Relationship between nap and hypertension in adults: An updated meta-analysis
Meng-Yang He, Yao Yang, Yi-Ting Guo, Qiu-Hui Tian, Yu-Qing Zhu✉
1. Graduate School of Beijing University of Chinese Medicine, Beijing 100029, China
2. China-Japan Friendship Hospital , Beijing 100029, China
Keywords:Nap Hypertension Meta-analysis
ABSTRACT Objective: We aimed to investigate whether nap is associated with an increased risk of hypertension through a comprehensive meta-analysis. Methods: Literature retrieval, research selection and data extraction were done independently and in duplicate. Effect-size estimates are expressed as risk ratio (RR) and 95% confidence interval (CI). Results: Summary data from 13 articles, involving a total of 119501 adults, were meta-analyzed. The overall analysis showed that in the included articles, when the factors were not adjusted, there was a significant association between nap and hypertension (RR=1.11,95%CI:1.02 to 1.21, P=0.013). After adjusting the possible confounding factors, nap was still correlated with hypertension (RR=1.07, 95% CI: 1.01 to 1.14, P= 0.041). In the subgroup analysis, there was a significant association between nap and hypertension in women (RR=1.13, 95% CI: 1.04 to 1.22, P=0.004), but this relationship was not recurred in men. And there was a significant association between nap and hypertension in people ≥ 45 years old (RR=1.16,95%CI:1.08 to 1.24, P < 0.001). In the dose analysis, it was found that there was a significant association between high blood pressure and the population with nap duration ≥ 90 minutes (RR=1.13, 95% CI: 1.01 to 1.27, P= 0.04). Conclusion: Our meta-analysis results show that nap is a risk factor for hypertension, which is more obvious in women, and the difference is statistically significant. In the elderly people, nap is a protective factor for hypertension.
1. Introduction
Hypertension is the leading preventable risk factor for cardiovascular disease and all-cause mortality worldwide. As of 2010, a total of 1.38 billion people (31.1% of the global adult population) had hypertension, which increased the risk of heart disease, stroke and kidney failure[1].The global prevalence of hypertension is on the rise[2]. The 2018 revision of China's guidelines for the prevention and treatment of hypertension showed that the crude prevalence rate of hypertension among residents aged 18 and over in China from 2012 to 2015 is 27.9%, and the prevalence rate is generally increasing.
Nap is a common behavior habit in many countries. In an international survey comparing the sleep habits of adults in six different countries, the United States and Japan had the highest proportion of nap. However, even though nap has exerted an imperceptible influence on the ordinary people, there is still no consensus on whether or how chronic physical and mental diseases are related to nap. Some studies had pointed out that most chronic diseases are independently related to nap [3].However, the relationship between nap and high blood pressure is not often reproducible. Some studies suggested that nap increased the risk of high blood pressure[1, 4, 5]. On the contrary, other studies have shown that nap can reduce the incidence of high blood pressure [6, 7].
To yield more information for future studies, we synthesized the results of published studies conducted in the adults, aiming to evaluate the possible dose-response association between nap and hypertension. Meanwhile, we also intended to explore possible causes of heterogeneity between studies.
2. Materials and Methods
2.1 Search Strategy
We completed literature search by scanning VIP database, CNKI, Wanfang database, PubMed, EMBASE and Web of Science databases as of January , 2020. The following medical topic terms are used:(nap OR napping OR sleep OR siesta OR naps OR wu jiao [Title/Abstract],AND blood pressure OR hypertension OR hypertensive [Title/Abstract])We also scanned the reference lists of retrieved articles and systematic reviews to avoid potential missing hits.
Two investigators independently reviewed all retrieved articles, and, they carefully evaluated preliminary qualification based on their titles or abstracts and full texts if necessary.
