Diagnostic Value of Conventional MRI and DWI for Atypical Primary Central Nervous System Lymphoma(PCNSL)
Corresponding author: Xinyan Yang, Radiologist, Department of Radiology, Sijing Hospital, Songjiang District, Shanghai 201601. E-mail: 731362977@qq.com
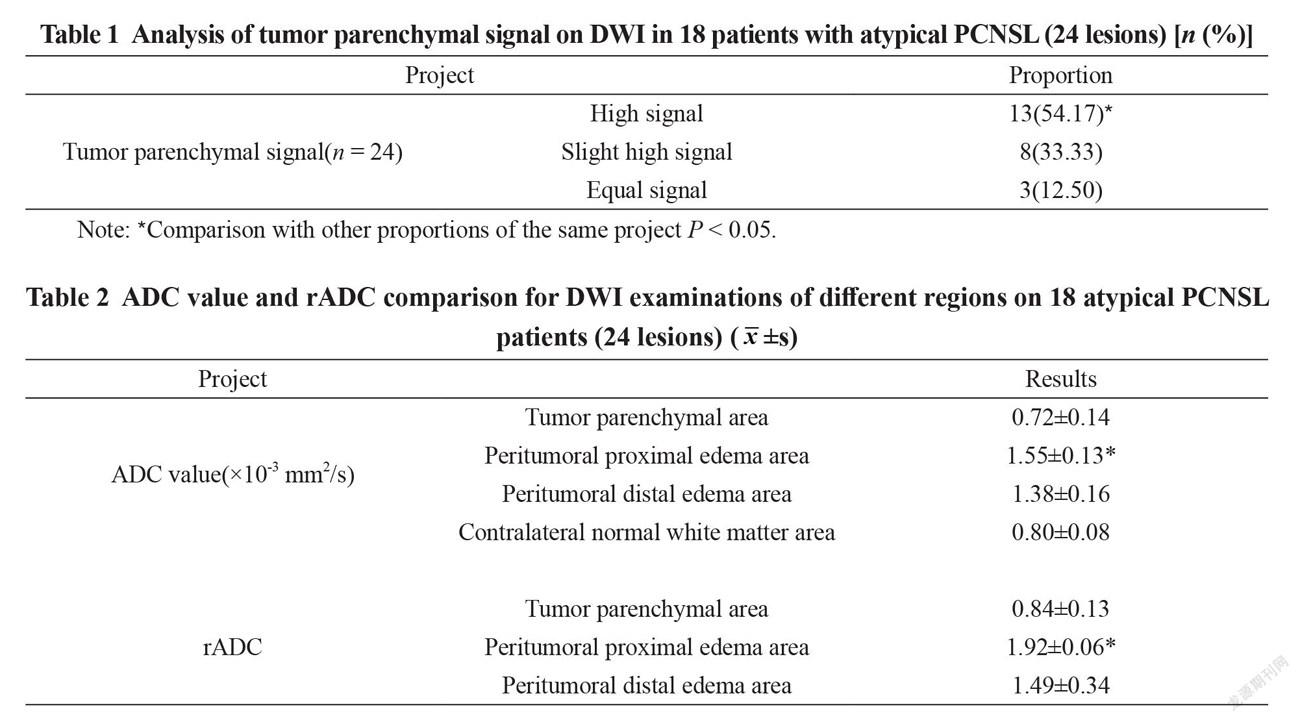
Abstract: Objective: To apply conventional Magnetic Resonance Imaging (MRI) and Diffusion-Weighted Imaging (DWI) to patients with atypical Primary Central Nervous System Lymphoma (PCNSL), and analyze its diagnostic value. Method: We selected 18 patients with atypical PCNSL who had been treated in our hospital from January 2018 to December 2019. All patients underwent conventional MRI and DWI, and we analyzed their MRI and DWI performance. Results: There were 24 lesions among the 18 patients in this group. MRI showed that the lesions were mostly in low signal on T1WI (83.33%), high signal on T2WI (83.33%), some with clear boundaries (62.5%), and some involved the midline structure or ventricles (62.5%). The single lesions were mostly nodular or mass-like enhancements (41.67%), and the multiple lesions were mostly ring-shaped enhancements (29.17%). DWI showed tumor epithelial high signal (54.17%) or slightly high signal (33.33%). The ADC value and rADC of tumor epithelial area, proximal and distal edema area around the tumor were significantly different (P<0.05). Conclusion: Conventional MRI and DWI showed obvious imaging characteristics of atypical PCNSL, with high diagnostic value.
