The relationship between diabetes‑related distress and self‑management in empty‑nest elderly patients with type 2 diabetes mellitus: The mediating effect of self‑efficacy
Hui‑Wen XU, Yuan YUAN, Lin LIU,En TAKASHI, Kitayama AKIO, Xin LI
1Department of Medical Nursing, School of Nursing, Yangzhou University, Yangzhou, China; 2Department of Basic Medicine and Nosography, Nagano College of Nursing, Komagane,Nagano, Japan; 3Department of Respiration, Affiliated Hospital of Yangzhou University, Yangzhou, China
ABSTRACT
Objective: The aim of this study is to investigate the mediating effect of self‑efficacy between diabetes‑related distress and self‑management in empty‑nest elderly patients with type 2 diabetes mellitus (T2DM).
Methods: A total of 347 empty‑nest elderly patients with T2DM from Jiangsu Province Hospital of Chinese Medicine and Affiliated Hospital of Yangzhou University were investigated by a self‑designed General Information Questionnaire, the Self‑efficacy for diabetes, the Diabetes Distress Scale, and the summary of diabetes self‑care activities.Diabetes‑related distress and diabetes self‑management were tested for correlation analysis with self‑efficacy.Meditational analyses were conducted to test the hypothesized mediating effects of diabetes self‑efficacy as an intervention variable between diabetes distress and self‑management.
Results: About 68.59% of patients suffered from diabetes‑related distress.The results of bivariate correlations revealed that self‑efficacy was negatively correlated with diabetes‑related distress (r =–0.627, P < 0.01) and positively correlated with self‑management (r = 0.356, P < 0.01).The relationship effects of diabetes distress on self‑management were fully mediated by self‑efficacy.
Conclusions: Diabetes‑related distress prevails in empty‑nest elderly patients with T2DM.Self‑efficacy plays a mediate role between diabetes‑related distress and self‑management.Psychological intervention is contributed to reducing diabetes‑related distress.
Keywords: Diabetes mellitus, empty nest elderly, mediating effect, self‑efficacy
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is one of the most common chronic and metabolic diseases indicated by elevated level of blood glucose due to insulin deficiency and resistance.International diabetes federation (IDF) reported that 451 million people had diabetes in the world in 2017.It is estimated that the figure will grow up to 693 million by 2045, among which the number of diabetes patients in China has reached 114.4 million, ranking the first in the world, and is expected to rise to 119.8 million by 2045.[1]The latest data from the Chinese Office of the National Working Committee on Aging reported that the number of local residents over 60 years old in Jiangsu province was 16.2302 million by the end of 2017, among which 52% were empty nesters.[2]The world population is growing and aging.Diabetes prevalence among empty nesters is increasing year by year.[3]The prevalence of diabetes among empty‑nested elderly people is 7.33% to 18.7%, ranking among the top 3 of chronic noncommunicable diseases.[4]
Diabetes is a kind of lifelong chronic disease, long‑term self‑management is needed to improve glycemic control,[5]which may affect the patients’ normal life, and may lead to their mental burden and psychological pressure, which is easy to produce diabetes‑related distress.An investigation showed that the incidence of diabetes‑related distress was 18% to 45%,[6]which affected the treatment adherence, self‑management behavior, glycemic control, and quality of life of patients with diabetes.[7‑9]The guidelines of the IDF and the American Diabetes Association both emphasize the importance of psychological problems of diabetes patients.[1,10]For a long time, psychological research on patients with diabetes has focused on anxiety and depression, and diabetes‑related distress has been neglected.Only 23.7% of patients with diabetes‑related distress have been treated by the health team,[1]which indirectly reflects that most of the medical staff do not have an ideal understanding of diabetes‑related distress.
Diabetes‑related distress reflects the psychological stress of patients during the self‑management of diabetes, and it is a negative emotional response toward stress which is different from depression and anxiety.[11]Empty‑nested elderly people are more likely prone to psychological problems and psychological disorders due to the change of family structure and the lack of social support.The previous research has shown that patients could carry out self‑management effectively if he/she has a good psychological state.[12]Fisheret al.[13]found that it was diabetes‑related distress instead of depressive symptoms or depression that significantly associated with self‑management.