2.2 Inclusion/Exclusion Criteria
The inclusion criteria were as follows: 1)Observational studies published as original studies or conference abstracts to assess the risk of hypertension in adult nappers. 2)There are clear diagnostic criteria for hypertension. Hypertension is defined as systolic blood pressure ≥ 140mmHg or diastolic blood pressure ≥ 90mmHg.3)studies that presented data to calculate odds ratios, relative risks or hazard ratios with 95% confidence intervals (CIs). 4)a reference group composed of individuals with no history of taking naps.
Exclusion criteria: 1)Repetitive studies.2)Diagnostic, therapeutic and non-adult studies.3)Results without detailed data.4)Case reports/series, editorials, and narrative comments.
2.3 Data Extraction
Two investigators independently extracted data from each qualified article, and typed them into a standardized Excel spreadsheet, including name of the first author, year of publication, country where study was conducted, sample size, sex, baseline age, ascertainment of nap,, adjusted confounders, nap duration, effect estimation, and other traditional risk factors, if available.
2.4 Statistical Analysis
We used the Stata software version 14.1 for Windows (StataCorp, College Station, TX) to manage and analyze data. Irrespective of the magnitude of between-study heterogeneity, the random-effects model was employed. Effect size estimates are expressed as relative risk (RR) and its 95% confidence interval (CI). The inconsistency index (I2) is used to assess heterogeneity between studies, and it represents the percentage of diversity observed between studies that results from chance rather than an accidental result. If I2 value is greater than 50%, significant heterogeneity is recorded, and a higher value indicates a higher degree of heterogeneity. Because of diverse sources of heterogeneity possibly from clinical and methodological aspects, a large number of prespecified subgroups were analyzed according to baseline age, sex, region, race, follow-up, short sleep duration and long sleep duration, respectively.
The probability of publication bias was evaluated by both Begg’s funnel plots and Egger regression asymmetry tests at a significance level of 10%. The trim-and-fill method was used to estimate the number of theoretically missing studies.
3. Results
3.1 Eligible Studies
After searching prespecified public databases using predefined medical subject terms, a total of 798 articles were initially identified, and 13 of them with data on nap and hypertension were eligible for inclusion, including 119501 adults in the final analysis. The detailed selection process and the specific reasons for exclusion are schematized in Figure 1. Since most articles provided data according to different age groups at baseline or follow-up periods, they are processed separately in subgroup analyses.
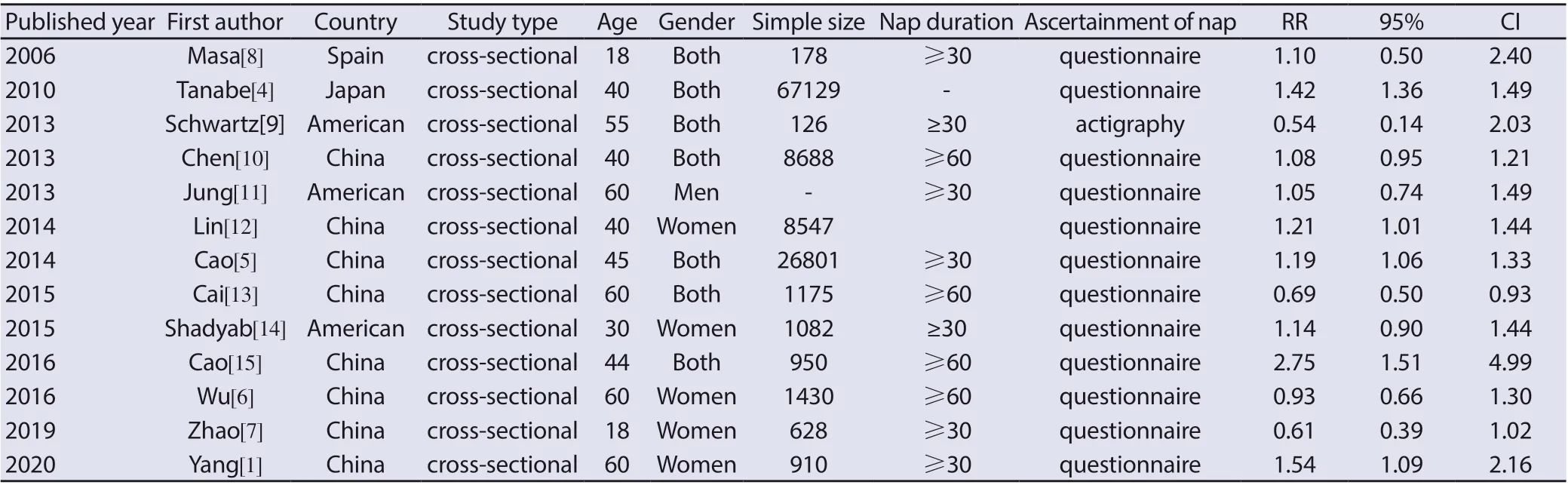
Table 1 The baseline characteristics of all involved studies in this meta-analysis.