Key words: Central nervous system lymphoma; MRI; DWI
I. INTRODUCTION
Primary central nervous system lymphoma (PCNSL) accounts for about 3% to 5% of intracranial tumors. It is a relatively rare central nervous system tumor. In recent years, the incidence of this disease has shown an increasing trend. Studies have found that PCNSL mainly occurs in people with abnormal immune function, especially people who take immunosuppressants for a long time, and people with acquired immunodeficiency, etc[1]. At present, the clinical treatment of PCNSL is mainly based on chemotherapy, and some patients' lesions can completely disappear after active treatment. In clinical diagnosis, there are certain risks in fine-needle aspiration biopsy, with low diagnosis rate, while preoperative diagnosis is the key to formulating surgical plans and preventing unnecessary craniotomy. MRI is a commonly used imaging technology in the diagnosis of PCNSL, which can display single and multiple deep intracranial lesions. Enhanced scan can show uniform enhancement, and appear "angular sign" and "incision sign". However, some patients' MRI findings are not typical, and are prone to misdiagnosis[2]. DWI can reflect molecular level and make up for the deficiency of conventional MRI diagnosis. The article applies conventional MRI and DWI to patients with atypical PCNSL, and analyzes its diagnostic value. It is reported as follows.
2. MATERIALS AND METHODS
2.1 General information
We selected 18 patients with atypical PCNSL treated in our hospital from January 2018 to December 2019. All patients had been pathologically confirmed; MRI findings were atypical; clinical manifestations include dizziness, headache, nausea, alalia, limb asthenia, blurred vision, and cognitive behavior and mental changes. Among the patients, 8 were males and 10 were females, aged 46 to 70, with an average of (57.57±3.34) years old. There were 16 cases of diffuse large B-cell lymphoma and 2 cases of NK/T lymphocytoma. MRI diagnostic criteria for atypical PCNSL: The imaging findings were not typical. Focal mass like lesions were found in deep periventricular white matter area of cerebral hemisphere (bilateral), with obvious homogeneous enhancement, single or multiple lesions. No hemorrhage, cystic degeneration and necrosis were found, involving ependyma, pia mater and corpus callosum. Preoperative misdiagnosis included meningioma in 4 cases, glioma in 7 cases, encephalitis in 1 case, pituitary tumor in 2 cases, metastasis in 3 cases, and medulloblastoma in 1 case. Patients with history of immune deficiency, organ transplantation and systemic lymphoma were excluded.
2.2 Method
All patients underwent conventional MRI and DWI, using GE Signal 3.0T MR scanner to perform plain scan, enhanced scan and DWI. Parameter settings: SE sequence: T1W1, TE 15 ms, TR 200 ms; T2W1, TE 120 ms, TR 4 300 ms; FLAIR sequence: TE 150 ms, TR 8000 ms; SE-EPI sequence :DWI: TE 100 ms, TR 4 500 ms, b value 0, 1000 s/mm2; interval between layers 1.5 mm, and layer thickness 6 mm. Gd-DTPA was used as contrast agent for the enhanced scanning, with dose 0.1 mmol/kg, and injection flow rate 2 mL/L. Scan parameters: TE 2.5 ms, TR 200 ms, layer spacing 0, layer thickness 1 mm. Axial, sagittal, and coronal enhanced scans were performed after injection. Two experienced radiologists analyzed the images and reached a consensus when they had different opinions. The location and space occupying situation, internal signal characteristics, peritumoral edema and enhancement were observed. The images were uploaded to GE AW4.3 image workstation. 16 lesions with peritumoral edema more than 1 cm were selected. ROI was set in the tumor parenchymal area, peritumoral proximal and distal edema area, with a size of 30-40 mm2. ADC values were measured three times to get the average value. In the same way, an ROI with the same area on the opposite side was selected to measure the ADC value as the reference value, and the relative ADC (rADC) value was calculated.
2.3 Evaluation criteria
Analyze the patient's pathogenic site, MRI, DWI, and pathological manifestations.
2.4 Statistical methods
Spss22.0 was used for data processing. Enumeration data and measurement data were expressed by (%), (X2±s), and X2 or t-test. P <0.05 indicates a difference, which is statistically significant.
