South Asian medicinal plants and chronic kidney disease
Sachinthi Sandaruwani Amarasiri,Anoja Priyadarshani Attanayake,Kamani Ayoma Perera Wijewardana Jayatilaka,Lakmini Kumari Boralugoda Mudduwa
1Department of Medical Laboratory Science,Faculty of Allied Health Sciences,University of Ruhuna,Galle 80000,Sri Lanka; 2Department of Biochemistry,Faculty of Medicine,University of Ruhuna,Galle 80000,Sri Lanka; 3Department of Pathology,Faculty of Medicine,University of Ruhuna,Galle 80000,Sri Lanka.
book=390,ebook=99Abstract
Chronic kidney disease remains as one of the serious health issues in South Asia.The paucity of effective pharmacotherapy targeting the management of chronic kidney disease has led to a search for alternative pharmacologic therapies.The traditional knowledge of medicinal plants plays a key role in the discovery of novel nephroprotective agents.This review aims to present the use of such South Asian ethnomedicinal plants that have sufficient therapeutic potency for the management of kidney diseases.Medicinal plants are rich sources of bioactive compounds that have been reported to exert nephroprotective mechanisms,such as antioxidant,anti-inflammation,diuretic,and immunomodulation.Many South Asian medicinal plants have been detailed in traditional medicinal pharmacopoeias for the management of kidney-related diseases.Some have shown promising effects to address nephropathy in animal models and in vitro research.This information can be beneficial in the development of novel pharmaceutical agents targeting the management of kidney diseases and improvement of quality of life for chronic kidney disease patients by fulfilling the requirements for disease management unmet by modern allopathic medicine.
Keywords: Chronic kidney disease,Medicinal plants,Nephroprotective agents,South Asia,Antioxidant,Antiinflammation
Background
Reports on traditional systems of medicine provide several effective therapeutic approaches to address the diverse pathologic conditions related to kidney disease.In general,medicinal plants are the key element in most of the therapeutic remedies used in traditional systems of medicine.Ethnomedicinal plants used in the management of chronic kidney disease (CKD) are effective in diuresis and renal detoxification,and thus are beneficial to reduce the adverse effects of dialysis treatment [1,2,3,4].The ease of availability,low cost,efficacy,and safety of these plants available as herbal medicines to the general public make their use common in this population [5,6,7,8].Use of ethnomedicinal plants is further supported with the fact that they have shown promising effects in the treatment of diseases that allopathic systems of medicine have failed to manage [5,9].Therefore,these plants are of utmost importance to protect renal function and slow the occurrence and the progression of CKD,thus forestalling the need for end-stage treatment options such as renal replacement therapy [9].
Most of the South Asian population continue to rely on traditional systems of medicine,especially for the treatment of chronic diseases.Several systems of complementary and alternative medicine (CAM) are used in South Asia,with different approaches among the countries in the region,including Ayurveda,Siddha,Unani,and Dhivehi beys,for example.Ayurveda is the oldest system of medicine,originating in 1500-2000 B.C.E.The classical Indian Ayurvedic texts,such as theRigveda(unknown author,written in 1500 B.C.E.-900 B.C.E.),Atharvaveda(unknown author,written in 600 B.C.E.),Charak Samhita(written by Charaka in 120 C.E-162 C.E.),andSushruta Samhita (written by Divodasa Dhanvantari,Susruta and Nagarjuna in 1500 B.C.E.-4thcentury C.E.),likewise may have originated thousands of years ago.In the modern era,in 1997,the National Center for Complementary and Alternative Medicine of the National Institutes of Health in United States (renamed the National Center for Complementary and Integrative Health in 2014) definedCAM as the practices that are not categorized as a part of the current conventional medical system for managing health and disease.The use of ethnomedicinal plants,also referred to as herbal therapeutics,is the most common form of CAM used by CKD patients worldwide.
Although several studies to date have focused on the nephroprotective medicinal plants used in traditional Indian medicine,there is no comprehensive review of the medicinal plants grown in other countries within the South Asia region,to the best knowledge of these authors [2,3].Therefore,this current review focuses on the use of ethnomedicinal plants of South Asian origin,with a potential therapeutic application in kidney disease.
Disease burden in South Asia
CKD remains one of the leading public health issues worldwide [12,13,14].It is characterized mainly by progressive loss of kidney function [15].The complex nature and the risks associated with the progression of the disease to a severe state—called the end-stage renal disease (ESRD)—make the management of CKD quite critical [9].The disease burden is massive in developing countries,as described later in text [12].In addition,CKD is a major contributor to increased morbidity and mortality in South Asia,where the disease is most frequently present as ESRD [16].Thus,CKD has become a devastating health problem in the South Asia,which directly affects the social and economic growth throughout the region [16].
Glomerular nephritis and interstitial disease have been considered to be the most common causes of ESRD in South Asia.Prevalent infections and environmental toxins are identified as the risk factors for glomerular nephritis and interstitial disease,respectively [12,17].However,diabetes mellitus and hypertension have drawn increasing research attention and are currently the leading causes of CKD [12,18].The oxidative stress associated with these two diseases leads to the progression of CKD.A high prevalence of diabetes mellitus and hypertension among the South Asian population may be the reason for an increase in the prevalence of CKD [1,19,20].Furthermore,individuals with a positive family history of kidney disease are more prone to develop diabetic renal disease or glomerulonephritis associated with CKD [14].However,the primary cause of CKD may vary depending on the socioeconomic status of patients and their environmental factors as well [18].
Chronic kidney disease of unknown origin (CKDu) is a condition in which the etiology and the exact prevalence of the disease remain unknown.This type of CKD has become a major health issue throughout South Asia,especially in countries such as Sri Lanka,where most CKDu patients are in the north central and north western provinces of the island,and in the Uva and Eastern provinces as well.Exposure to heavy metals (Cd,As,Pb),fluoride,pesticide residues,glyphosate from herbicides,and cyanogens from algae present in contaminated water sources have been identified as possible predisposing factors for CKDu [17,18,21].
The mean age of CKD patients in South Asian countries is lower compared with those in other countries globally.This age discrepancy may be the result of exposure to environmental toxins at a young age and poor access to health care,which delays diagnosis.In general,South Asian countries perform poorly on health care indices [16,17].Therefore,providing sufficient health care for patient with CKD is a major challenge within this region.Moreover,book=392,ebook=101although the prevalence of CKD is high among South Asian countries,no accurate data are currently available.Most of the reported data are hospital-based records or individual approximations [16].Therefore,there is a large gap between the reported prevalence of CKD and the actual value because many patients with CKD never seek or receive medical attention [17].Furthermore,CKD is often asymptomatic until the disease reaches its advanced stages; thus,these patients already have one or more disease complications or comorbidities by the time they seek medical attention [14].Therefore,it is critical to implement a strategy so that measures can be taken for prevention as well as management of the disease before the progression to ESRD [17].
Management strategies
Management of CKD is mainly based on early diagnosis,pharmacologic intervention,and strategies to preserve renal function [14].Early diagnosis permits initiation of pharmacologic interventions early,resulting in a slower progression from CKD to ESRD.Early diagnosis of the disease may reduce the risks for cardiovascular events as well as the associated comorbidities and mortality [15].
However,pharmacologic management strategies in CKD are constrained by several limitations.First,no medication is available to cure CKD,and the available pharmacologic approaches mainly comprise measures to control the signs and symptoms and reduce the complications of disease [9,22].Second,although the management of hypertension would be beneficial in delaying the decline in renal function for patients with CKD,the therapeutic use of antihypertensive medications,such as angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers,has been undermined because of their serious adverse effects,including neutropenia,proteinuria,angioneurotic edema,and hyperkalemia [14,23,24].
Management of ESRD is possible only with renal replacement therapy [23,25,26].Dialysis and kidney transplantation are two main components of renal replacement therapy; however,their application may be limited because these approaches to management are highly sophisticated and expensive [23].
Although the use of pharmaceutical agents has been beneficial to some extent,the comorbidities and mortality associated with CKD have increased within the past few years.Patients with CKD are more likely to develop other systemic diseases,such as atherosclerosis and cardiovascular disease,which are a frequent cause of mortality [23,25,27].Based on these factors of disease progression and the unavailability of extensive management options and renal replacement therapy facilities,the annual mortality rate for CKD patients is high in South Asian countries compared with other countries globally.Therefore,prevention of disease progression is a critical factor in the appropriate management of CKD [23].
The implementation of measures to preserve renal function is considered as one of the best options available to slow the progression of CKD and to delay the need of renal replacement therapy [28].In this regard,the use of nephroprotective agents at the earlier stages of the disease play an important role in the management of CKD [14].
