骨科住院患者医院感染特点与危险因素分析
康中琴 吴晓英
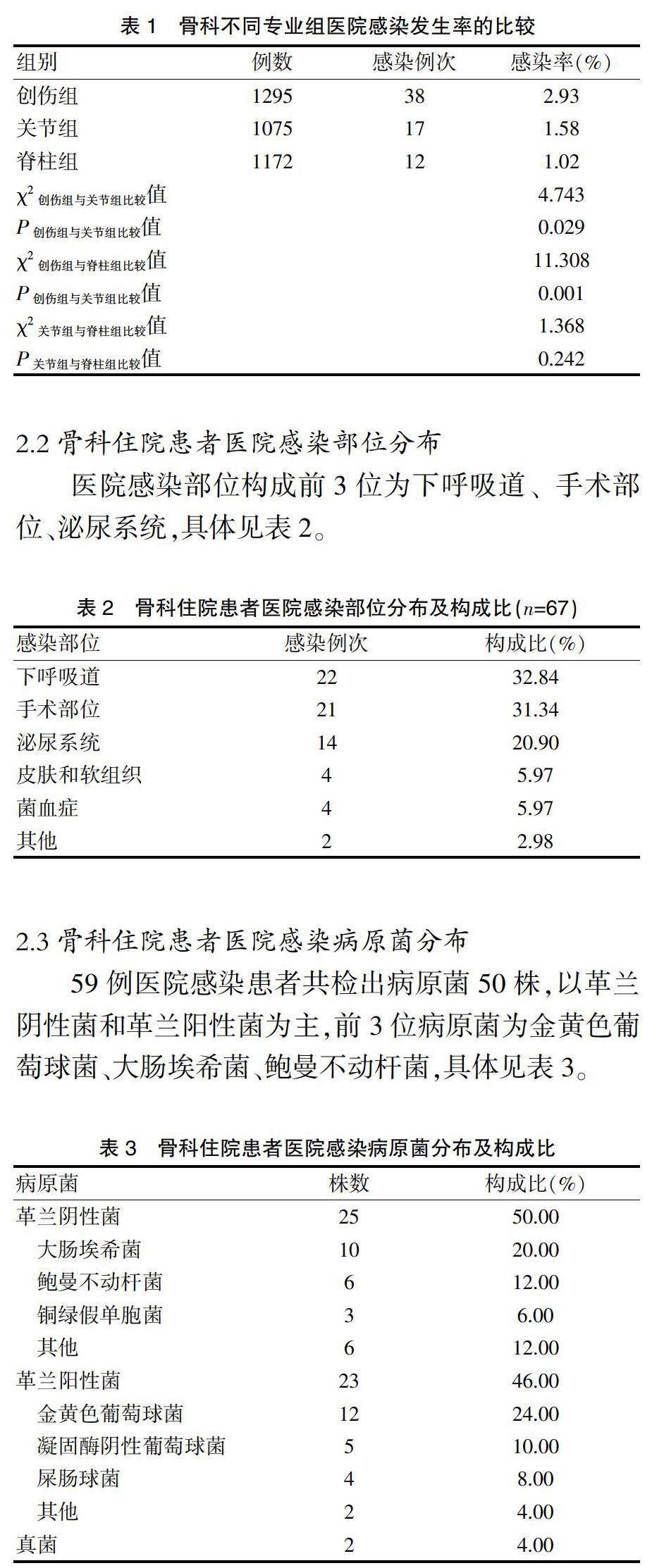
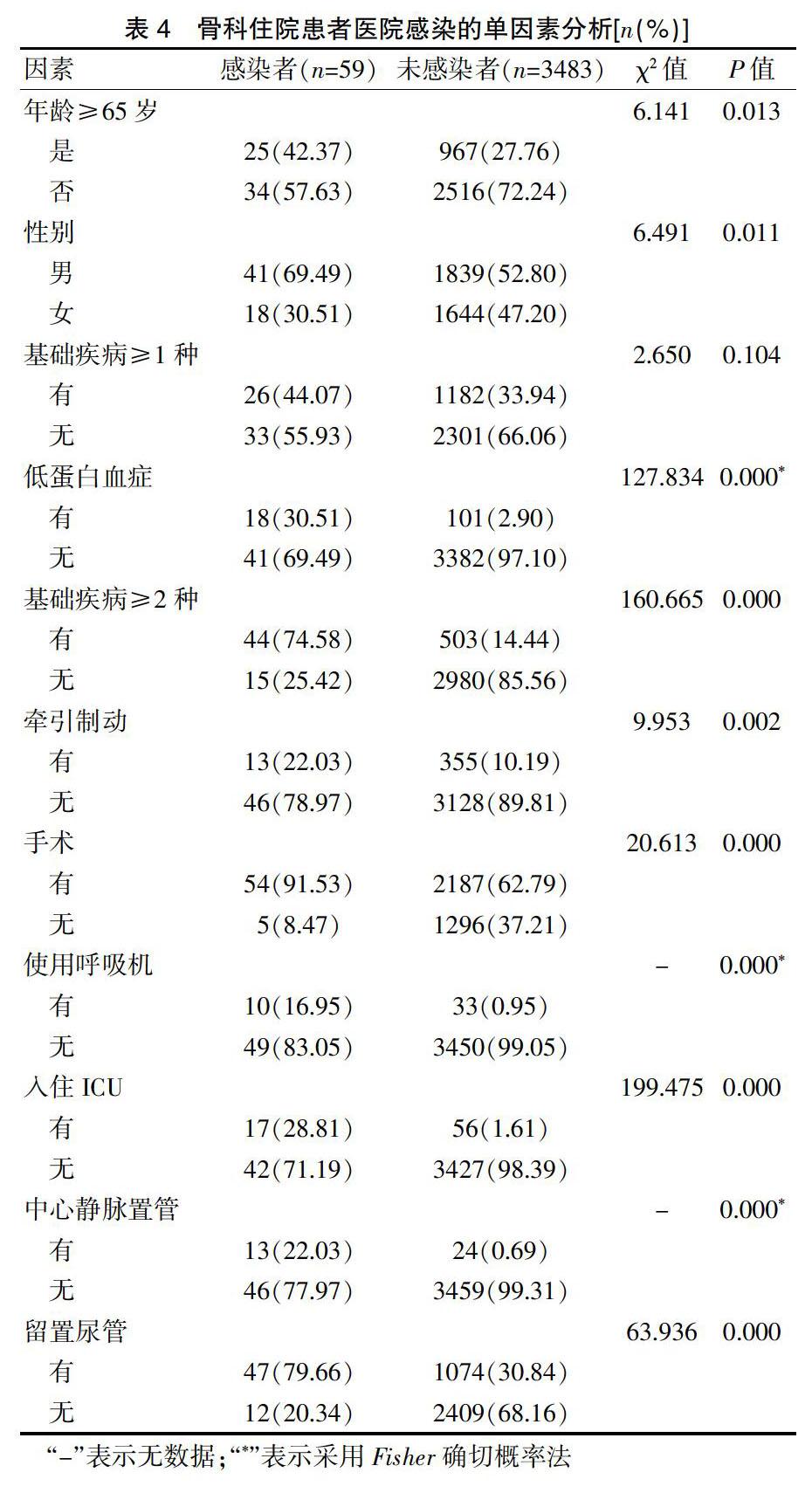
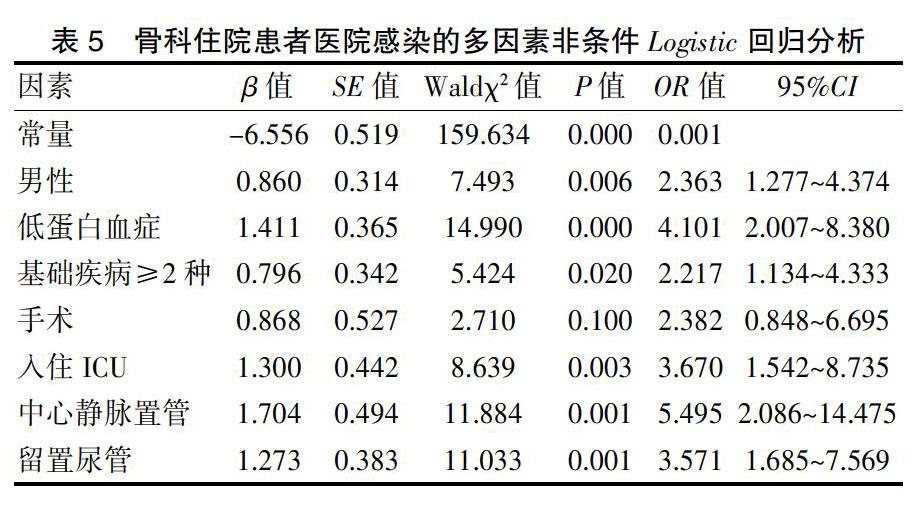
[摘要]目的 分析骨科住院患者醫院感染的临床特征与危险因素,为降低骨科医院感染发生率提供科学依据。方法 选取2017年9月1日~2018年8月31日于我院骨科住院的3542例患者作为监测对象,将其分为创伤(1295例)、关节(1075例)、脊柱(1172例)三个专业组,分析骨科住院患者医院感染的临床特点及危险因素。结果 骨科住院患者医院感染发生率(例次发生率)为1.67%(1.89%);创伤组的医院感染例次发生率为2.93%,高于关节组的1.58%和脊柱组的1.02%,差异有统计学意义(P<0.05)。医院感染部位构成前3位为下呼吸道(32.84%)、手术部位(31.34%)、泌尿道(20.90%);病原菌中革兰阴性菌、革兰阳性菌、真菌分别占50.00%、46.00%、4.00%,前3位病原菌为金黄色葡萄球菌(24.00%)、大肠埃希菌(20.00%)、鲍曼不动杆菌(12.00%)。感染者与未感染者的年龄≥65岁、性别、低蛋白血症、基础疾病≥2种、牵引制动、手术、使用呼吸机、入住ICU、中心静脉置管、留置尿管情况比较,差异有统计学意义(P<0.05);进一步多因素非条件Logistic回归分析显示,男性、低蛋白血症、基础疾病≥2种、入住ICU、中心静脉置管、留置尿管为骨科患者医院感染的独立危险因素(P<0.05)。结论 骨科住院患者医院感染具有以下呼吸道和手术部位感染为主、革兰阴性菌及革兰阳性菌感染比例相当、创伤患者医院感染率较高的特点,存在上述一种或多种危险因素的骨科住院患者发生医院感染风险较大,应积极治疗低蛋白血症、基础疾病,规范并减少侵入性操作等,以降低医院感染率。
[关键词]骨科;住院患者;医院感染;监测;危险因素
[中图分类号] R181.3 [文献标识码] A [文章编号] 1674-4721(2020)6(b)-0180-04
[Abstract] Objective To analyze the clinical characteristics and risk factors of nosocomial infection in hospitalized patients in orthopedic department, so as to provide scientific basis for reducing the incidence of nosocomial infection