Currently, the reported research has proved the positive correlation between self‑management and diabetes‑related distress in diabetic patients.The previous study[14]demonstrates that improving self‑efficacy can prompt patients to adopt a positive attitude to cope with the disease and improve their self‑management level.The correlation ship between diabetes‑related distress and self‑efficacy was also proved.[15]However, it remains unclear that how diabetes‑related distress affect self‑management? Is there any other mediating factor between them? As a result, we made a hypothesis that less distress level would improve patients’ self‑efficacy, which, in turns, leads to improve the patients’ self‑management level.
The purpose of this study was to explore the mediating effect of self‑efficacy between self‑management and diabetes‑related distress of empty‑nest elderly people with T2DM.We intend to improve our understanding of the relationship of those 3 variables and to provide a reference for the intervention to improve the self‑management level of empty‑nest elderly patients with T2DM.
METHODS
Participant recruitment
The cross‑sectional data were collected from two clinical centers from January 2017 to January 2018: Jiangsu Province Hospital of Chinese Medicine, located in Nanjing city, and the Affiliated Hospital of Yangzhou University, located in Yangzhou city.The inclusion criteria for participants included: (1) inpatients or outpatients who aged ≥60 years old; (2) patients had a diagnosis of T2DM; (3) patients stay alone or stay with their spouses only; (4) patients can read or speak Chinese; and (5)patients have normal cognitive function.Patients who met the inclusion criteria and agreed to participate in the study were sent the questionnaire, which include informed consent.They were asked to complete and return the survey and informed consent immediately after they finished.
Measurement
General information questionnaire
The self‑designed general information questionnaire was used to evaluate the demographic variables, including age,gender, education, dwelling condition, and so forth.At the same time, the duration of diabetes was collected from the patients’ self‑report.Previous information related to the disease was also investigated, including complications,glucose, and how many times of inpatient.
Self‑efficacy for diabetes
The self‑efficacy for diabetes (SED) was designed by Loriget al.[16]in 1999, which is used for measuring the level of self‑efficacy in diabetic people.It contains 8 items,including exercise management, diet management, glucose management, disease control, and so forth.All statements were measured on a 10‑point Likert scale from 1 = not confident at all to 10 = absolutely confident.The mean score of the 8 items was used, with higher scores indicating more self‑efficacy.SED was translated into the Chinese version by Sun[17]in 2010.Cronbach’s alpha for the Chinese version was 0.75, and it is used for free in China.[17]
Diabetes Distress Scale
The Diabetes Distress Scale (DDS) is a 17‑item scale designed by Polonskyet al.[18]in 2005.It was developed to measure diabetes‑related distress in 4 domains, including emotional burden, regimen‑related distress, physician‑related distress,and interpersonal distress.Responses were recorded on a 6‑point Likert scale ranging from 1 = no problem to 6 = very serious problem.The scores for emotional burden,regimen‑related distress, physician‑related distress, and interpersonal distress range from 5 to 30, 5–30, 4–24, 3–18,respectively, and the overall DDS score ranges from 17 to 102.The mean score of the 17 items was used, with higher scores indicating greater distress.In 2010, Yanget al.[19]introduced it to China.The coefficient of internal consistency reliability of the Chinese version of the total scale and the 4 subscales were 0.842–0.951, and the retest reliability of the total scale was 0.849.The Chinese version of DDS is freely used in China.[19]
Summary of diabetes self‑care activities
Summary of diabetes self‑care activities (SDSCA) was developed by Toobertet al.[20]in the year 2000.It was designed especially for the elderly with diabetes who were over 60 to assess their self‑management level.The scale contains 6 domains, including diet control, exercise, glucose monitoring,foot care, medication adherence, and smoking.There were 13 items in total.Participants were asked about their recent diabetes care behaviors.Responses were from 0 to 7 for each item.Higher scores indicate better self‑management.Sunet al.[21]introduced it to China in 2011.The content validity index of the Chinese version was 1.00.Cronbach’s alpha of each domain was in the range of 0.62–0.92.The Chinese version of SDSCA is freely acceptable.[21]
All the survey were conducted by the nurses worked in these two hospitals, they were all trained by the research manager before the investigation so as to be eligible to carry out the survey.