Figure 1: Flow chart of records retrieved, screened and included in this meta-analysis.
3.2 Study Characteristics
Table 1 shows the baseline characteristics of each qualified study in this meta-analysis. Among the 13 eligible articles, The studies of Yang, Cao, Wu, Jung, Cai [1, 5, 6, 11, 13] focused on the relationship between siesta and hypertension in middle-aged and elderly people. The age range of the people included in the rest of the articles is large. The study of Yang, Tanabe, Wu, Zhao, Jung[1, 4, 6, 7, 11] separately analyzed the correlation between male and female populations included in the study. Yang[1] also analyzed the correlation between siesta and hypertension in middle-aged and old men and in middle-aged and elderly women. Schwartz[9] used a body motion recorder to record the length of their siesta, and the rest of the articles were conducted in the form of a questionnaire. Lin, Shadyab [12, 14] have only analyzed the correlation between nap and the risk of hypertension in women. Except for the studies of Tanabe[4] and Lin [12], other articles have a clear description of the length of siesta. Among them, the descriptions of nap data in the studies of scholars such as Tanabe, Masa, Chen, Jung, Lin[4, 8, 10-12]were relatively mixed, so some datas refered to the data in the meta-analysis written by Cheungpasitpor[16].
With regard to the baseline age, according to the population included in each article, the study divided them into three groups: the young, middle-aged and elderly group ≥ 18 years old, the middleaged group ≥ 45 years old and the elderly group ≥ 60 years old. As far as the region is concerned, all the articles included in this study are divided into three groups according to their geographical location: Schwartz, Jung, Shadyab[9, 11, 14] three articles were divided into America, The study of Masa [8] was divided into Europe. The articles of Yang, Tanabe, Cao, Wu, Zhao [1, 4-7, 10, 12, 13, 15] was divided into Asia.
Table 2 is the quality evaluation included in the articles. The methodological quality of the studies included was assessed using an 11-item checklist which was recommended by Agency for Healthcare Research and Quality (AHRQ). An item would be scored ‘0’ if it was answered ‘NO’ or ‘UNCLEAR’; if it was answered ‘YES’, then the item scored ‘1’. Article quality was assessed as follows: low quality = 0—3; moderate quality = 4—7; high quality = 8—11.
Abbreviations:①Define the source of information (survey, record review) ②List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications.③Indicate time period used for identifying patients.④Indicate whether or not subjects were consecutive if not population-based.⑤Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants⑥Describe any assessments undertaken for quality assurance purposes(e.g.,test/retest of primary outcome measurements)⑦Explain any patient exclusions from analysis.⑧Describe how confounding was assessed and/or controlled.⑨If applicable, explain how missing data were handled inthe analysis.⑩Summarize patient response rates and completeness of data collection. ⑪Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or followup was obtained.