Complementary and alternative practices in South Asia
The potential threat to quality of life and the chronic nature of kidney disease have led many South Asian patients with CKD to turn to CAM practices to help them manage their disease [29].In addition,the available treatment options in allopathic medicine for CKD are in most cases unaffordable for low- and middle-income patients in South Asia,and this cost factor further directs these patients toward the traditional systems of medicine [30].Furthermore,in terms of the social context of South Asia,the region is known for a rich heritage of traditional systems of medicine that have been practiced for centuries [5].
More than 70% of the South Asian population relies on these nonallopathic systems of medicine that are based on knowledge generated from centuries of experience,observation,and investigation.Traditional systems of medicine served as the mainstay of treatment in most of the South Asian countries before colonization by West [5,6].Traditional medicines comprise a variety of therapeutic approaches,including food habits and the use of herbs,metals,minerals,and precious stones.The approaches may vary among the different countries within the region [6,31,32].
Several CAM systems of have been used in South Asia.For example,Bangladesh,India,Nepal,and Sri Lanka mainly practice Ayurveda,Siddha,and Unani medicine,whereas Maldivians practice their own unique system known as Dhivehi beys [5,6].As the oldest system of medicine,originating in 1500-2000 BC [5,31] Ayurveda is not simply a system of medicine—rather it is the science of life [6,31,32].Its objective is not just treating the diseased person,but also for the person to achieve physical,mental,social,and spiritual well-being [6,31,32].Ayurveda is based on the individualized treatment approaches that promote healing mechanisms and self-repair processes in the body [5].Thus,Ayurveda is effective in the management of common diseases as well as many chronic diseases [6].The Siddha system of medicine has a striking similarity to Ayurveda,but is specialized with regard to iatrochemistry with the use of herbomineral products [6].Moreover,this system uses extensive astrology and incantations during treatments [32].The Unani system of medicine has its origins in Greece.Different modes of treatments including regimental therapy,diet modification,pharmacotherapy,andbook=393,ebook=102surgery are practiced in Unani [5,31].However,medicinal plants play a key role in all of these traditional systems of medicine [6].
Nephroprotective role of natural products
Herbs are the most common forms of CAM used by CKD patients [30,33].The traditional treatment approaches based on medicinal plants focus the cause as well as the outcomes of kidney diseases to forestall the need for hemodialysis and to reduce the adverse consequences of dialysis treatments [1,2,3,4].In addition,herbs are beneficial to relieve some of the associated symptoms of CKD comorbidities,including cutaneous pruritus,fatigue,depression,muscle cramps,and uremic bruising.[29,30,33].These herbs may decrease the frequency of dialysis treatment as well.Therefore,over the past decade there has been a remarkable increase in the use of medicinal plantderived herbal medicines by patients who undergo hemodialysis [33].The diuretic properties of these herbal medicines are not only useful for patients on hemodialysis,but also for pre-dialysis patients by stimulating their declining kidney function and thus delaying the need for dialysis [34].
Since herbal medicines have been used for thousands of years,their use is popular among general public.Moreover,medicinal plants used in the traditional systems of medicine have been beneficial in the discovery of number of modern allopathic medicines.Examples include aspirin,atropine,ephedrine,digoxin,morphine,quinine,reserpine,and tubocurarine,all of which have been developed based on the observations of indigenous medicine [35].It is estimated that nearly one-third of all newly approved compounds in modern pharmacology are derived from medicinal plants [36].Therefore,the World Health Organization has also recommended promoting herbal medicine in order to fulfill the requirements for disease management unmet by modern allopathic medicine [5].The literature supports a number of medicinal plants used in these traditional systems of medicine that show promising effects in renal failure [2,37].
Nephroprotection by suppression of oxidative stress and chronic inflammation
Several mechanisms are suggested for the nephroprotective activity of medicinal plants.Among them the most common mechanism is through the antioxidant defense system [19,37].Antioxidants are the molecules that combat the oxidative stress developed from an imbalance between the rate of production and removal of produced oxidants.Oxidative stress is the causative factor for a wide variety of diseases,including CKD [19].A key advantage to medicinal plants is that they are rich sources of antioxidants,mainly present in the form of phenolic compounds (flavonoids,phenolic acids,tocopherols,tocotrienols),ascorbic acid,and carotenoids.These substances work to prevent renal damage by reducing lipid peroxidation and increasing endogenous antioxidants [9,19,38,39].Therefore,supplementation with medicinal plant-derived antioxidants is of utmost importance in curtailing the free radical pathologies present in CKD [14].However,the literature provides evidence for the capacity of natural whole products rather than single antioxidants or their combinations in preventing or managing kidney diseases [19].
Another important mechanism of nephroprotection is the anti-inflammatory effects of medicinal plants.The compounds such as curcumin and resveratrol found in medicinal plants have shown promising effects in nephroprotection by modulating inflammation processes [30].Moreover,other pharmacologic characteristics,such as diuresis,immunomodulation,reduction in proteinuria,and stimulation of renal repair mechanisms,may contribute to slowing the progression from kidney-related disease conditions to later-stage disease [1,36].
Polyphenols in medicinal plants play an important role in nephroprotection by acting as antioxidant,antiinflammatory,and diuretic agents [1,36].The enormous value of these phytoconstituents mandates investigating the bioactivities of medicinal plants for the discovery of nephroprotective therapeutic agents.In this context,medicinal plants used in the management of kidney-related diseases in traditional systems of medicine have drawn increasingly more research attention.
Although a large number of medicinal plants are used in the therapy for kidney diseases in the indigenous and traditional systems of medicine,most have not been scientifically scrutinized for their therapeutic effects as well as for their safety.Therefore,it is important to validate the use of these plants through phytochemical analysis and investigation of their relevant pharmacologic activities [35].In view of that goal,many research studies have been conducted in the fields of pharmacognosy,chemistry,pharmacology,and clinical therapeutics,on native medicinal plants through the approach of reverse pharmacology,facilitated by traditional knowledge [1,3,31,40,41,42,43,44].Table1 summarizes an overview of such ethnomedicinal plants of South Asian origin,with potential for the treatment of kidney diseases.
Nephroprotective activity of medicinal plant extracts on animal models
A number of medicinal plants with nephroprotective activity have been effective in the treatment of kidney diseases as shown in animal models [36,41,72,69,88].These plants have been useful in the management of glomerulonephritis,different forms of nephropathies,glomerulosclerosis,nephrotic syndrome,lupus,and tubulointerstitial nephritis,as well as in the treatment of kidney stones [36].
Different mechanisms of nephrotoxicity are used forthe scientific investigation of nephroprotective activity of the medicinal plants in animal models.Several different nephrotoxic agents,including therapeutic drugs,diagnostic agents,and chemicals,have been used to induce nephrotoxicity in animal models.The most common among them is the use of various antineoplastic agents including the following:cisplatin,cyclophosphamide,streptozotocin,carmustine,lomustine,semustine,mitomycin,mithramycin,and doxorubicin.Moreover,aminoglycosides,such as gentamycin,amikacin,kanamycin,and streptomycin,and antimicrobial agents,such as tetracycline,acyclovir,pentamidine,sulfadiazine,trimethoprim,and rifampicin are widely used as nephrotoxic agents.Furthermore,the literature supports the use of heavy metals such as Hg,As,Pb,and Bi as nephrotoxic agents [113,114].
