Clinical observation on muscle regions of meridians needling method in improving upper limb function for children with cerebral palsy of spastic hemiplegia type
Li Nuo (李诺), Jin Bing-xu (金炳旭), Zhao Yong (赵勇), Fu Wen-jie (符文杰), Liu Zhen-huan (刘振寰), Liang Bi-qi (梁碧琪), Pang Bi-hui (庞碧徽)
Nanhai Maternity and Children’s Hospital Affiliated to Guangzhou University of Chinese Medicine, Foshan 528200, China
Abstract
Keywords: Acupuncture Therapy; Musculature of 12 Meridians; Rehabilitation; Cerebral Palsy; Hemiplegia; Myospasm; Movement Disorders; Child, Preschool
Cerebral palsy (CP) is a syndrome characterized by persistent movement, abnormal posture and limited activity due to non-progressive brain injury in the developing fetal or infant. There are 20-35 CP children per 10 000 live births[1]. Spastic hemiplegic CP accounts for approximately 44% of the total number of CP patients[2]. Among patients with spastic hemiplegia, unilateral upper limb dysfunction is more obvious than lower limb dysfunction. Because of the younger age of onset and poor self-control, children often use the healthy side of upper limb habitually. It is easy to form ‘learned non-use’ or ‘developmental disuse’ on the affected side[3].
The muscle regions of meridians needling method has good efficacy in treating limb spasm in adults after stroke[4-6]. Considering the clinical characteristics of Jingjin (muscle regions of meridians) diseases, spastic hemiplegic CP can be attributed to Jingjin (muscle regions of meridians) diseases[7-8]. Therefore, since 2012, we applied muscle regions of meridians needling method in treating children with spastic hemiplegic CP, and observed the improving effect of muscle regions of meridians needling method on upper limb function in children with spastic hemiplegic CP.
1 Clinical Materials
1.1 Diagnostic criteria
This study referred to the diagnostic criteria of CP in theChina Guidelines for Rehabilitation of Children with Cerebral Palsy(2015, part 1)[1]: non-progressive brain injury; dyskinesia caused by lesion site in the brain; symptoms occur in infancy; can be combined with intellectual disorder, epilepsy, psychosensory disturbance, communication disorder and abnormal behavior; exclusion of central dyskinesia caused by progressive diseases and temporary motor retardation in normal children; the clinical symptom type was spastic hemiplegia.
1.2 Inclusion criteria
Those who met the above diagnostic criteria of CP of spastic hemiplegia type; aged 12-48 months; children and their guardians agreed to participate in this trial and signed informed consent.
1.3 Exclusion criteria
Those who might reduce the enrolling possibility or complicate the enrollment; patients with progressive or retrogressive diseases or malignant tumors; with chronic diseases of heart, liver or kidney, or infectious diseases; with coagulation disorder or skin lesions and unable to have acupuncture treatment; children with hemiplegia due to acquired factors (such as craniocerebral trauma) 6 months after birth.
1.4 Dropout criteria
Those who interrupted treatment for more than 7 d during the trial; who had severe adverse events that caused treatment interruption; or with incomplete data that affected efficacy or safety evaluation.
1.5 Statistical methods
All data were statistically analyzed by the SPSS version 21.0 statistical software. Counting data were expressed by frequency, and analyzed by Chi-square test. Measurement data in normal distribution and having homogeneous variance were expressed as mean ± standard deviation (±s). The independent samplet-test was used for comparisons between the groups, and repeated measures analysis of variance was used for intra-group comparisons.P<0.05 was considered to indicate a statistically significant difference.
1.6 General data
A total of 100 children with CP of spastic hemiplegia type were enrolled from the Pediatric Neurore- habilitation Department of Nanhai Maternity and Children’s Hospital Affiliated to Guangzhou University of Chinese Medicine, between January 2017 and December 2018. All the children were divided into a treatment group and a control group according to the visiting sequence, with 50 cases in each group. There were no dropout cases during the treatment. The children in the treatment group were aged between 16 and 42 months. The children in the control group were aged between 17 and 45 months. There were no significant differences in the data of gender, age, duration and examination in electroencephalography between the two groups (allP>0.05), indicating that the two groups were comparable (Table 1).

Table 1. Comparison of general data between the two groups
2 Treatment Methods
Children in both groups were treated with the same conventional rehabilitation.
Physical therapy: Based on Bobath manipulation and Rood technique.
Tuina manipulations: Tui-pushing, Rou-kneading and An-pressing manipulations were applied to local part, and Dian-digital An-pressing was applied to points.