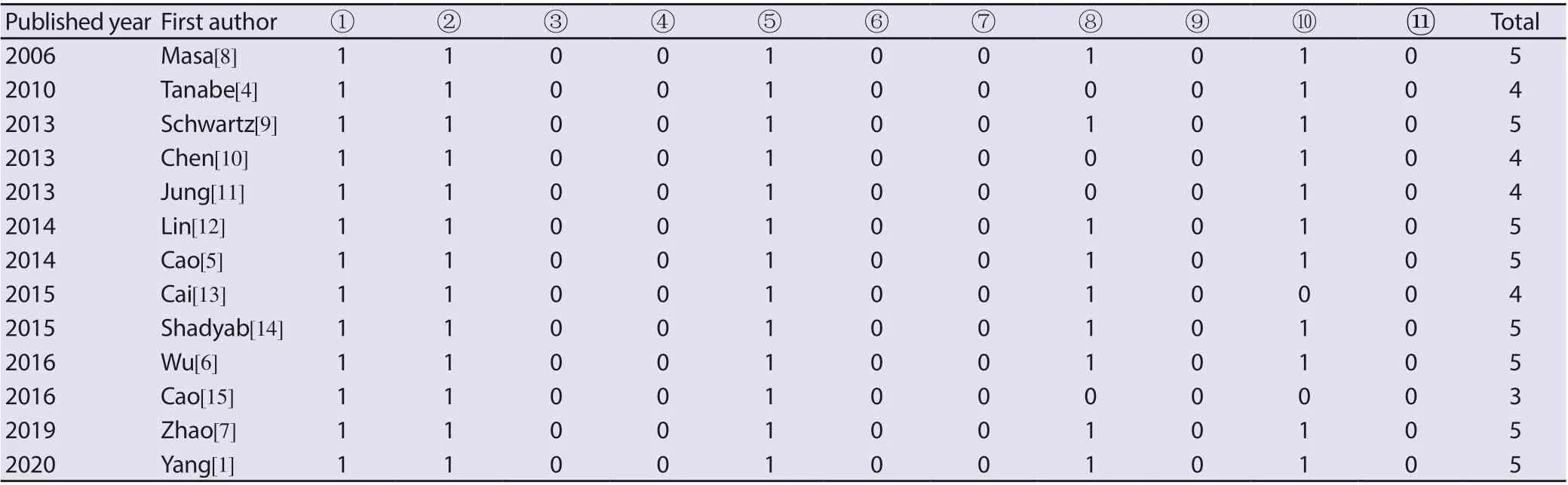
Table 2 AHRQ cross-sectional study evaluation criteria.
3.3 Publication Bias
Figure 2 shows the Begg’s funnel plots to assess publication bias for the association of nap with hypertension, and the plot o seemed symmetrical. This correlation is overshadowed by significant interstudy heterogeneity because the I2value of the overall analysis is more than 50%.The probability of Begg test showed that there was no evidence of bias between nap and hypertension (P < 0.12), but the probability of Egger test showed that there was a bias between siesta and hypertension risk.The possibility of publication bias suggests that negative studies are not excluded between siesta and the risk of high blood pressure.