Ethical considerations
The participants would be told about the aims, methods,and benefits of the investigation before they fill the questionnaires.Moreover, the patients would be asked to sign an informed consent if they agree to participate.
Statistical analysis
The collected data were entered into a database with EpiData 3.1 software (EpiData Association,http://www.epidata.dk).Data analysis was undertaken using SPSS 20.0 (IBM Corporation,New York, NY).Frequency and percentages were used to describe categorical variables.Mean ± standard deviation (SD)was used to present continuous variables.Bivariate correlations were performed on all variables used in the linear regression models.Spearman correlation analysis was adopted if the data were normally distributed, and Pearson correlation analysis was adopted, otherwise.To test whether self‑efficacy mediated the relationship between diabetes‑related distress and self‑management, regression analysis was employed.The mediating effect was analyzed by multiple linear regressions.Two‑tailedP <0.05 was considered statistically significant.
RESULTS
Characteristics of participants
Initially, we distributed 400 questionnaires.After the distribution‑return process, 347 questionnaires were returned at a rate of 86.75%.Among the returned questionnaires, all of them were valid at a rate of 100%.The general characteristics of the participants are shown in Table 1.
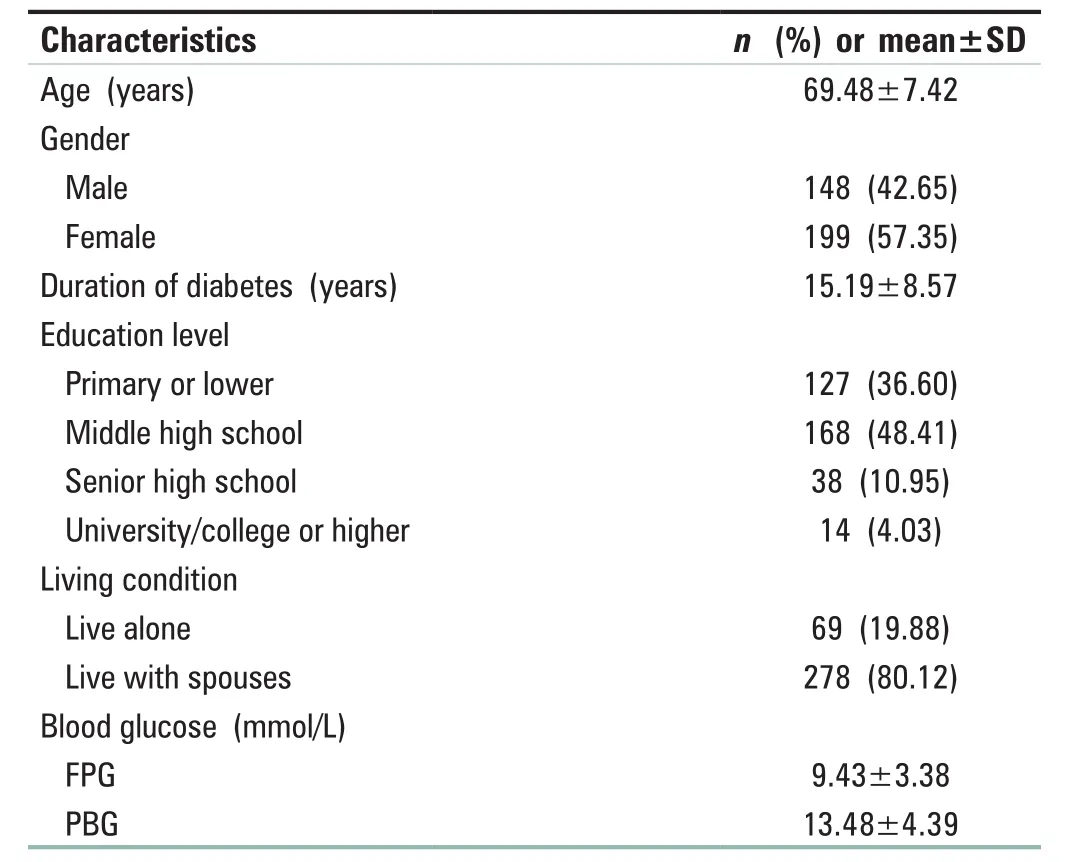
Table 1: General characteristics of the participants (n=347)
Descriptive statistics of self‑efficacy, self‑management,and diabetes‑related distress
Means and SDs for all measures are represented in Table 2.