3. RESULTS
3.1 lesion analysis
Of the 18 patients in this group, 14 cases (77.78%) with single lesion and 4 cases (22.22%) with multiple lesions. With a total of 24 lesions, including 4 cases of temporal lobe (16.67%), 8 cases of basal ganglia (33.33%), 3 cases of corpus callosum (12.5%), 3 cases of corona radiata (12.5%), and for other parts, like temporal-occipital lobe, occipital, frontal lobe, cerebellar hemisphere, third ventricle, brainstem pons area were 1 (4.17%).
3.2 Analysis of MRI Manifestations
MRI examination showed that the diameter of lesions was 1.2~6.6 cm, with an average of (3.58±1.57) cm. Among the 24 lesions, 20 (83.33%) were low signal on T1WI and 4 (16.67%) were equal signal. T2WI had 20 high signals (83.33%) and 4 equal signals (16.67%). There was 1 hemorrhage (4.17%), 4 cystic and necrotic lesions (22.22%). 15 with clear boundaries (62.5%) and 9 with blurred boundaries (37.5%). 15 (62.5%) of midline structures or ventricles were involved. The extent of tumor space occupation: 15 cases were mild (62.5%), 7 cases were moderate (29.17%), and 2 cases were severe (8.33%). The degree of peritumoral edema: 8 cases were mild (33.33%), 10 cases were moderate (41.67%), and 6 cases were severe (25%). 14 cases showed single lesions: 10 cases were nodular and mass enhancement (41.67%), 2 cases were irregular enhancements (8.33%), 1 case was internal hemorrhages companion ring enhancement (4.17%), and 1 case was bilateral corpus callosum and "butterfly sign" enhancement (4.17%). 10 cases showed multiple lesions: 3 with irregular flaky enhancement (12.5%) and 7 with circular enhancement (29.17%). There were 24 lesions in total: 4 with "gap sign" (22.22%) and 5 with "sharp sign" (20.83%). Among them, 2 lesions (8.33%) showed both "gap sign" and "sharp sign".
3.3 Analysis of DWI Manifestations
Among the 24 lesions, tumor parenchymal high signals occupied the highest ratio (54.17%), and the peritumoral proximal edema area displayed the highest ADC value and rADC, showing significant differences in data comparison (P <0.05), with details in Table 1 and Table 2.
3.4 Pathological analysis
16 cases of diffuse large B-cell lymphoma were diagnosed by surgery and pathology (88.89%). 2 cases of NK/T lymphocytoma(11.11%). The tumor cells presented a "sleeve-like" structure and gathered in the gap around the blood vessel.
4. DISCUSSION
PCNSL is a relatively rare malignant tumor, accounting for only 0.5% to 2.0% of primary brain tumors. Due to the lack of specific symptoms and signs, the patients may have increased intracranial pressure, mental disorders, focal neurological dysfunction and other manifestations[3]. The study found that[4], most PCNSL are non-Hodgkin's lymphoma, and more than 90% are B cell type, T cell type is relatively rare. Because PCNSL progresses rapidly and is highly aggressive, the prognosis is poor. To give patients timely treatment, early diagnosis is very important. DWI is a kind of use of resonance imaging sequence technology to observe the diffusion motion of water molecules, and it has high motion sensitivity. Under normal circumstances, the diffusion methods of water molecules include concentration gradient diffusion, random diffusion, and transmembrane diffusion, which can be affected by many factors and have anisotropic characteristics. Due to the different structures and regional components of brain tissue, the degree of restriction on the diffusion of water molecules is also different. Observing the changes of magnetic resonance signals is helpful to understand the microstructure and functional changes of tumors and brain tissues[5].
Atypical PCNSL is prone to misdiagnosis due to atypical MRI performance, and DWI diagnosis is needed. In this study, there were a total of 24 lesions. MRI examinations were mostly low signal on T1WI (83.33%), high signal on T2WI (83.33%), clear boundaries (62.5%), and midline structures or ventricles (62.5%). The single lesions were mostly nodular or mass enhancement (41.67%), and the multiple lesions were mostly ring-shaped enhancement (29.17%). DWI showed tumor parenchymal high signal (54.17%) or slightly high signal (33.33%). The ADC value and rADC of the tumor parenchyma, proximal and distal edema area around the tumor were significantly different (P <0.05). Comprehensive analysis of conventional MRI , DWI images is helpful for the diagnosis of atypical PCNSL.