book=394,ebook=103
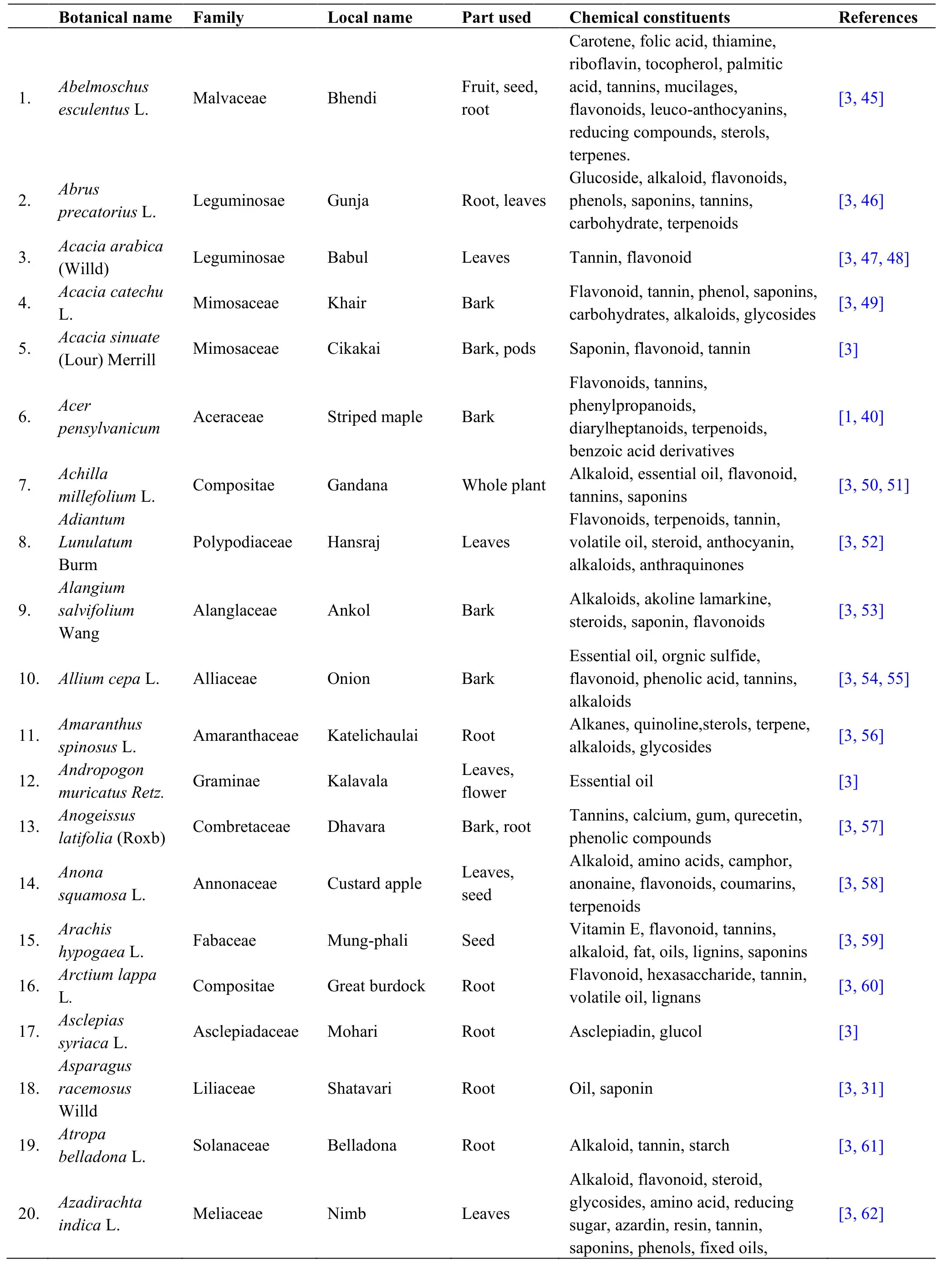
Table1 Overview of South Asian medicinal plants used in therapy for kidney diseases
book=395,ebook=104
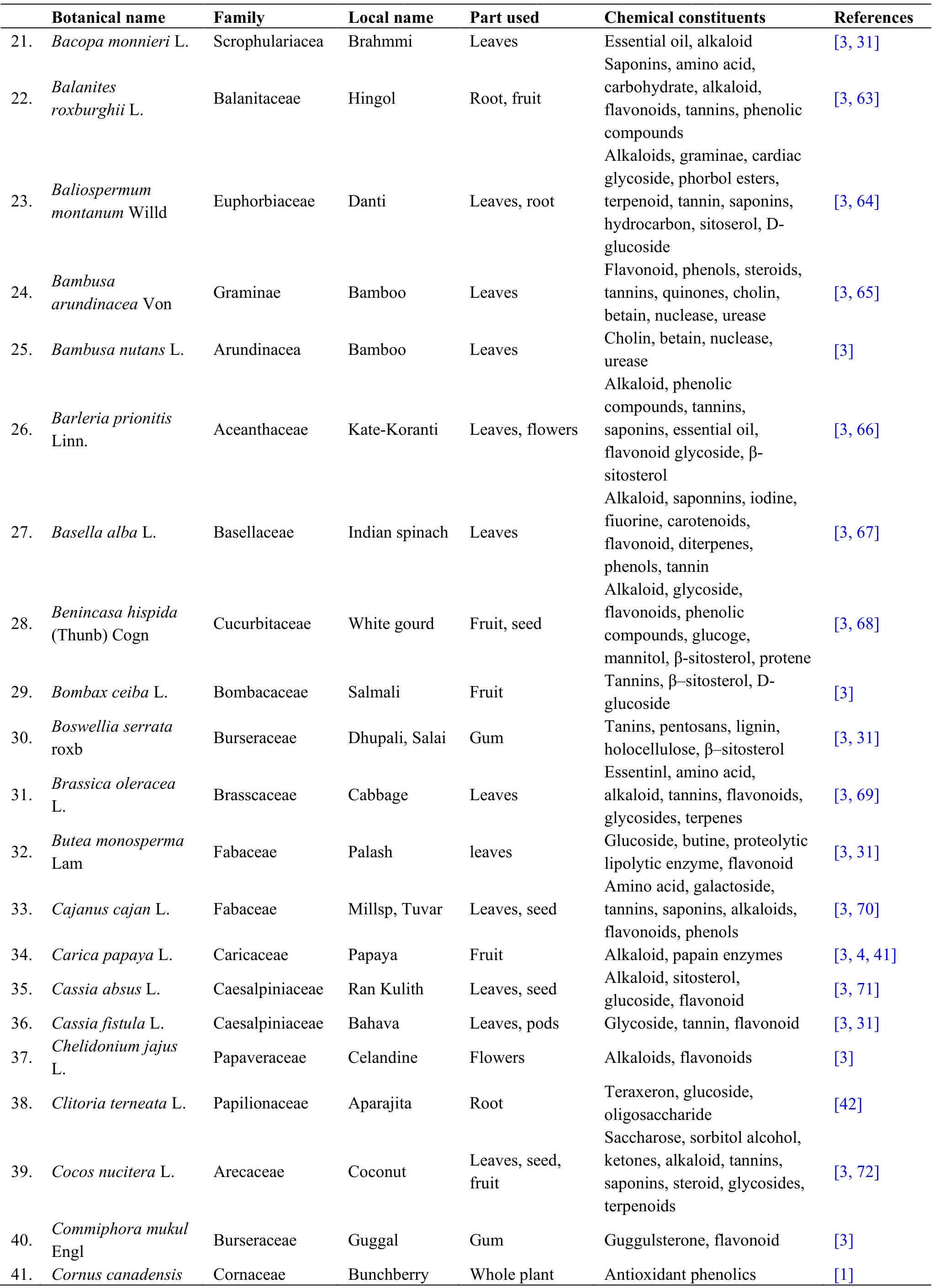
Table1 Overview of South Asian medicinal plants used in therapy for kidney diseases (continued)
book=396,ebook=105
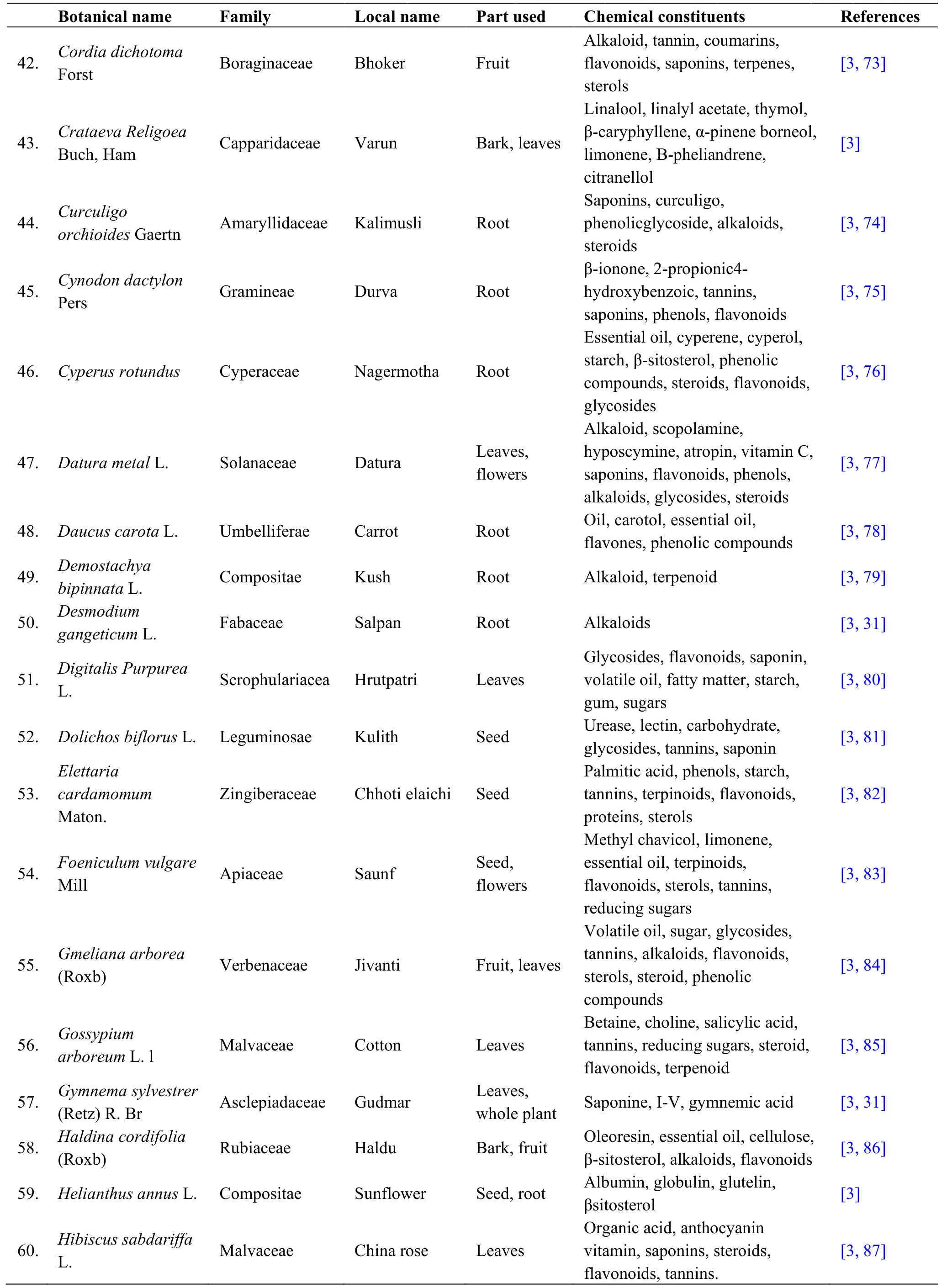
Table1 Overview of South Asian medicinal plants used in therapy for kidney diseases (continued)
book=397,ebook=106
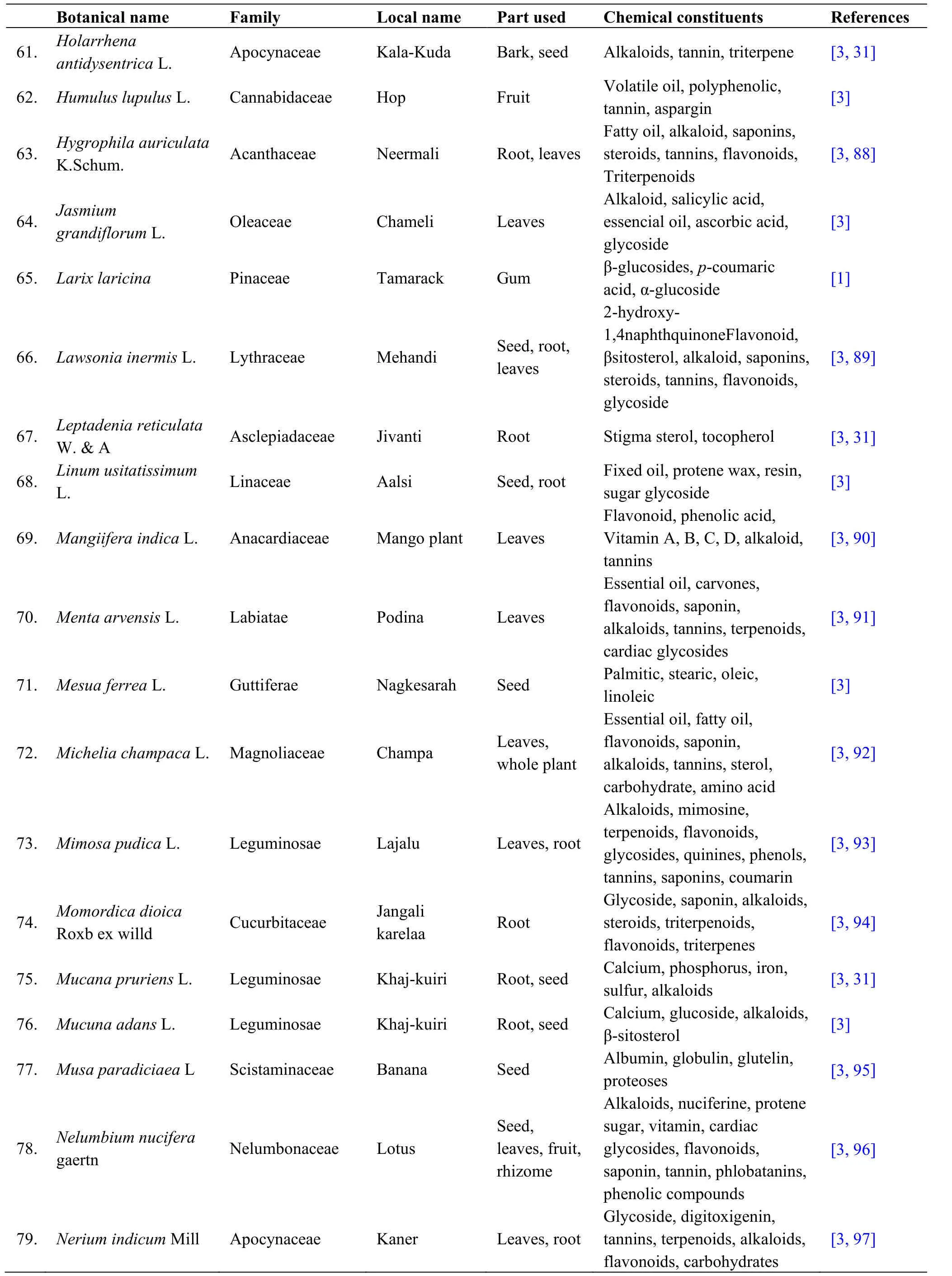
Table1 Overview of South Asian medicinal plants used in therapy for kidney diseases (continued)
book=398,ebook=107
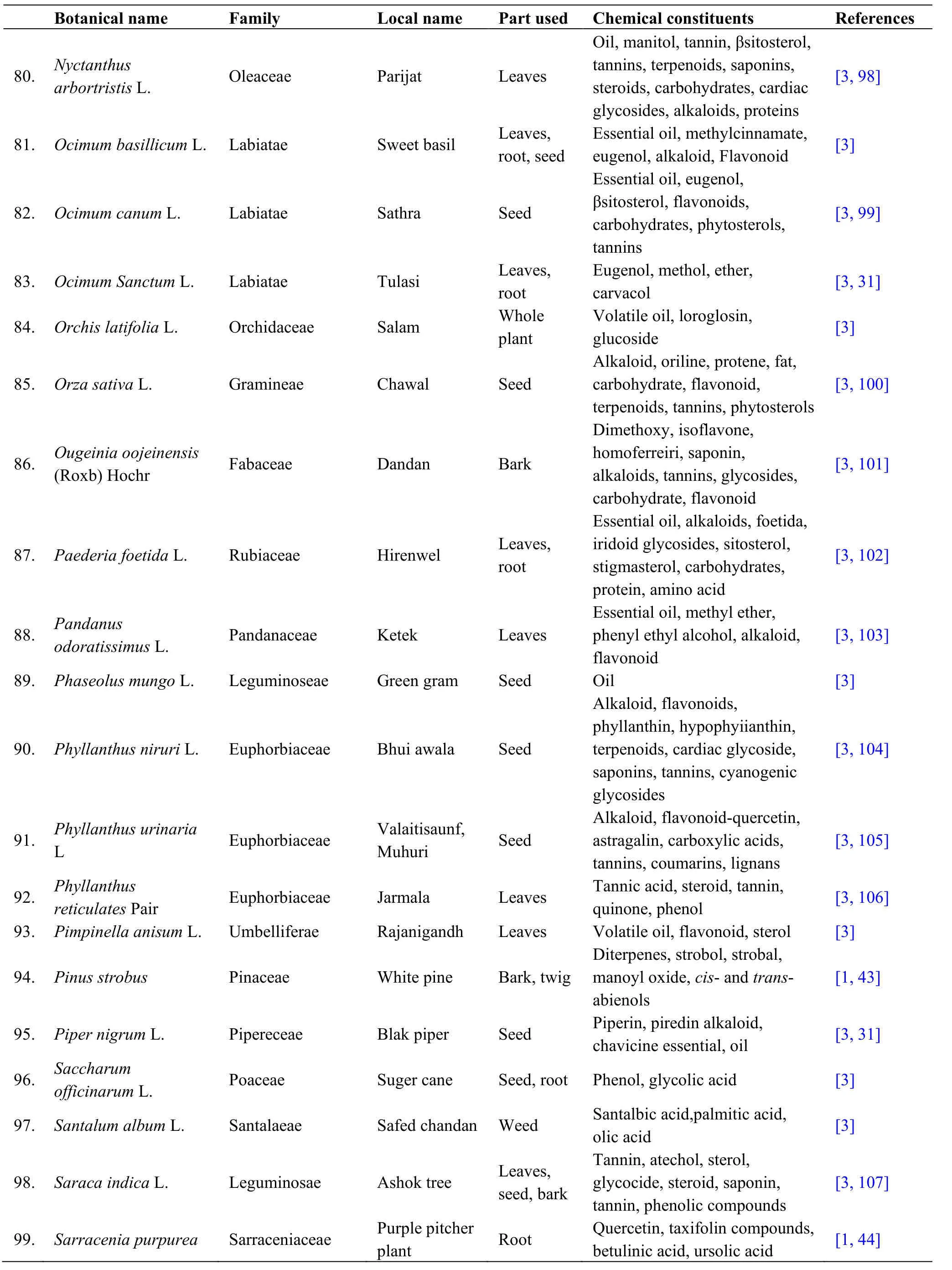
Table1 Overview of South Asian medicinal plants used in therapy for kidney diseases (continued)
book=399,ebook=108
These toxins may directly affect the membrane permeability of renal tubular cells,thereby causing potential injury.Further,they involve in remodeling of the cellular surface changing the area available for ion transportation.These changes may result in accumulation of intracellular calcium and loss of enzymes and nucleotides.An increase in calcium in the renal cortex and mitochondria may lead to features of cellular necrosis and renal failure [114].Further,intracellular metabolism of these toxic drugs lead to the formation of reactive metabolites,such as free radicals,which are toxic for cells.The superoxide ions formed during oxidation of hydroxyl radicals in turn leads to lipid peroxidation.This effect may result in oxidative deterioration of polyunsaturated lipids of membranes,causing modification of the structure and function.Moreover,these nephrotoxins may reduce the concentration of antioxidants,superoxide dismutase,glutathione,catalase,vitamin E,and ascorbic acid,all of which are protective against free radical injury.In addition,these toxins might induce changes in the integrity of renal tubular cells,thereby causing several lethal changes such as development of abnormallybook=400,ebook=109enlarged lysosomes and myeloid bodies,loss of brush border membrane,and vacuolization and dilation of the endoplasmic reticulum.Free radical-induced renal damage has been demonstrated in several in vivo and in vitrostudies that have shown the development of glomerular dysfunction and proteinuria because of altered glomerular permselectivity by chemical infusion of reactive oxygen species [114].
