Combined surgical and interventional treatment of tandem carotid artery and middle cerebral artery embolus: A case report
Meng Zhang, Ji-Heng Hao, Kai Lin, Qing-Ke Cui, Li-Yong Zhang, Department of Neurosurgery,Liaocheng Brain Hospital, Liaocheng 252000, Shandong Province, China
Abstract
BACKGROUND
The 2018 American Heart Association/American Stroke Association guidelines for early management of acute ischemic stroke recommend the use of retrievable stents for mechanical thrombectomy in patients with acute internal carotid artery or middle cerebral artery M1 occlusion that can be treated within 6 h from onset.For cases of carotid artery with ipsilateral middle cerebral artery tandem embolization, the operation is more complicated and challenging. We here report a case of a tandem embolism, and the anatomy of the aortic arch was complex.Direct carotid artery incision and thrombectomy can not only prevent the escape of the carotid embolus but also save time during establishment of the thrombectomy access.
CASE SUMMARY
The patient was a 70-year-old man. He was admitted to hospital due to sudden inability to speak and inability to move his right limb for 3 h. Imaging confirmed a diagnosis of a tandem embolism in the left carotid artery with left M1 occlusion.Carotid artery incision thrombectomy combined with stent thrombectomy was performed. The operation was successful, and 24 h later the patient was conscious and mentally competent but had motor aphasia. His bilateral limb muscle strength level was 5, and his neurologic severity scores score was 2.
CONCLUSION
Carotid artery incision thrombectomy combined with stenting for carotid artery plus cerebral artery tandem embolization is clinically feasible. For patients with a complicated aortic arch and an extremely tortuous carotid artery, carotid artery incision can be chosen to establish the interventional path.
Key words: Carotid artery incision thrombectomy; Mechanical thrombectomy; Carotid thrombosis; Middle cerebral artery occlusion; Tandem occlusion; Case report
INTRODUCTION
The 2018 American Heart Association/American Stroke Association guidelines for early management of acute ischemic stroke recommend the use of retrievable stents for mechanical thrombectomy in patients with acute internal carotid artery or middle cerebral artery M1 occlusion that can be treated within 6 h from onset[1]. Few cases of carotid artery combined with ipsilateral middle cerebral artery tandem embolism,have been reported. In addition, the operation is more complex and challenging, and the prognosis of such patients is poor[2]. We treated a case of carotid artery combined with middle cerebral artery tandem embolization with carotid artery incision thrombectomy combined with stenting. The result was satisfactory.
CASE PRESENTATION
Chief complaints
A 70-year-old man complained of sudden inability to speak and inability to move his right limb for 3 h.
History of present illness
A history of atrial fibrillation for more than 1 year.
Personal and family history
No history of hypertension, diabetes, coronary heart disease or other chronic diseases.There was no similar event or known genetic history in his family.
Physical examination
The patient presented with drowsiness and complete mixed aphasia. The right nasolabial groove had become shallow, and his mouth was askew to the left. His left limb was movable, and the right limb was unmovable. The muscle tension of the extremities was normal, and pathological signs on the right side were positive. His baseline neurologic severity scores (NHISS) score was 23.
Imaging examination
Electrocardiogram examination showed atrial fibrillation. Head and neck computed tomography angiography (CTA) showed embolisms in the left carotid bifurcation and left middle cerebral artery. Brain computed tomography showed a small infarct in the left insular lobe (Figure 1).
Laboratory examination
Blood routine examination and coagulation mechanism showed no obvious abnormalities.
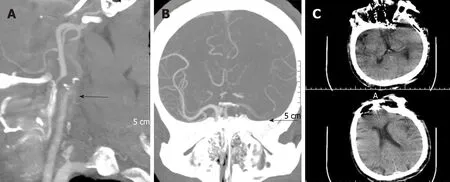
Figure 1 Head and neck computed tomography angiography and brain computed tomography findings. A: Computed tomography angiography (CTA) of the neck showing an embolism at the left carotid bifurcation; B: Intracranial CTA showing an embolism in the upper trunk of the left middle cerebral artery; C: Brain computed tomography showing a small infarction in the left insular lobe; the Alberta Stroke Program Early CT Score was 9.