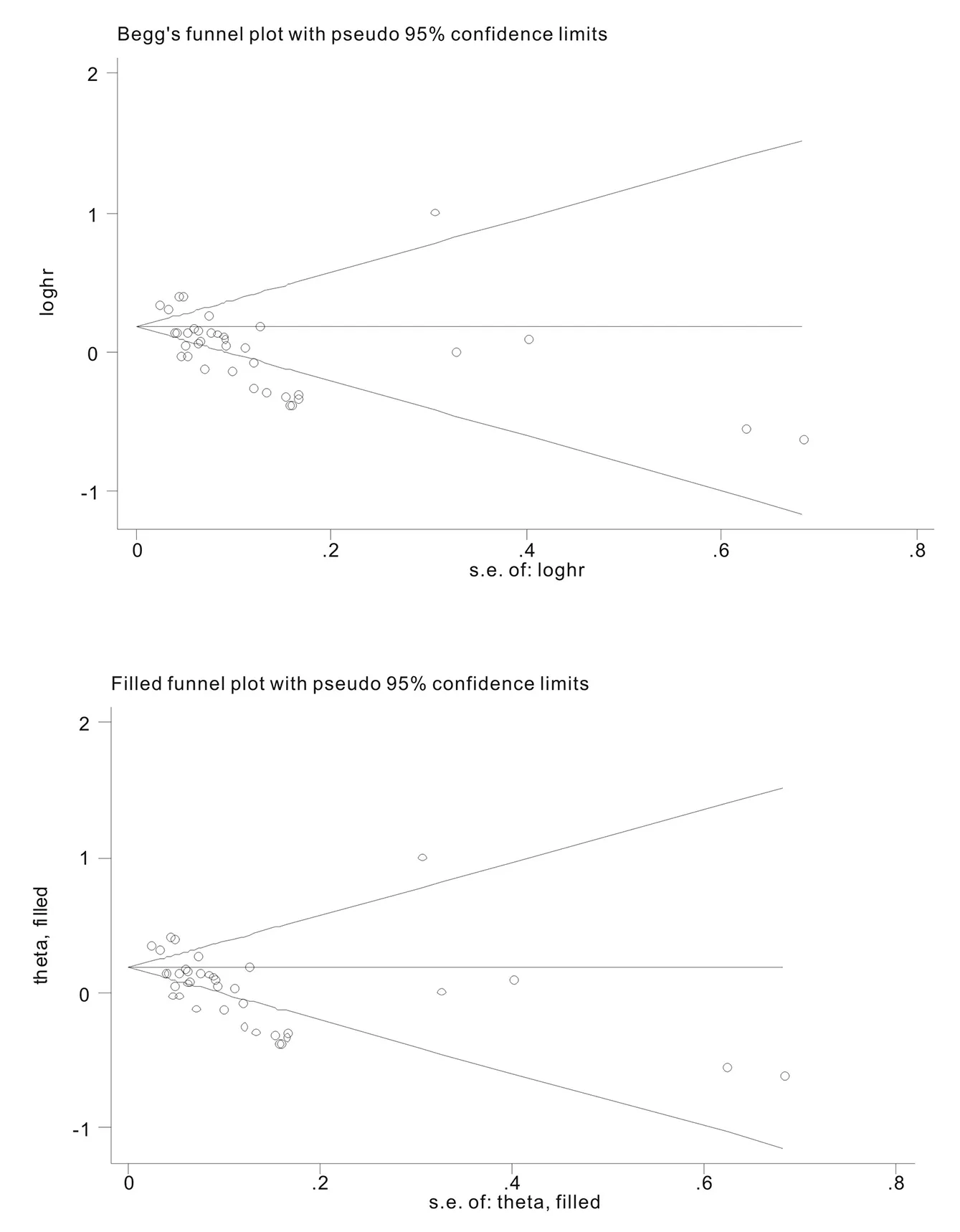
Figure 2. Begg’s and filled funnel plots on the association of nap with hypertension
3.4 Overall and Subgroup Analyses
After summing up the results of all qualified articles, Table 3 showed that the unadjusted effect between nap and hypertension is estimated to be 1.11 (95% CI: 1.02-1.21), indicating that there is a significant association between them, but there is still a significant correlation between them after adjusting for confounding factors (RR=1.07,95%CI:1.01-1.14,P=0.041).
Because the I2 value showed heterogeneity in the study, a series of subgroup analyses were carried out in this study (Table 3). In the gender subgroup analysis, there was a significant correlation between nap (RR=1.13,95%CI:1.04~1.22, P=0.004) and hypertension, but no such association was found in men.
By geographic locations, the association of nap with hypertension was stronger in Asia (RR=1.07, 95% CI: 1.00-1.15,P=0.048) than in Europe (RR=1.10,95%CI:0.5~2.41, P=0.812) and America(RR=1.09,95%CI:0.93~1.27).