Table2 details the nephroprotective medicinal plants for which the protective activity was investigated in animal models.The nephroprotective activity was evaluated using changes in renal function parameters as follows:serum creatinine,blood urea,serum protein,serum albumin,urine creatinine,urinary protein,albumin,uric acid,and urinary osmolality [113,118,121,124,129,143].Furthermore,plasma concentrations of malondialdehyde,superoxide dismutase,reduced glutathione,and total antioxidants were investigated in several studies [120,121,125,131,132,136,139].Assessment of histopathology in hematoxylin and eosin-stained kidney sections for the features of glomerular congestion,tubular casts,peritubular congestion,epithelial desquamation,blood vessel congestion,and presence of inflammatory cells have also been conducted for the evaluation of the nephroprotective effects of these medicinal plants in selected animal models [114,115,116].
In addition to these medicinal plants,the nephroprotective activity of a polyherbal mixture composed ofBauhinia racemosa(Caesalpiniaceae; stem bark),Dolichos biflorus(Fabaceae; seed),Sphaeranthus indicus(Asteraceae; flower),Tectona grandis(Verbenaceae; saag seed),Tephrosia purpurea(Fabaceae; leaves) andTribulusterrestris(Zygophyllaceae; fruit) have been investigated for nephroprotective effect by Chopda et al.[8].Gentamicin was administered to induce renal toxicity.Coadministration of the polyherbal mixture at three selected doses resulted in reverting changes in biochemical parameters.The protective effect was found increased with the increased dose of the mixture.Assessment of