FINAL DIAGNOSIS
Carotid artery combined with ipsilateral middle cerebral artery acute tandem embolism.
TREATMENT
Alteplase was administered at a dose of 0.9 mg/kg 200 min after symptom onset.Revascularization was initiated 210 min after onset. Cerebral angiography showed a type III aortic arch, where the left common carotid artery shared the main trunk with the brachiocephalic trunk. A Simmon 2 angiography catheter was placed for left common carotid artery angiography. The left external carotid artery was not visible,and the left internal carotid artery showed slow blood flow. Thrombosis at the beginning of the internal carotid artery and occlusion of the upper trunk of the left middle cerebral artery was considered. The left anterior cerebral artery provided secondary compensatory blood supply to the left middle cerebral artery (Figure 2).Repeated attempts were made to place the 8F guiding catheter into the left common carotid artery, which took 40 min. The 8F guiding catheter was aspirated at the bifurcation of the left carotid artery, and no reverse bleeding was observed. A percutaneous carotid artery incision was made to remove the thrombus in the neck under direct vision, and it only took 20 min (Figure 3). The left carotid artery was sutured, and angiography showed that the thrombosis in the bifurcation of the carotid artery had disappeared and that the internal and external carotid arteries were unblocked. Using the Solitaire intermediate catheter for mechanical thrombectomy , a 5Fr Navien intermediate catheter was placed across the carotid bifurcation into the petrosal segment. The left middle cerebral artery clot was removed with a Solitaire FR 6–30 mm. After two attempts, the patient was re-examined by angiography, which revealed middle cerebral artery blood flow recanalization, with modified thrombolysis in cerebral infarction score level III (Figure 4).
OUTCOME AND FOLLOW-UP
Neurological examination was performed 24 h after the operation. The patient was conscious and mentally competent, accompanied by motor aphasia. His bilateral limb muscle strength level was 5, and his NHISS score was 2. Brain magnetic resonance imaging showed small infarcts in the frontal and temporal lobes (Figure 5).Pathological examination of the thrombus showed a mixed thrombus (Figure 6). His mRS score was 0 at 3 mo of follow-up (Table 1).