Occupational therapy: The fine movement training of the affected hand, such as pinching the object with the opposite fingers, wrist dorsal extending and pinching beans.
The above treatments were individualized by rehabilitation therapists according to the clinical manifestations, and the daily training lasted for 3 h.
2.1 Control group
In addition to the conventional rehabilitation, children in the control group received conventional acupuncture.
Points: Jianyu (LI 15), Quchi (LI 11), Shousanli (LI 10) and Hegu (LI 4) on the affected side.
Method: The above points were punctured by using Hwato brand disposable filiform needles of 0.30 mm in diameter and 25 mm in length after routine disinfection. The physician punctured Hegu (LI 4) with the tip of needle towards Erjian (LI 2). And the remaining points were routinely acupunctured. After the arrival of qi, the twirling reducing manipulation was performed, and the needles were retained for 15 min.
2.2 Treatment group
In addition to conventional rehabilitation, the children in the treatment group were given muscle regions of meridians needling method.
Acupuncture site of the shoulder: The nodal points of muscle regions of the Large Intestine Meridian and Triple Energizer Meridian on the shoulder were punctured. The nodal point of muscle regions of meridians below deltoid [located at the termination of the deltoid muscle, with upper limb dropping naturally, on the line between Quchi (LI 11) and Jianyu (LI 15), 7 cun above Quchi (LI 11), which was the nodal point of muscle regions of meridians in shoulder abduction], nodal points of muscle regions of meridians on deltoid [located above the deltoid muscle, about 1.5 cun from the left and right sides of Jianyu (LI 15), between the anterior, middle and posterior bundles of deltoid muscles, which were the nodal points of muscle regions of meridians in shoulder flexion and medial rotation, extension and lateral rotation], (Figure 1).

Figure 1. Acupuncture at the shoulder
Acupuncture site of the elbow: The nodal points of muscle regions of meridians on the pronator teres [located at the elbow, on the line between the medial end of the transverse line of the elbow and the medial epicondyle of humerus, similar to the location of Shaohai (HT 3)], (Figure 2).

Figure 2. Acupuncture at the elbow
Acupuncture site on the back of the hand: Between the five metacarpophalangeal joints and the proximal interphalangeal joints on the affected side of the back of the hand (Figure 3).
Acupuncture site of the palm: Between the five metacarpophalangeal joints and the proximal interphalangeal joints on the affected side of the palm (Figure 4).
Figure 3. Acupuncture at the back of the hand

Figure 4. Acupuncture at the palm
Methods: After routine disinfection, the filiform needles of 0.30 mm in diameter and 25 mm in length were inserted rapidly into the muscle regions of meridians nodal points of the shoulder and elbow, till the tip of needles reached the periosteum. Then lifting- thrusting and twirling manipulations were performed strongly, and penetrating acupuncture was performed forward and backward along the tendon route. After the arrival of qi at the points on the hand, the lifting-thrusting and twirling manipulations were performed strongly, with the intensive needling sensation, but not causing sustained finger dorsiflexion. Acupuncture on the shoulder, elbow and hand was performed simultaneously, and the needles were retained for 15 min.
Acupuncture was performed once every other day in both groups, for 30 times in total.
3 Observation on Results
3.1 Observation items
The trial was evaluated by a designated therapist or physician in a quiet, detached, and well-lit room. The room temperature is controlled at 20-30 ℃. The below items were assessed before treatment, 3 and 6 months after treatment, respectively.
3.1.1 Surface electromyography (sEMG)
The FlexComp Infiniti System (provided by Nanjing Vishee Medical Technology Co., Ltd., manufactured by Thought Technology Ltd., Canada) was used for sEMG testing. The test was conducted in the sEMG room at room temperature of 25-28 ℃. The EMG signals of triceps brachii at resting state and during active elbow extension, and signals of pronator teres during passive supination of forearm were collected. The tests were repeated 3 times, and the root mean square (RMS) of the three tests was used for analysis[9].
3.1.2 Peabody developmental motor scale-fine motor (PDMS-FM)
The PDMS-FM score was used to evaluate the fine motor ability of hands[10]. The scale was used to assess the fine motor function of children aged 0-6 years old, mainly to evaluate the grasping ability and the visual-motor integration ability. There were 26 items in the grasping part and 72 items in the visual motor integration part. The evaluation results were expressed by standard score and development quotient. The standard scores included grasping ability and visual-motor integration ability. A higher score indicated a better fine motor development.