In the subgroup analysis of age, there was a significant correlation between nap and hypertension in people ≥ 45 years old (RR=1.16,95%CI:1.08~1.24, P < 0.001). There was also a significant correlation between siesta and hypertension in people ≥ 18 years old (RR=0.78,95%CI:0.66~0.92, P=0.004) and ≥ 60 years old (RR=0.87,95%CI:0.75~1.00, P=0.044).
In dose analysis, data analysis showed that there was a significant association between nap and hypertension (RR=1.13,95%CI:1.01~1.27,P=0.04) in the group of greater than or equal to 90 minutes, but there was no significant difference among ≤ 30 minutes, 30 to 60minutes and 60 to 90minutes.
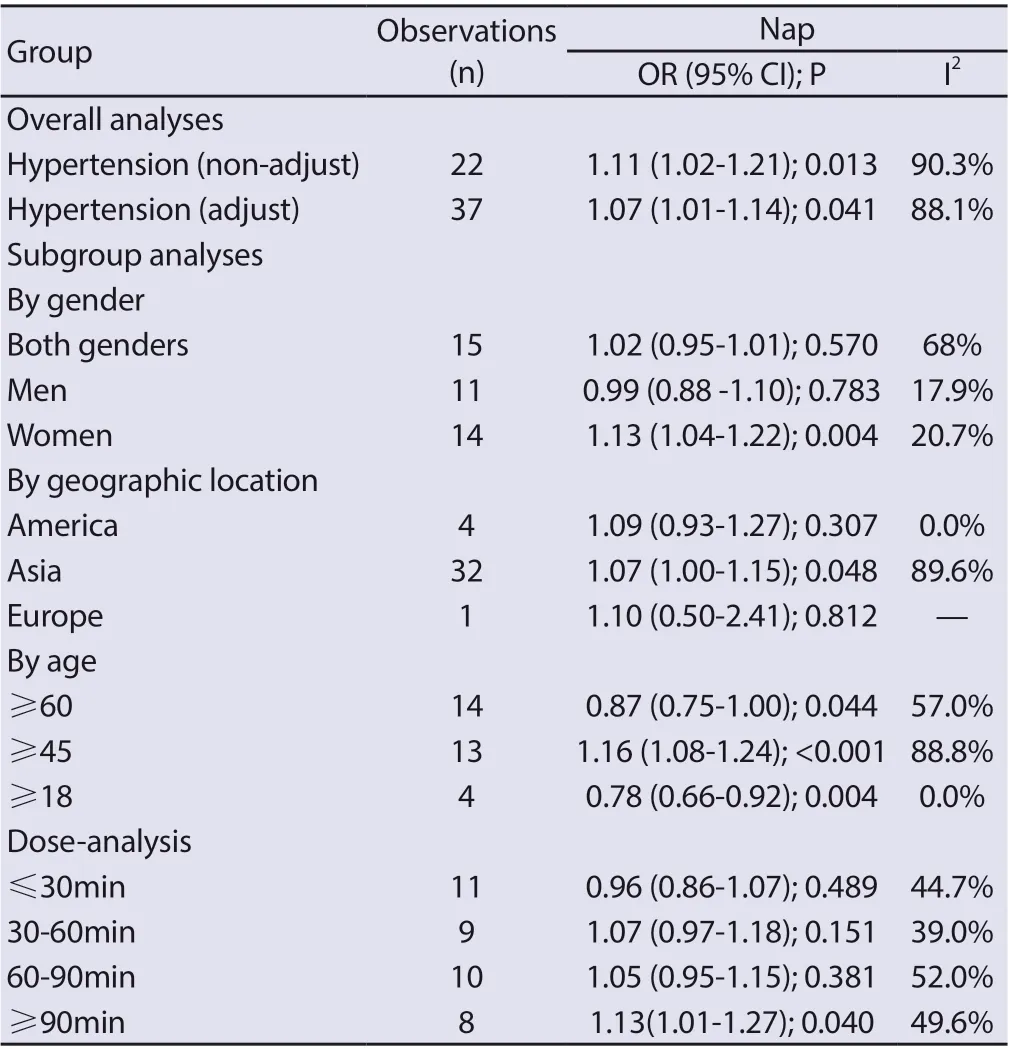
Table3 Overall and subgroup analyses of nap and hypertension.