Analysis of the image characteristics of atypical PCNSL:
(1) The growth site is atypical, mainly occurring in the deep near midline area of the brain, and it is easy to grow across the midline. Multiple foci can grow on both sides of the cerebral hemisphere at the same time, and can involve the cerebellum and cerebral hemisphere, and some lesions can be diffusely distributed[6].
(2) Multiple lesions are not uncommon, with multiple central infiltrations, which can be located on the same side or on both sides of the cerebral hemispheres, or both superficial and deep lesions. From the perspective of enhancement, the focus is on actual enhancement.
(3) MRI enhancement is atypical. Patients with immunodeficiency and normal immune function during the enhancement scan of typical lesions are mainly ring enhancement and homogeneous enhancement respectively. Because the tumor grows too fast, "umbilical depression", "sharp angle signs", "Fist" and other performances may appear. On the other hand, the atypical PCNSL of the mass type showed "umbilical pit sign" and "butterfly wing sign". The non-mass type lesions showed nodular, streak, patchy, and focal enhancement. Fourth, DWI performance is atypical, because tumor cells have less cytoplasm, less water content, small extracellular space, high nucleocytoplasm ratio, and dense composition, which will limit the diffusion of water molecules, so it shows high signal on DWI and low signal on ADC[7]. With the calculations of ADC value and rADC of different regions, it can be found that there are significant differences.
5. CONCLUSION
To sum up, conventional MRI and DWI examinations show obvious imaging characteristics on atypical PCNSL cases, holding high diagnostic value.
CONFERENCE
[1]Lei Geng, Yi sun, Xiuling Wang, Kai Xu. Conventional MRI and DWI in the diagnosis of atypical primary central nervous system lymphoma[J]. Chinese Journal of Medical Imaging Technology,2018,34(10):1455-1459.
[2]Xiao Wang, Xuefei Deng, Wei Song, Deli Tan, Youzhi Zhu, Xiangwei Luo, Yu Zhang. Value of perfusion weighted imaging in predicting progression free survival of primary central nervous system lymphoma [J]. Journal of Clinical Radiology, 2018,37(03):379-385.
[3]A.S.Cottereau,S.Mulé,C.Lin,K.Belhadj,A.Vignaud,C.CopieBergma, Ruili Du. Whole body diffusion weighted imaging for the detection of iron deposits in Hodgkin’s lymphoma, follicular lymphoma and diffuse large B-cell lymphoma[J]. International Journal of Medical Radiology,2018,41(02):228.
[4]Rui Yang, Xiaorong Chen, Anlu Liu, Peng Min. The value of DWI combined with ADC in the differential diagnosis of primary central nervous system lymphoma and acute cerebral infarction[J]. Modern Medical Journal, 2018,46(01):23-26.
[5]Shengfeng Yu, Xuefei Deng, Dong Hu, Qian Zhang, Xiangwei Luo, Zi Mo, Xuejiang Zhang, Yu Zhang. The predictive value of diffusion-weighted imaging for the efficacy of radiotherapy in primary central nervous system lymphoma[J]. Anhui Medical Journal, 2017,38(06):705-708.
[6]Yu Zhang, Junping Zhou, Wensheng Hao, Donghui Lu, Youzhi Zhu. Diffusion-weighted imaging predicts the chemotherapy efficacy of primary central nervous system lymphoma based on high-dose methotrexate[J]. Journal of Clinical Radiology, 2017,36(05):607-613.
[7]Y.S.Choi,H.J.Lee,S.S.Ahn,J.H.Chang,S.G.Kang,E.H.Kim, Xue Bai. Differentiation of primary central nervous system lymphoma and atypical glioblastoma by area under the curve and diffusion coefficient of dynamic enhanced MRI images[J]. International Journal of Medical Radiology, 2017,40(03):362.
- Trends in Oncology的其它文章
- Analysis of Retropubic and Laparoscopic Radical Prostatectomy for Localized Prostate Cancer
- Diagnostic Value of Electrocardiogram(ECG) in Aortic Dissection Aneurysm
- Analysis of Pain Assessment and Nursing Measures for Patients with Advanced Hematological Tumors
- Virulent Bacteria as ACo-factor of Colon Carcinogenesis: Evidence from Two Monozygotic Patients