in orthopedic. Methods A total of 3542 patients who hospitalized in the orthopedic department from September 1, 2017 to August 31, 2018 in our hospital were selected as the monitoring objects and divided into three specialized groups: the trauma group (1295 cases), the joint group (1075 cases) and the spine group (1172 cases). The clinical characteristics and risk factors of nosocomial infection in orthopedic inpatients were analyzed. Results The incidence rate of nosocomial infection of orthopedic inpatients was 1.67% (the case number infection rate was 1.89%). The incidence rate of case number nosocomial infection in the trauma group was 2.93%, which was higher than that in the joint group (1.58%) and spine group (1.02%), the differences were statistically significant (P<0.05). The top three infection sites were lower respiratory tract (32.84%), surgical site (31.34%) and urinary tract (20.90%). Gram-negative bacteria, gram-positive bacteria and fungi accounted for 50.00%, 46.00%, and 4.00%, respectively. The top three pathogens were Staphylococcus aureus (24.00%), Escherichia coli (20.00%) and Acinetobacter baumannii (12.00%). The differences between the infected and uninfected patients in age (over 65 years old), gender, hypoproteinemia, basic diseases (more than 2 kinds), traction brake, surgery, use of ventilator, admission to ICU, central vein catheterization and indwelling catheter were statistically significant (P<0.05). Further multivariate unconditional Logistic regression analysis showed that male, hypoproteinemia, basic diseases (more than 2 kinds), admission to ICU, central vein catheterization and indwelling catheter were independent risk factors of nosocomial infection in orthopedic patients (P<0.05). Conclusion The nosocomial infection of orthopedic inpatients has the following characteristics: the mainly infection sites are lower respiratory tract and surgical site, the proportion of gram-negative bacteria and gram-positive bacteria is similar, and the nosocomial infection rate in trauma patients is higher. The risk of nosocomial infection of orthopedic inpatients with one or more of the above risk factors is higher. The hypoproteinemia and basic diseases should be actively treated, and invasive operation should be standardized and reduced, in order to reduce the nosocomial infection rate.