histopathology revealed the features of tubular necrosis,increased urinary space,loss of epithelial lining,and inconspicuous nucleoli in the nephrotoxic control group.However,the highest dose of the polyherbal mixture resulted in restoration of the changes induced by gentamicin in the animal model.Further,the polyherbal preparation has shown relativelybook=405,ebook=114high antioxidant activity in the kidney tissues [8].
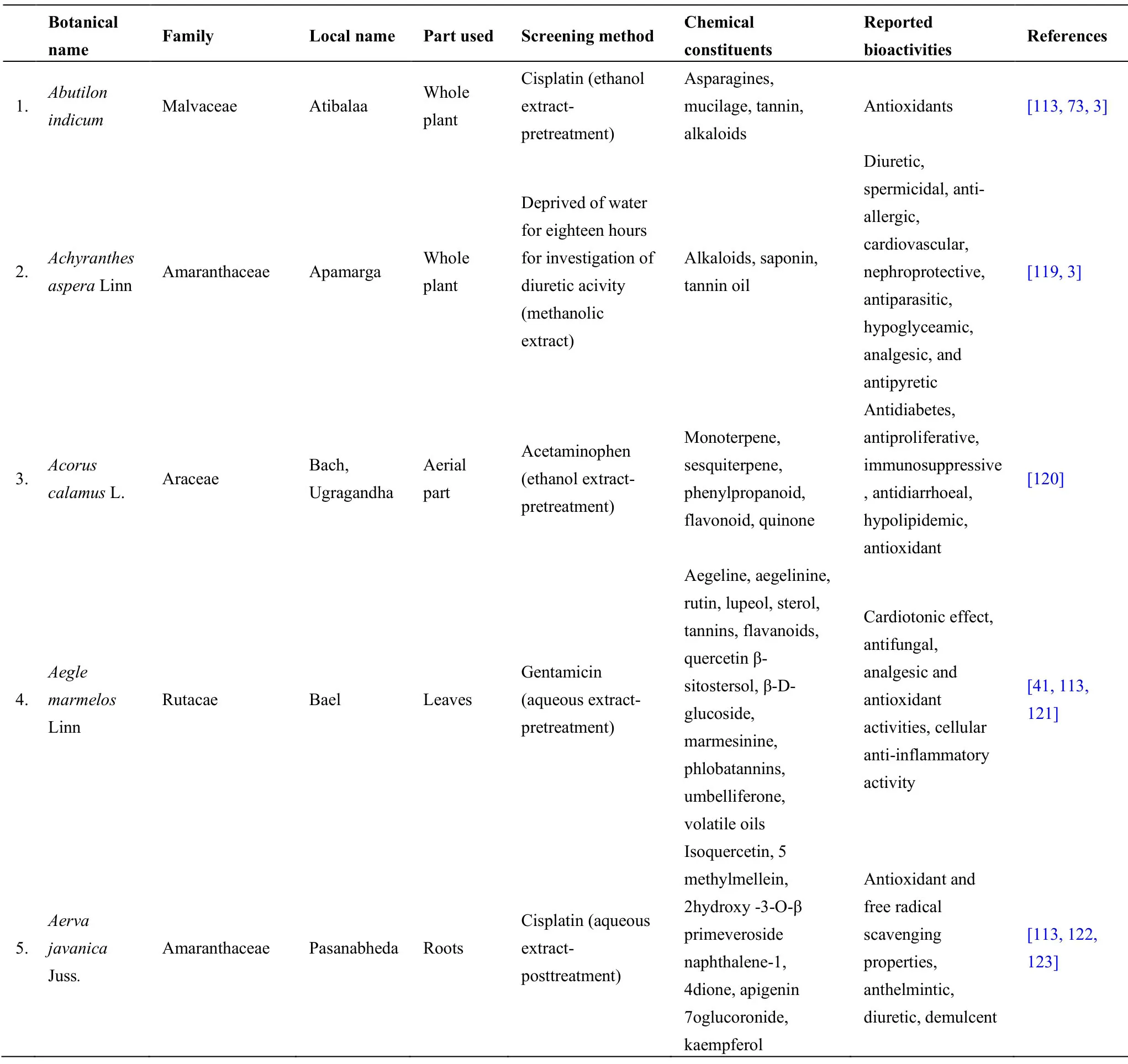
Table2 South Asian medicinal plants investigated for nephroprotective activity in animal models
book=401,ebook=110
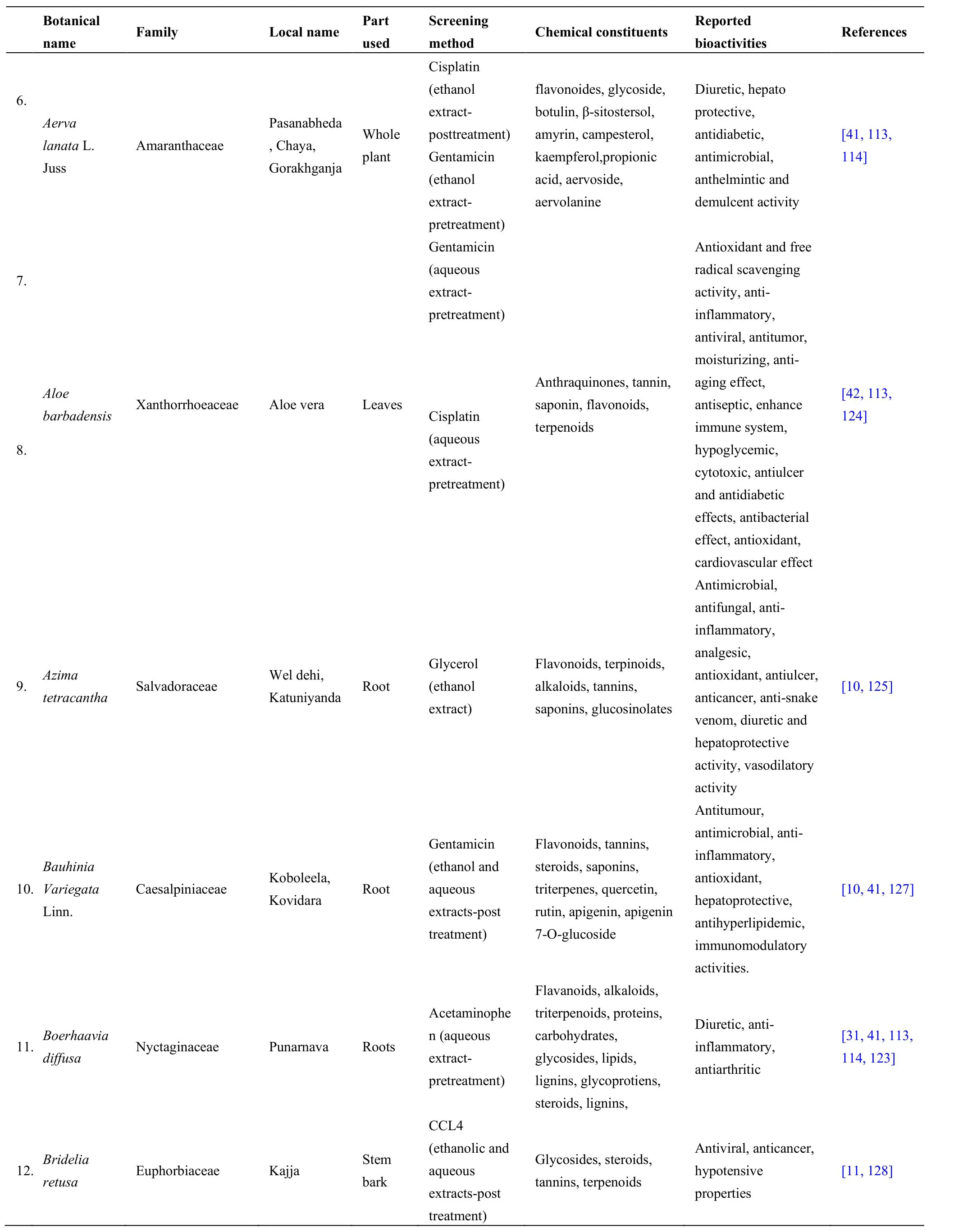
Table2 South Asian medicinal plants investigated for nephroprotective activity in animal models (continued)
book=402,ebook=111
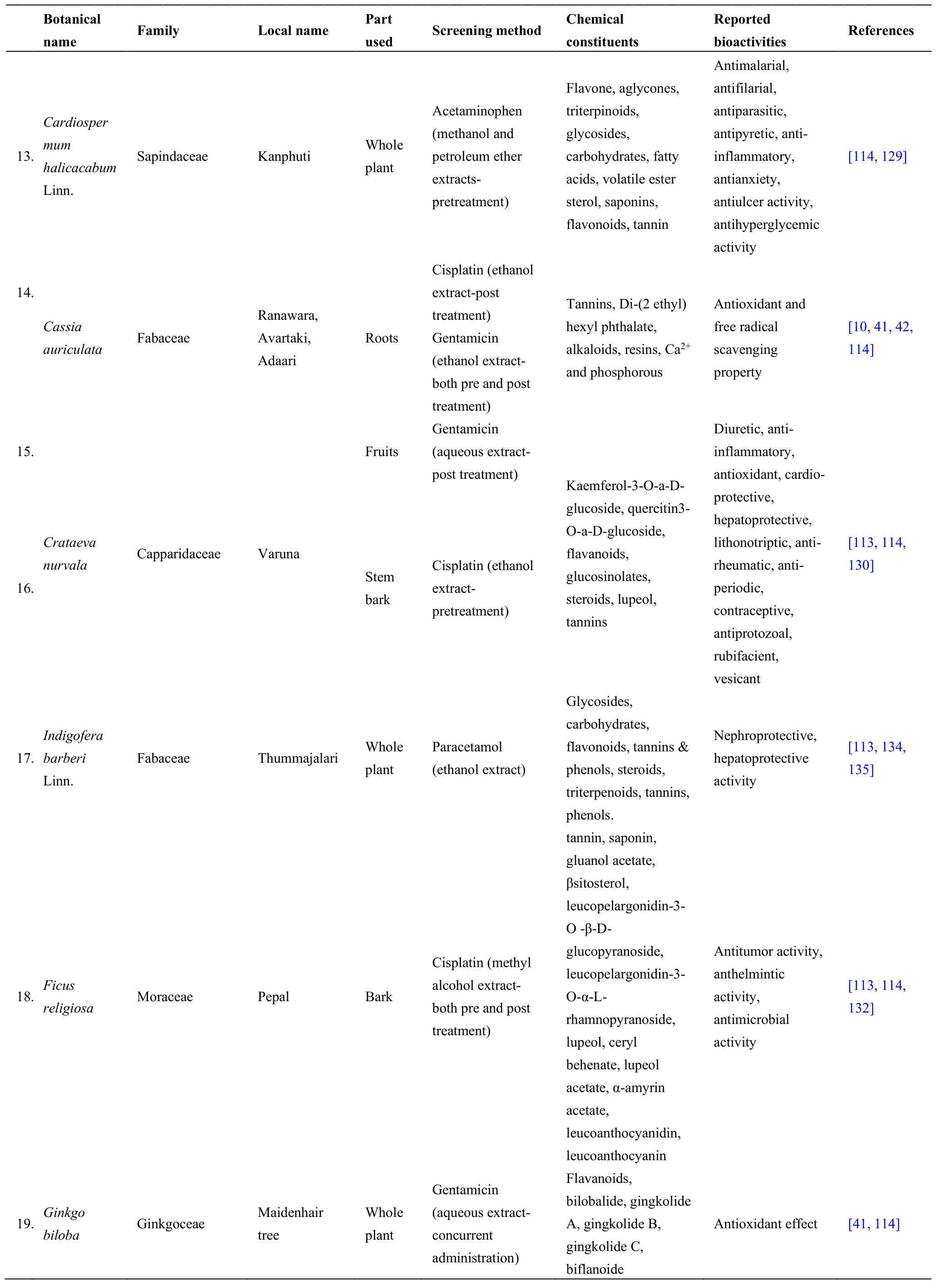
Table2 South Asian medicinal plants investigated for nephroprotective activity in animal models (continued)
book=403,ebook=112
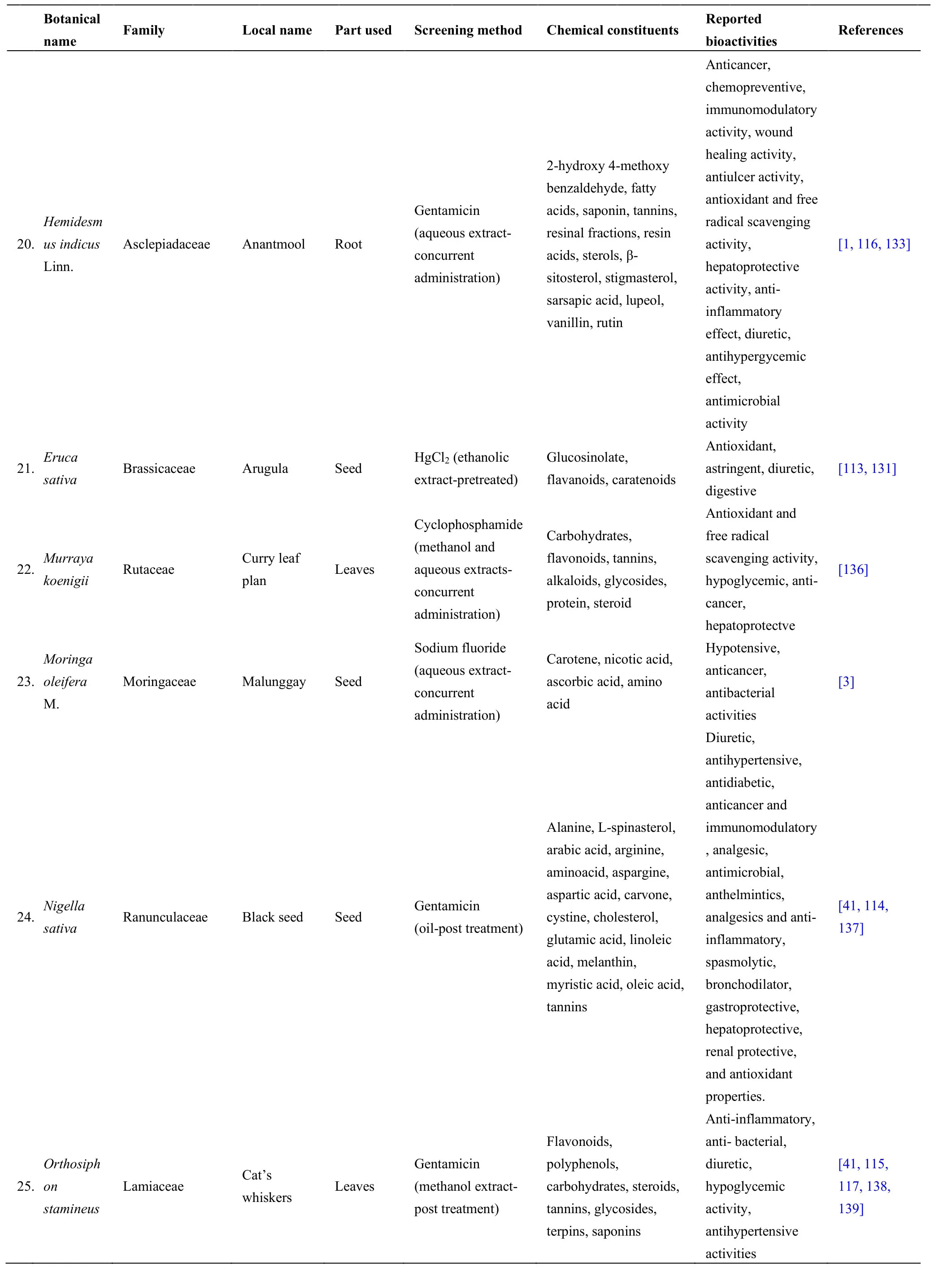
Table2 South Asian medicinal plants investigated for nephroprotective activity in animal models (continued)
book=404,ebook=113
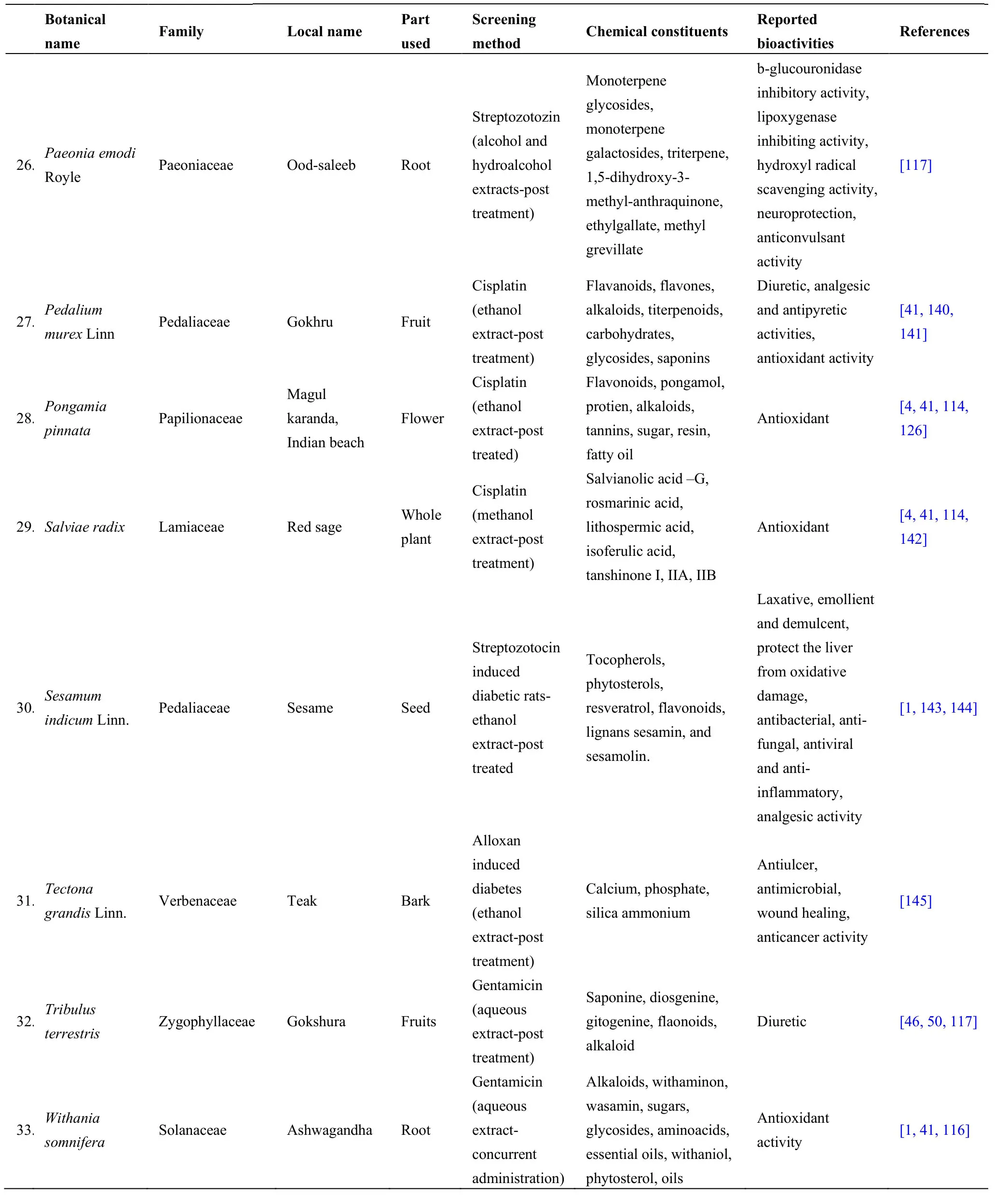
Table2 South Asian medicinal plants investigated for nephroprotective activity in animal models (continued)
Moreover,the protective role of the aged garlic extract (AGE),which works as an antioxidant,has been investigated on gentamicin induced nephrotoxicity in male Wistar rats.Pretreatment with the AGE at a dose of 1.2 mL/kg every 12 hours ameliorated the changes in biochemical parameters and histopathology induced by gentamicin,suggesting the use of AGE for the prevention of gentamicin induced nephrotoxicity [114].