3.1.3 Fine motor function measure (FMFM)
The scale was mainly used to measure visual tracking, upper limb joint activity, grasping and operating ability, and hand-eye coordination ability of children with CP. The scale had a total of 61 items, using 0, 1, 2 and 3 four-level grading method, and the original score was 183 points. By looking up the table, the FMFM score with equidistant characteristics could be obtained, and the score range was 0 to 100 points. Some items in FMFM could be completed with only one upper limb, while the paired evaluation data of the affected side and healthy side should be collected at the same time[11].
3.2 Results
3.2.1 Comparisons of the RMS values of triceps brachii and pronator teres
Active elbow extension reflected triceps brachii muscle strength and passive supination reflected pronator teres muscle tension.
In the test of active elbow extension, the RMS values of triceps brachii muscle in both groups 3 and 6 months after treatment were increased compared with those before treatment, and the intra-group differences were statistically significant (allP<0.05). Compared with the same group 3 months after treatment, the RMS values in the control group were increased 6 months after treatment, but the intra-group differences were statistically insignificant (P>0.05). Six months after treatment, the RMS values in the treatment group were higher than those 3 months after treatment, and the intra-group differences were statistically significant (P<0.05). The values in the treatment group were higher than those in the control group 6 months after treatment, and the differences between the groups were statistically significant (P<0.05).
In the passive supination test, the RMS values of triceps brachii muscle in the treatment group 3 and 6 months after treatment were lower than those before treatment, and the intra-group differences were statistically significant (allP<0.05). The RMS values 6 months after treatment in the control group were decreased compared with those before treatment, and the intra-group differences were statistically significant (P<0.05). Six months after treatment, the RMS values in the treatment group were lower than those in the control group, and the differences between the groups were statistically significant (P<0.05), (Table 2).
3.2.2 Comparison of the PDMS-FM score
Three and six months after treatment, the PDMS-FM scores in the treatment group were increased compared with those before treatment, and the intra-group differences were statistically significant (bothP<0.05). And the scores were all higher than those in the control group at the same time points, and the differences between the groups were statistically significant (bothP<0.05). Three months after treatment, the PDMS-FM score in the control group was increased compared with that before treatment; and 6 months after treatment, the score was increased compared with that 3 months after treatment, but all the intra-group differences were statistically insignificant (bothP>0.05); while 6 months after treatment, the score was higher than that before treatment, the intra- group difference was significant (P<0.05), (Table 3). time points, and the differences between the groups were statistically significant (bothP<0.05). Six months after treatment, the score in the control group was increased compared with that before treatment, and the intra-group difference was statistically significant (P<0.05), (Table 4).