本研究结果显示,基础疾病≥1种与骨科住院患者医院感染无关,与文献[19-20]报道不符,可能与研究对象年龄偏大、基础疾病患病率高以及患者基础疾病控制较好有关。手术、牵引制动、年龄≥65岁、使用呼吸机在本研究中虽不是独立危险因素,但单因素分析显示这4个因素与骨科住院患者医院感染有较强的相关性,仍需要医护人员重视骨科患者围术期管理、卧床与高龄患者呼吸功能锻炼、呼吸机相关性肺炎预防等医院感染防控措施。
综上所述,骨科住院患者医院感染具有以下呼吸道和手术部位感染为主、革兰阴性菌及阳性菌感染比例相当、创伤患者医院感染发生率较高的特点,存在上述一种或多种危险因素的骨科住院患者发生医院感染风险较大,医护人员应劝导患者戒烟,积极治疗基础疾病与低蛋白血症,规范并减少侵入性操作等,以降低骨科患者医院感染发生率。
[参考文献]
[1]Spatenkova V,Bradac O,Fackova D,et al.Low incidence of multidrug-resistant bacteria and nosocomial infection due to a preventive multimodal nosocomial infection control:a 10-year single centre prospective cohort study in neurocritical care[J].BMC Neurol,2018,18(1):23.
[2]王华芳,向珮莹,潘泽英,等.老年住院患者医院感染经济损失的病例对照研究[J].中华医院感染学杂志,2018,28(8):1241-1244.
[3]吴晓英,丁丽娜,吴修建.多重耐药鲍曼不动杆菌所致医院感染的直接经济损失研究[J].中国感染控制杂志,2018, 17(8):735-738.
[4]魏燕,张翠红,谭桃,等.脊柱手术患者术后医院感染的临床特点与影响因素及预防[J].中华医院感染学杂志,2018, 28(24):3804-3807.
[5]中华人民共和国卫生部.医院感染诊断标准(试行)[S].北京,2001.
[6]Rosenthal VD,Rodrigues C,Alvarez-Moreno C,et al.Effectiveness of a multidimensional approach for prevention of ventilator-associated pneumonia in adult intensive care units from 14 developing countries of four continents:Findings of the International Nosocomial Infection Control Consortium[J].Crit Care Med,2012,40(12):3121-3128.
[7]杨心怡,朱会英,索继江,等.综合性医院骨科医院感染危险因素分析[J].中华医院感染学杂志,2016,26(16):3752-3754.
[8]吴丽红,师靓,李刚,等.骨科手术患者术后医院感染相关因素分析[J].中华医院感染学杂志,2018,28(20):3120-3123.
[9]李坚,张金喜,李敏皋,等.骨科老年患者术后医院感染相关因素及预防策略分析[J].中华医院感染学杂志,2018, 28(6):876-878.
[10]Durand F,Berthelot P,Cazorla C,et al.Smoking is a risk factor of organ/space surgical site infection in orthopaedic surgery with implant materials[J].Int Orthop,2013,37(4):723-727.
[11]Foo YZ,Nakagawa S,Rhodes G,et al.The effects of sex hormones on immune function:a meta-analysis[J].Biol Rev Camb Philos Soc,2017,92(1):551-571.
[12]Parmentierdecrucq E,Nseir S,Makris D,et al.Accuracy of leptin serum level in diagnosing ventilator-associated pneumonia:a case-control study[J].Minerva Anestesiol,2014,80(1):39-47.
[13]Bohl DD,Shen MR,Kayupov E,et al.Hypoalbuminemia independently predicts surgical site infection,pneumonia,length of stay,and readmission after total joint arthroplasty[J].J Arthroplasty,2016,31(1):15-21.
[14]Richards JE,Kauffmann RM,Zuckerman SL,et al.Relationship of hyperglycemia and surgical-site infection in orthopaedic surgery[J].J Bone Joint Surg Am,2012,94(13):1181-1186.
[15]成鵬,周海宇,尹晓莉,等.中国人群脊柱术后手术部位感染相关危险因素的Meta分析[J].中国脊柱脊髓杂志,2017,27(8):704-713.
[16]蒋晓霞,陈坤,杨梅,等.骨科手术患者术后感染危险因素的病例对照研究[J].预防医学,2018,30(3):232-235, 239.
[17]杨楠,马雄心,杨文选,等.骨科植入术后患者医院感染临床特征与实施流程化管理的控制研究[J].中华医院感染学杂志,2015,25(23):5444-5446.
[18]宋维海,邓国超,沈建新,等.骨科住院患者医院感染特点与预防[J].中医药管理杂志,2017,25(10):89-91.
[19]Zhang J,Zhao T,Long S,et al.Risk factors for postoperative infection in Chinese lung cancer patients:A meta-analysis[J].J Evid Based Med,2017,10(4),255-262.
[20]Bohl DD,Saltzman BM,Sershon RA,et al.Incidence,risk factors,and clinical implications of pneumonia following total hip and knee arthroplasty[J].J Arthroplasty,2017,32(6):1991-1995.
(收稿日期:2019-11-01 本文编辑:任秀兰)