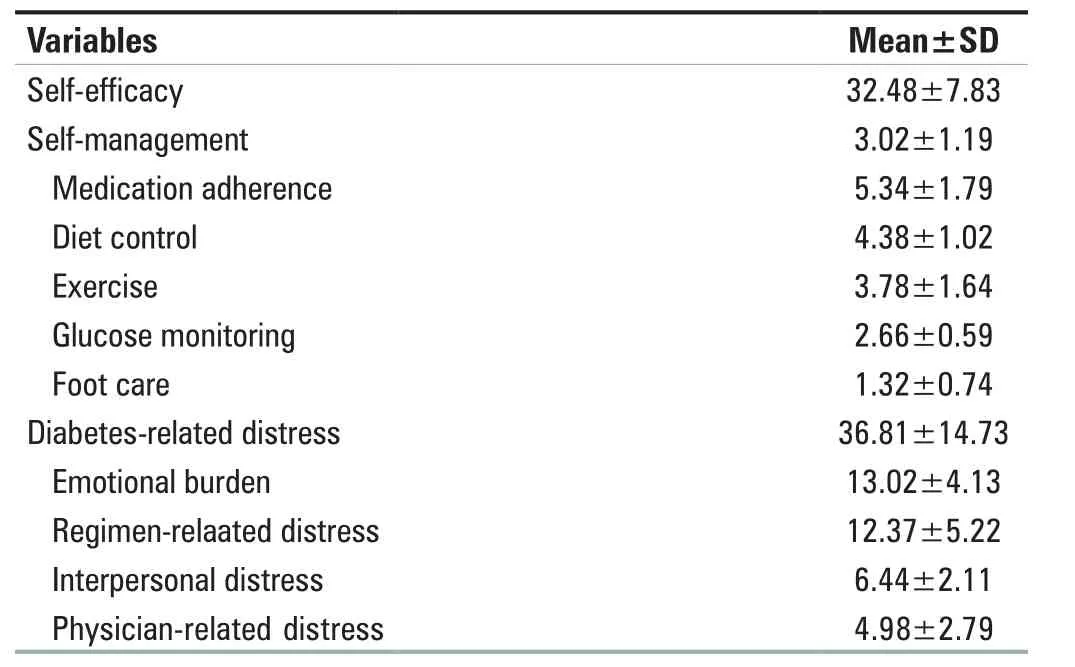
Table 2: Scores of self‑efficacy, self‑management and diabetes‑related distress (n=347)
The correlations between self‑efficacy, self‑management,and diabetes‑related distress
Table 3 indicates all correlations were statistically significant.In particular, diabetes‑related distress had negative correlations with both self‑management (r= −0.351,P< 0.01) and self‑efficacy (r= −0.627,P< 0.01).However, self‑efficacy was positively associated with self‑management (r= 0.356,P< 0.01).
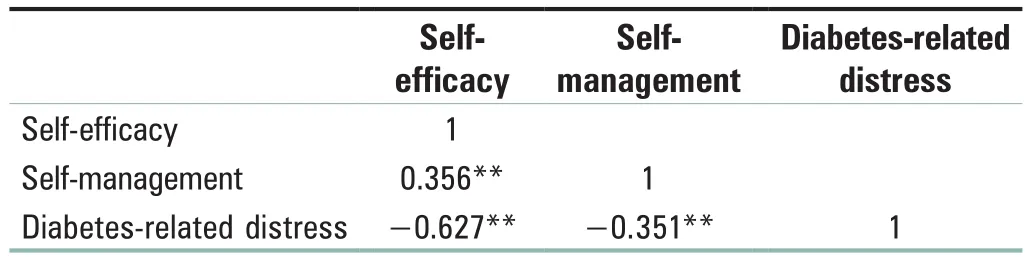
Table 3: The correlations between self‑efficacy,self‑management and diabetes‑related distress
Measurement model
To test whether self‑efficacy mediated the relationship between diabetes‑related distress and self‑management, regression analysis was employed.The first regression equation evaluated whether diabetes‑related distress indices (the independent variable) predicted self‑management (the dependent variable).The second regression equation tested the relationship between diabetes‑related distress and self‑efficacy (the mediator).In step 3, the self‑efficacy was induced in the structural equation modeling.The results are summarized in Table 4 and Figure 1.The results of the regression analysis showed that self‑efficacy fully mediated the relationship between diabetes‑related distress and self‑management.