4. Discussion
To the best of our knowledge, this is the most comprehensive metaanalysis exploring the relationship between siesta and high blood pressure. An important finding of this meta-analysis is that siesta is a risk factor for high blood pressure. This is consistent with the conclusion of a 2016 meta-analysis of siesta and hypertension [16]. However, this study conducted a more detailed subgroup analysis, and concluded that compared with men, the relationship between siesta and hypertension was more significant in women, and the risk of elevated blood pressure and hypertension was higher when napping duration ≥ 90 minutes.
Although the mechanism of the relationship between siesta and hypertension is not completely clear, the more reasonable mechanism is that napping during the day may lead to an increase in cortisol levels at night which may lead to an increase in blood pressure [5, 17]. Some studies have shown that longer sleep increases the risk of high blood pressure. [18], naps increase total sleep time, thereby increasing the risk of high blood pressure. In addition, some studies have shown that siesta is a new risk factor for diabetes[19-22],More than 2/3 of patients with type 2 diabetes reported hypertension[23].Siesta may increase the risk of diabetes and hypertension through the underlying pathophysiological pathway (inflammatory process) of metabolic syndrome[24].However, the link between daytime napping and inflammation is not strong, and some studies have shown that daytime napping after sleep restriction or sleep deprivation contributes to immune recovery rather than night sleep.[25]
In this analysis, by the age subgroup analysis, it is concluded that siesta is the protective factor of hypertension in the elderly people.With regard to this conclusion, there is the view that nap can reflect the severity of some chronic diseases, and that the elderly need more sleep to cope with fatigue, pain, and possible inflammatory processes[3], proper nap duration may could help the elderly to control their blood pressure. More data on the siesta of the elderly are needed for further analysis and exploration in the future. In addition, this conclusion may be the reason for the publication bias of this study. The subgroup analysis in this article shows that the differences in geographical area, age and nap duration may be the reason for the great heterogeneity among the studies. We believes that it is meaningful to longitudinally track adults' siestas.
This meta-analysis has some limitations. First, the cross-sectional study is included in this study, and its causality can not be obtained. Longitudinal analysis is needed to clarify the causal relationship in the future. Second, only a few articles study nighttime sleep duration as a confounding factor, so it is necessary to take nighttime sleep duration into account in the further study of nap. Third, only one article used objective measuring tool to monitor sleep duration, and the other articles used the questionnaires, which is inevitably subjective. Fourth, there is a big difference in age stratification in the included articles, and the rigor of age subgroup analysis will be needed. All in all, the results of this study show that siesta is a risk factor for hypertension, and this association is more obvious in women. More studies are needed to prove that siesta should be used as an important reference factor when screening hypertension clinically.More studies are needed to further demonstrate the relationship between nap and hypertension in the elderly.
 Journal of Hainan Medical College2020年15期
Journal of Hainan Medical College2020年15期
- Journal of Hainan Medical College的其它文章
- Mechanism of Duhuo Jisheng Decoction based on bioinformatics and network pharmacology in treating osteoporosis of kidney Yin deficiency
- Clinical features and prognosis of patients with novel coronavirus pneumonia complicated with diabetes
- A nomogram of 5-year risk of type 2 diabetes in Chinese population
- Yiqi Huoxue Decoction in the treatment of Qi and yin deficiency and stasis type diabetic nephropathy in stage Ⅲ and its effect on VEGF and TGF-β1
- A meta-analysis of the safety of clopidogrel and tegrarol in patients with non-ST elevation acute coronary syndrome after PCI in China
- Super-minimal incision kidney transplantation: Report of 6 cases