Similar studies have been used for evaluation of the nephroprotective effect of compounds isolated from medicinal plants,and increasingly more attention has been given to the use of phytochemicals as a protective strategy against nephrotoxicity [146].A major turning point was the demonstration of nephroprotective potential for phenolic compounds,including flavonoids [146].Table3 depicts such phytoconstituents/ compounds isolated from South Asian medicinal plants with proven nephroprotective effects against nephrotoxicity tested in animal models.
In vitro assessment of nephroprotective activity
Based on the ethical concerns and the “3R” principle:reduction,replacement,and refinement,more attentionhas been recently directed toward in vitro cell-based studies for the discovery of new therapeutic candidates.Accordingly,a number of studies have been conducted on the therapeutic efficacy of medicinal plants in kidney diseases using different cell lines such as human renal proximal tubule cells HK-2,pig kidney epithelial cells LLC-PK1,and human embryonic kidney cells HEK293,in different nephrotoxicity models [154].The nephroprotective effect was assessed by the measurement of cell viability through 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) bioassay in most of the studies [146].Scoparia dulcisLinn.(Scrophulariaceae) is one such South Asian medicinal plant for which nephroprotective activity was determined by MTT assay in HEK 293 against gentamycin-induced nephrotoxicity [155].However,sparse evidence is available for the in vitro assessment of nephroprotective medicinal plants of South Asian origin.