Table 4: Results of indirect effects of self‑efficacy mediation models

Figure 1: Self‑efficacy mediation models between diabetes‑related distress and self‑management.Notes: a × b: Mediating effect; c: Total effect; c’: Direct effect; **P < 0.001, *P < 0.05
DISCUSSION
Self‑efficacy is defined as “the conviction that one can successfully execute the behavior required to produce the outcomes.”[22]Our findings suggest that higher diabetes‑related distress level may depress the sense of personal self‑efficacy in T2DM empty‑nest elderly patients.The reasons may lie in the following: First, these people lack satisfactory social relationships and the necessary social support, leading to their low ability to attain goals, and thus more experience of failure.[23]The Chinese usually pay more attention to social relationships and social interaction.[24]As empty nesters lack satisfying social relationships and have little social support, they are more likely to suffer from stress.Second, diabetes mellitus is a lifelong disease and it could not be cured nowadays.To manage the disease well, strict control of diet, regular exercises, self‑monitoring of glucose,and medication adherence are required.The patients suffer from diabetes as well as its complications all the life, which,as a result, people tend to have negative psychology, leading to a lower level of self‑efficacy.
Diabetes‑related distress is defined as the patient’s concerns about self‑management of diabetes, perception of support,emotional burden, and access to quality health care.[25]The study demonstrates a large number of participants have diabetes‑related distress (68.59%).The mean score of the total DDS was (36.81 ± 14.73), which was higher than the result reported in the previous study.[14]The reason may be related to the lower education level, longer diabetic duration, and more implications of the participants.Qin’s study[26]shows that education level, disease duration and complications are independent risk factors for diabetes‑related distress.
DDS can not only assess overall diabetes‑related distress but also pinpoint the specific nature of the distress.It provides an opportunity to assess the personal and environmental influences in diabetic patients.The research shows emotional burden and physician‑related distress were the top two crucial aspects of diabetes‑related distress.Nurses and diabetes educators should assist in finding strategies to provide psychological support.For the physicians, they may be able to communicate with the patients more about their disease to improve their understanding of diabetes.Which,as a result, reduces their diabetes‑related distress.
It is complex to manage diabetes mellitus.Patients need to change their original behaviors so as to improve health outcomes.Table 2 illustrates the mean score of the total SDSCA was (3.02 ± 1.19), which was lower than Heet al.’s research.[27]Once a person was diagnosed with diabetes mellitus, he/she have to learn the skills and strategies necessary for self‑management and persist in managing their disease.As for the empty‑nest elderly people, they live alone or with their own spouses.Some of their children live far away from them and come back home less than once a year, which means they can only rely on themselves to manage their diabetes.However, most of the elderly have little access to the methods of diabetes management, leading to their poor self‑management of diabetes.A systematic review reported that quality of life was improved following interventions targeting the improvement of self‑management.[28]Thus,it is important to create interventions that reduce distress so as to improve self‑management.Building a comfortable relationship with their families and companions may allow patients to discuss their stress, master practical skills, which,in turn, relive their burden and psychological stress and become more confident in self‑management.Consequently,the ability of diabetes management would also be improved.
Previous researchers have examined the interactions between self‑efficacy and self‑management in patients with T2DM and analyzed their correlated or independent effects.For instance, Krichbaumet al.[29]and Sarkaret al.[30]have found that a high self‑efficacy level is positively associated with self‑management in diabetic patients.Thus, T2DM patients with higher self‑efficacy are prone to engage in self‑management behaviors.[31]Likewise, our data revealed that self‑efficacy was positively correlated with self‑management.Patients with low self‑efficacy tend to believe that they are incompetent, depressed, and lose motivation and confidence in self‑management.On the contrary, the higher self‑efficacy,the more confident the patient will be to overcome difficulties and challenges, the more persistent and firm in the process of diabetes management.[32]Consequently, they would be able to cope with adverse factors during managing diabetes.Therefore, the level of self‑management may be improved.
