8].
In recent years, robot assisted laparoscopic renal transplantation (RKT) has been reported at home and abroad. In 2002, hoznek et al[9]. for the first time applied robot assisted laparoscopic technology in renal transplantation. After that, there were relevant reports at home and abroad. In the early stage of RKT, due to the long time of vascular anastomosis, no local hypothermia protection measures were taken, and the long warm ischemia time could affect the function of transplanted kidney. In 2014, Menon et al[10]. performed RKT under hypothermia protection for the first time. The average renal surface temperature of 50 recipients was 20.3 ℃, and the average length of abdominal incision was 6.1cm. RKT is usually operated through abdominal cavity, which has large space and clear anatomical structure. It is more advantageous for high BMI receptor, especially BMI ≥ 30kg / m2. However, there are some risks in the intraperitoneal approach: ① there are many visceral organs in the abdominal cavity which are easy to move, and the transplanted kidney will be greatly affected, which may lead to renal torsion after operation; ② percutaneous renal transplantation puncture may damage the abdominal organs; ③ intraperitoneal approach is easy to affect the intestinal function during RKT. In 2014, Tsai et al[11]. also reported that RKT was performed via the extraperitoneal route, the abdominal incision length was 7.7 ± 1.04cm, which could avoid the influence of hypothermia on the function of abdominal organs. However, the extraperitoneal space was narrow and the visual field was poor, so it was not recommended to use high BMI receptor. Zhao Jianming, Zhang Xu et al [12]. also reported 3 cases of extraperitoneal RKT, the length of abdominal incision was about 8 cm. In this study, SMIKT was used. The incision length was 6.1 ± 1.1cm, which was close to the abdominal incision length of laparoscopic surgery. At the same time, there were more than three trocar incisions in laparoscopy, which resulted in greater overall damage and higher cost of robotic laparoscopic surgery.
In this study, the grafts were preserved in plastic bags containing appropriate amount of ice chips, and vascular anastomosis was performed in vitro to avoid the warm ischemia damage during the process of anastomosis. The surface temperature of transplanted kidney could be guaranteed at 0-4 ℃, which is better than RKT with low temperature protection measures (the average surface temperature of RKT grafts were 20.3 ℃). Meanwhile, it is necessary to repair the kidney carefully and fully free the donor renal artery and vein. The perirenal fat should be removed carefully. On the premise of maintaining its integrity, the redundant part should be removed as much as possible to reduce the difficulty of kidney transplantation. When the blood flow was opened, the vein should be opened first, and the artery should be opened immediately when there was no obvious bleeding (this is different from that reported by Professor Song tourun and Professor Lin Tao). After careful hemostasis, the transplanted kidney should be placed vertically into the iliac fossa after careful examination without obvious bleeding point. It is emphasized here that hemostasis must be careful to ensure that there is no obvious bleeding point.Once the transplanted kidney was put into the iliac fossa, it could not be taken out unless the incision is extended. Once the incision was extended, it is against the original intention of this study. Therefore, it was necessary to ensure that the donor kidney had no obvious bleeding point before insertion, and the arteriovenous examination was required after insertion Whether there was distortion, compression, etc.
In conclusion, this study basically achieved its purpose. Compared with traditional Gibson, SMIKT had advantages of shorter incision length and less damage to patients; compared with RKT, its incision length was also relatively close, but this study also had its limitations. It was necessary to select recipients with BMI < 25kg / m2, and abdominal endoscopic kidney transplantation had more advantages for recipients with BMI > 25kg / m2. At the same time, the sample size of this study was small .In the future, more samples will be needed to enrich the data to further prove its advantages.
 Journal of Hainan Medical College2020年15期
Journal of Hainan Medical College2020年15期
- Journal of Hainan Medical College的其它文章
- Mechanism of Duhuo Jisheng Decoction based on bioinformatics and network pharmacology in treating osteoporosis of kidney Yin deficiency
- Clinical features and prognosis of patients with novel coronavirus pneumonia complicated with diabetes
- A nomogram of 5-year risk of type 2 diabetes in Chinese population
- Yiqi Huoxue Decoction in the treatment of Qi and yin deficiency and stasis type diabetic nephropathy in stage Ⅲ and its effect on VEGF and TGF-β1
- Relationship between nap and hypertension in adults: An updated meta-analysis
- A meta-analysis of the safety of clopidogrel and tegrarol in patients with non-ST elevation acute coronary syndrome after PCI in China