3.2.3 Comparison of the FMFM score
Three and six months after treatment, the scores in the treatment group were increased compared with that before treatment, and the intra-group differences were statistically significant (bothP<0.05). The scores were higher than those in the control group at the same
Table 2. Comparison of the RMS values of triceps brachii and pronator teres between the two groups before and after treatment (±s)
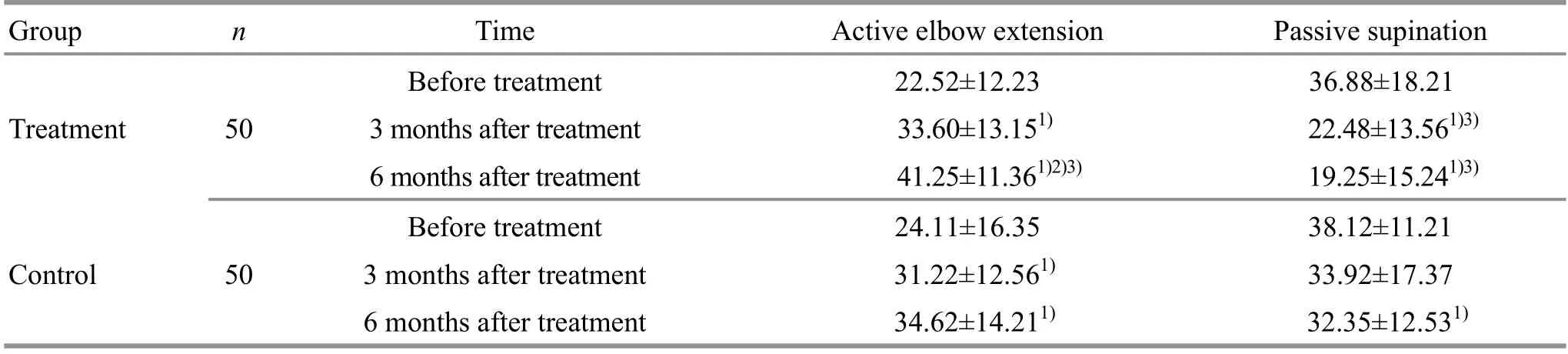
Table 2. Comparison of the RMS values of triceps brachii and pronator teres between the two groups before and after treatment (±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the same group 3 months after treatment, 2) P<0.05; compared with the control group at the same time point, 3) P<0.05
Group n Time Active elbow extension Passive supination Before treatment 22.52±12.23 36.88±18.21 Treatment 50 3 months after treatment 33.60±13.151) 22.48±13.561)3) 6 months after treatment 41.25±11.361)2)3) 19.25±15.241)3) Before treatment 24.11±16.35 38.12±11.21 Control 50 3 months after treatment 31.22±12.561) 33.92±17.37 6 months after treatment 34.62±14.211) 32.35±12.531)
Table 3. Comparison of the PDMS-FM score between the two groups before and after treatment (±s, point)
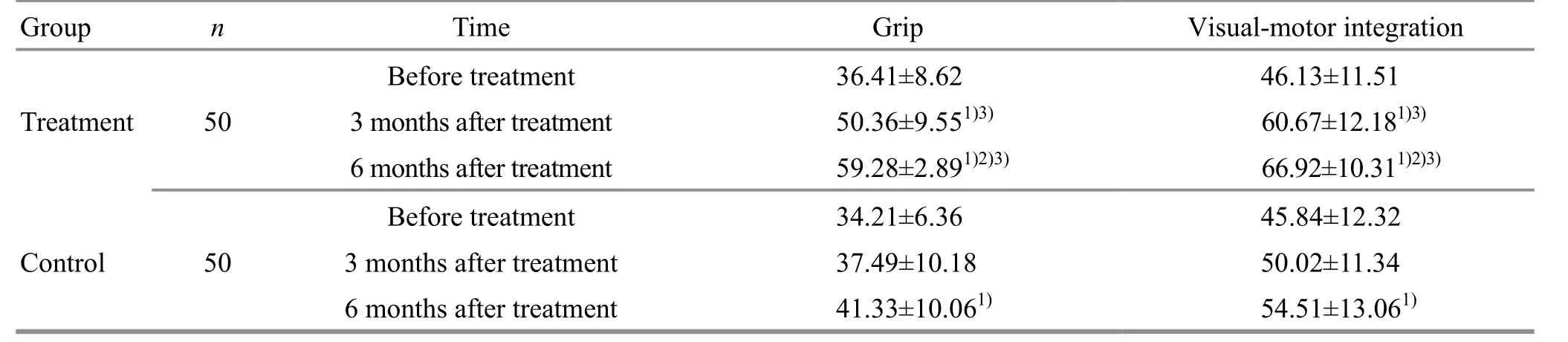
Table 3. Comparison of the PDMS-FM score between the two groups before and after treatment (±s, point)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the same group 3 months after treatment, 2) P<0.05; compared with the control group at the same time point, 3) P<0.05
Group n Time Grip Visual-motor integration 46.13±11.51 60.67±12.181)3) 66.92±10.311)2)3) 45.84±12.32 50.02±11.34 54.51±13.061)
Table 4. Comparison of FMFM score between the two groups before and after treatment (±s, point)
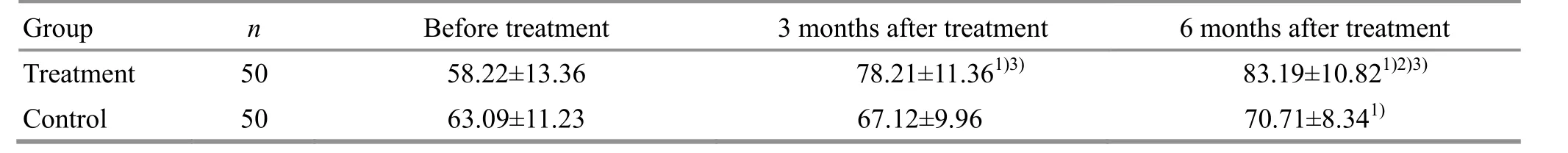
Table 4. Comparison of FMFM score between the two groups before and after treatment (±s, point)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the same group 3 months after treatment, 2) P<0.05; compared with the control group at the same time point, 3) P<0.05
6 months after treatment 83.19±10.821)2)3) 70.71±8.341)
4 Discussion
The theory of Jingjin (muscle regions of meridians) originated fromLing Shu(Spiritual Pivot), where it discusses the Jingjin (muscle regions of meridians) in details, and points out that there is a close relationship between the muscle regions of 12 meridians and the treatment of diseases[12]. The muscle regions of 12 meridians mainly gather around joints and skeletons, with main functions of connecting skeletons, communicating the whole body and governing the joint activities. Wei ZG,et al[13]consider that the complete Jingjin (muscle regions of meridians) system should include the muscle regions of 12 meridians and muscle regions of Zang-fu organs inLing Shu(Spiritual Pivot), that is, the Jingjin (muscle regions of meridians) in macroscopic and microcosmic view. Ru K,et al[14]believe that Jingjin (muscle regions of meridians) should be formed by linear tissues with tension proprioceptive, such as muscle spindles, tendons and ligaments and joint capsules, which functionally connect and interlock. It is a system that integrates form, function and information perception. It forms up during the generation and development of the human body, and it is a motion ontology perception system that connects and interacts with the body and the brain-spinal cord nervous system.