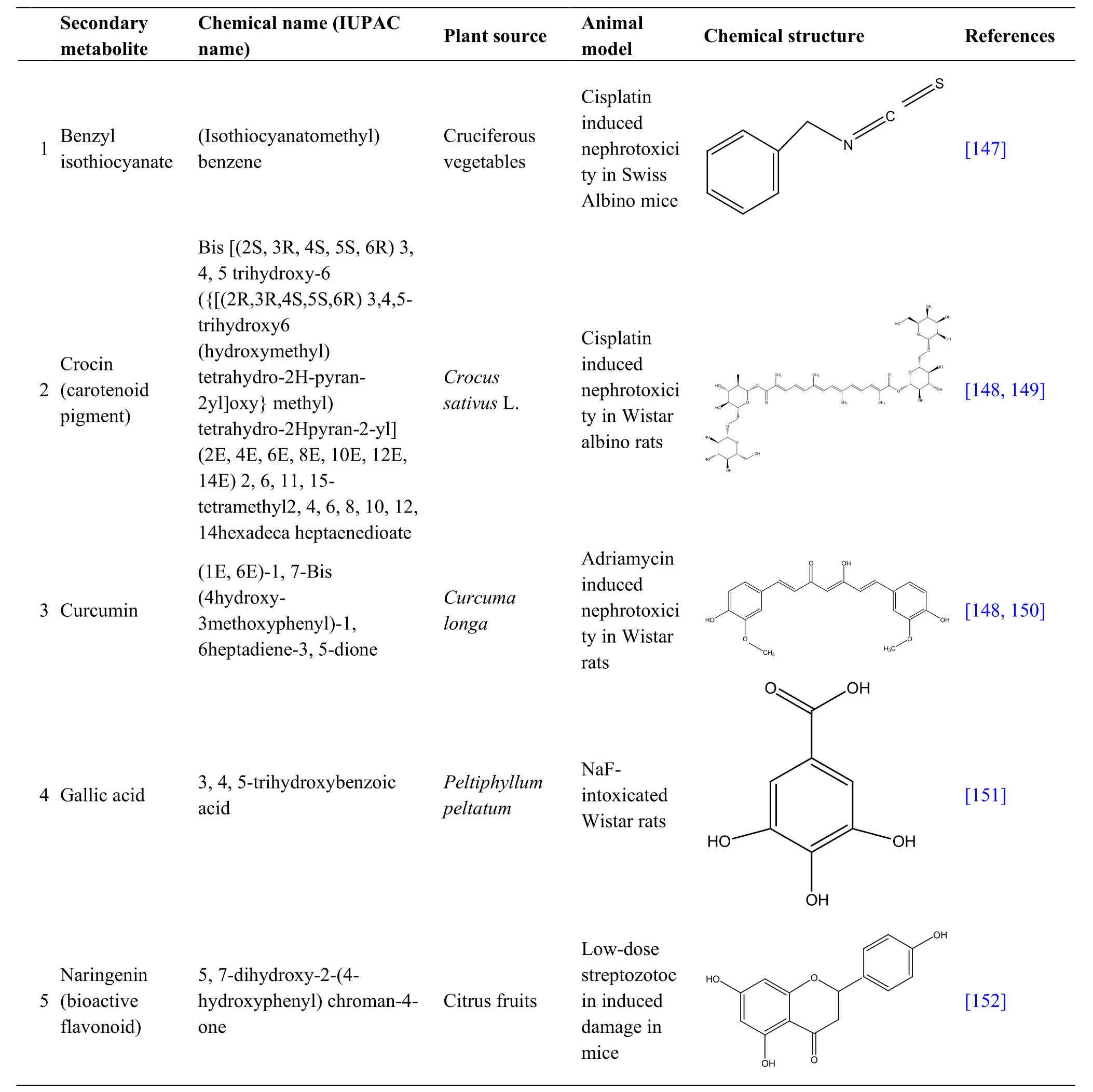
Table3 Nephroprotective secondary metabolites from South Asian medicinal plants against nephrotoxicity in animal models
book=406,ebook=115
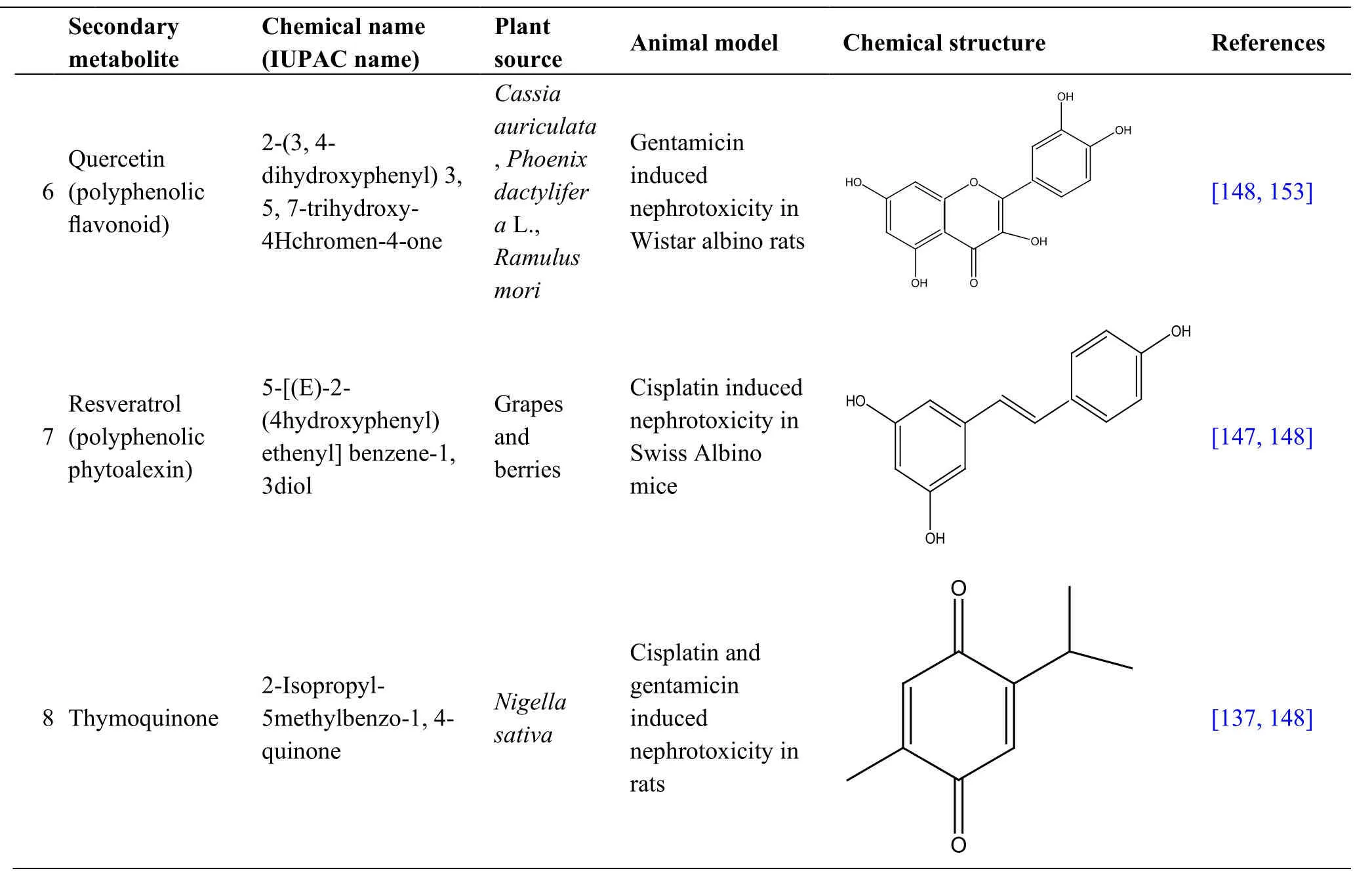
Table3 Nephroprotective secondary metabolites from South Asian medicinal plants against nephrotoxicity in animal models (continued)
Conclusion
Medicinal plants used in traditional systems of medicine have become valuable sources of knowledge for modern medicine.This plant-based knowledge serves as a powerful search engine as well as a facilitator for the discovery of novel drugs.Accordingly,a large number of research studies are being conducted on medicinal plants native to the South Asian region,in combination with modern technology for the discovery of nephroprotective agents.The discoveries will be beneficial in the near future in the clinical arsenal of medicine,especially for patients with limited access to use expensive Western systems of medicine.Further,these findings will be advantageous for developing nutraceuticals with high nephroprotective effects in the management of CKD.
 Traditional Medicine Research2020年5期
Traditional Medicine Research2020年5期
- Traditional Medicine Research的其它文章
- Inner peace makes you live longer
- East to west:research progress in traditional Chinese medicine for antiaging strategies
- The effects of nutritional ketosis induced by Bigu-herbs regimen and ketogenic diet on diseases and aging
- From religious manual to herbal pharmacopoeia:a textual study of the formation and transformation of Shennong’s Classic of Materia Medica
- Molecular mechanism prediction analysis of compound Kushen injection in the treatment of COVID-19 based on network pharmacology and molecular docking
- Ethnoveterinary medicines used against various livestock disorders in the flora of Shamozai Valley,Swat,KP Pakistan