Our study also revealed that self‑efficacy was negatively correlated with diabetes‑related distress, which is consistent with the research results of Wardian and Sun.[33]Their research indicates that high self‑efficacy is associated with reduction in diabetes‑related distress.Patients with higher self‑efficacy would have better control of glucose, which is conducive to improving the hope level of patients to treat the disease, thus reducing diabetes‑related distress.[34]Therefore, in the nursing process, nurses need to consider the effect of self‑efficacy on diabetes‑related disease, and try to improve the patients’ self‑efficacy and enhance the patients’confidence to overcome the disease, so as to reduce the level of diabetes‑related distress, promote the physical and mental health of patients, and improve the quality of life.
The primary findings of this study confirm our hypothesis that diabetes‑related distress significantly affects self‑management,and the effect is fully mediated by self‑efficacy.The multiple linear regression suggests that less diabetes‑related distress may strengthen the empty‑nest elderly patients’self‑efficacy, which in turns, results in improving their ability of self‑management.So the study highlights the importance of reducing diabetes‑related distress.Less distress would cultivate patients’ positive attitude towards disease and strengthen their belief and confidence to solve the problem in the process of diabetes management.Such internal change, that is, improved self‑efficacy, is important for T2DM patients to maintain sustained, positive behavior changes.[35]For example, adhering to treatment regiment,exercising regularly, eating healthily, and so forth.In general,our finding indicates that diabetes‑related stress has a direct effect in patients’ self‑motivation in managing diabetes, and this improved self‑efficacy could translate into improved diabetes self‑care activities, which result in a better quality of life.It is also likely that diabetes‑related stress affects patients’ self‑management, but such effects might be quite small when self‑efficacy’s strong impact on self‑management is accounted for.
The research results indicate that when the medical personnel take actions to improve T2DM patients’ self‑management,self‑efficacy, and diabetes‑related disease should also be assessed.Trying suitable interventions to reduce the patients’diabetes‑related disease, such as peer education, motivated interview.Thus, the self‑efficacy and self‑management may be improved at the same time.As a result, patients’ quality of life would be improved.
Limitations
Our study has some limitations.First, the generalizability of the outcome is limited because our sample was small (only 347 cases).Moreover, all the patients were from only 2 sites,which mean that our participants could not represent the broader population of T2DM empty‑nest elderly patients in China.Second, our findings might suffer from self‑report bias, just like all the studies based on data collected from self‑completed questionnaires Third, this study only discussed the mediating effect of self‑efficacy between psychological pain and self‑management, and the role of other mediating variables needs to be further studied.However, the limitations would not be a serious threatens to our results.Further research, including replication studies and explorations of other factors, is needed.
CONCLUSIONS
The study clarifies the mediating role of self‑efficacy in T2DM empty‑nest elderly patients between diabetes‑related distress and self‑management.Our finding indicates that nurses should recognize diabetes‑related distress as a key element in nursing process aimed at improving the patients’ ability of self‑management.As a result, the patients’ quality of life would be improved.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.In the form, the patients have given their consent for clinical information to be reported in the journal.The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Acknowledgments
The authors would like to thank all the nurses involved in the research for their collaboration in the questionnaires collection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 Journal of Integrative Nursing2020年3期
Journal of Integrative Nursing2020年3期
- Journal of Integrative Nursing的其它文章
- Impact of the emigration of nurses on health care delivery system in selected hospitals, Benin‑City, Edo State, Nigeria
- A bibliometric analysis of nursing research in COVID‑19 in China
- Effect of flapping‑meridians combined with thunder‑fire moxibustion on upper limb dysfunction after stroke
- Clinical effect of scraping therapy in the treatment of knee osteoarthritis
- Competence investigation on insulation testing on electrosurgical instruments and needs analysis of training for Central Sterile Supply Department staff
- Establishment and management of neurosurgery emergency observation ward during the COVID‑19 epidemic period