The diseases of Jingjin (muscle regions of meridians) are mainly manifested in movements[15], such as local or general muscle twitching and rigidity, which all belong to the category of Jingjin (muscle regions of meridians) disease, and are particularly common in children with spastic hemiplegia. Therefore, according to the TCM and modern medicine theory, the limb dysfunction of cerebral palsy falls under the category of Jingjin (muscle regions of meridians) disease. ‘Muscle regions of meridians needling method’ was founded by academician Shi Xue-min. It absorbs the essence of Jingjin (muscle regions of meridians) theory in TCM and combines with long-term clinical practice and modern medicine[16]. At present, it is widely used in the treatment of nervous system diseases and motor system diseases[17-19].
Modern research showed that strong stimulation to Jingjin (muscle regions of meridians) could effectively stimulate the proprioceptive sensory nerves, and the nerve impulses caused by it were transmitted into the brain through afferent nerve fibers to promote brain tissue reconstruction, and then spread out through α motor neurons in the anterior angle of the spinal cord, thus inhibiting limb spasticity[20]. In addition, there are multiple sets of small muscle groups in the hand, and their coordinated movements play an important role for the fine movements such as thumb index finger pinching objects. Acupuncture at the root of the finger can induce excitement of paralyzed muscle spindles, thereby generating afferent impulses and maximizing the upload to the different levels in the brain through the sensory afferent pathway in the spinal cord, stimulating the function recovery of damaged brain tissues or promoting brain function reorganization, so as to achieve the regulation of the lower nervous center, and ultimately promote the recovery of fine movements of the paralyzed hand[21]. The above description may be the mechanism of muscle regions of meridians needling method in the treatment of paralysis.
In this study, the selected points on the shoulder, elbow and hand are all located around the joint[22], which could smooth and benefit the joint, and relieve the spasm of the upper limb. The study results showed that compared with the same group before treatment, the RMS values of triceps brachii and pronator teres of the children in both groups increased after treatment, and so did the grasping score and visual-motor integrated score of PDMS-FM, and the FMFM score (allP<0.05). With the prolongation of treatment course, the increase degree was further improved, and the increase range in the treatment group was significantly higher than that in the control group (P<0.05), indicating that adding muscle regions of meridians needling method to conventional rehabilitation was more beneficial for the recovery of upper limb function than adding conventional acupuncture in children with spastic hemiplegic CP, which could improve the independent living capacity and quality of life in the children. It was worthy of clinical promotion and further research.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by 2013 Medical Scientific Research Project of Foshan Science and Technology Bureau (2013 年佛山市科技局“医学类科研攻关项目”, No. 201308202).
Statement of Informed Consent
Informed consent was obtained from the guardians of the recruited children in this study.
Received: 30 October 2019/Accepted: 11 December 2019
 Journal of Acupuncture and Tuina Science2020年4期
Journal of Acupuncture and Tuina Science2020年4期
- Journal of Acupuncture and Tuina Science的其它文章
- Clinical observation of Zhen’ai needling method in Nei Jing (Classic of Internal Medicine) for children with allergic rhinitis accompanied by adenoid hypertrophy
- Clinical observation of tuina manipulations for tic disorders in kids
- Electronic moxibustion apparatus and traditional moxibustion in treating knee osteoarthritis: a randomized controlled trial
- Clinical observation on filiform fire-needling plus continuous passive motion therapy for frozen shoulder
- Clinical study on auricular point sticking plus Western medicine for moderate gastric cancer pain
- Therapeutic efficacy of moxibustion plus medicine in the treatment of infertility due to polycystic ovary syndrome and its effect on serum immune inflammatory factors