DISCUSSION
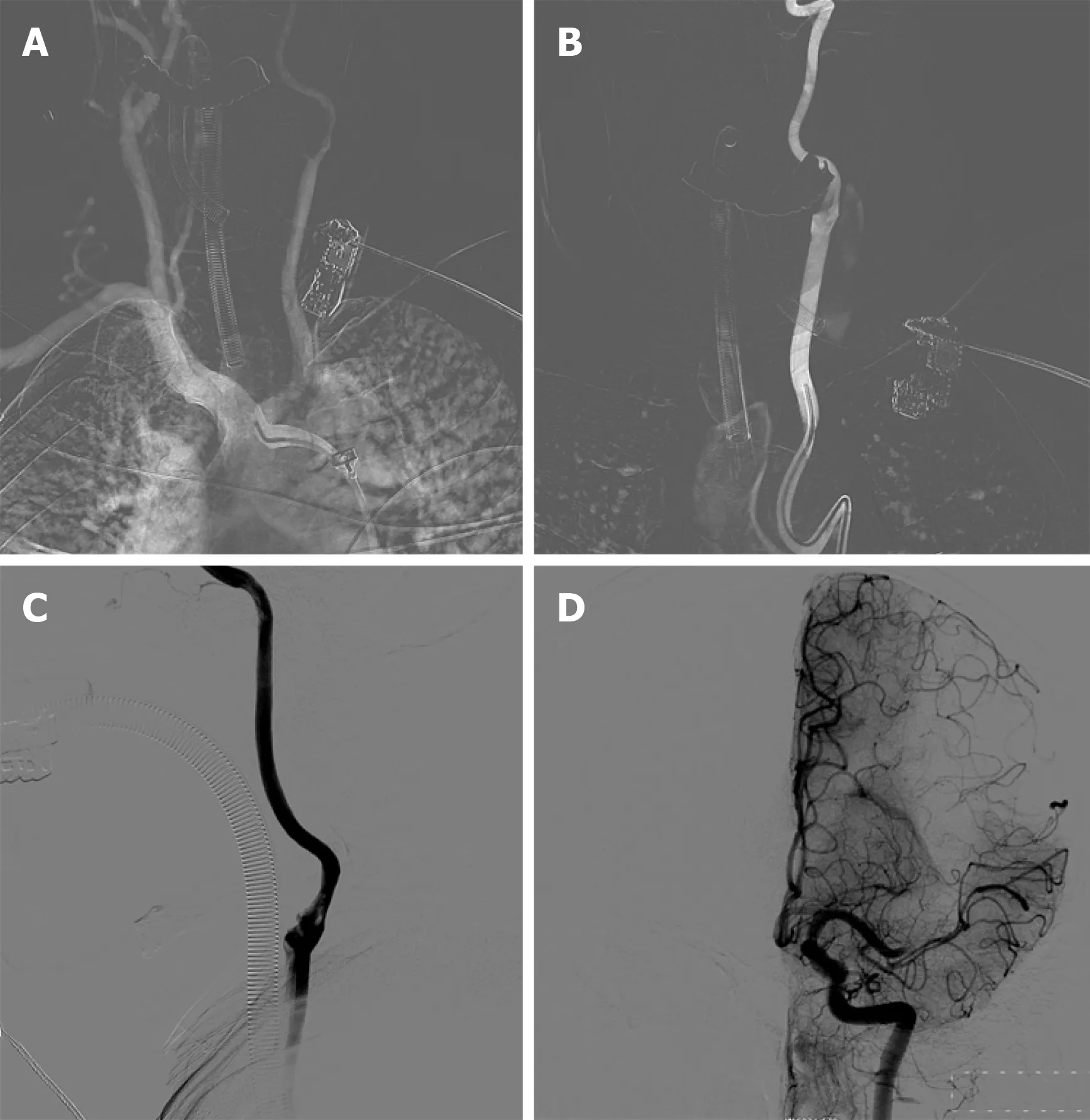
Figure 2 Intracranial angiography findings. A: Subaortic arch angiography shows a type III aortic arch where the left common carotid artery shares the main trunk with the brachiocephalic trunk; B: Simmon 2 catheterangiography showing that the left external carotid artery was not visible, and the left internal carotid artery showing slow blood flow; C: There was a thrombus at the beginning of the left internal carotid artery; D: The upper trunk of the left middle cerebral artery was occluded, but the anterior cerebral artery compensated for the blood supply of the middle cerebral artery via the lateral branches of the meninges.
Severe acute ischemic stroke is often caused by acute tandem occlusion of the internal carotid artery and the ipsilateral middle cerebral artery. External carotid artery occlusion is mainly caused by arterial dissection and atherosclerotic plaques[3].Ipsilateral middle cerebral artery occlusion is usually caused by thrombus or plaque detachment in the lesion site near the internal carotid artery[4-6]. Treatment for patients with such tandem occlusions has been reported at several centers[7-9]. Balloon dilatation or combined stenting was used to treat the occlusion of the external segment of the internal carotid artery, and mechanical thrombectomy was used to solve the occlusion of the ipsilateral middle cerebral artery. It has also been reported that due to the hardness of the plaque in the initial segment of the internal carotid artery, various microcatheter and guidewire techniques were attempted but could not pass through the occlusion site of the external cranial segment of the internal carotid artery. Carotid artery puncture was performed to establish thrombectomy access.Mechanical thrombectomy of the ipsilateral middle cerebral artery occlusion was performed first, and carotid endarterectomy was then performed to treat the internal carotid artery lesions[10]. One study evaluated outcomes and feasibility of carotid artery stenting versus carotid endarterectomy, and performed both procedures in the same patient. Carotid endarterectomy confirms its efficacy in carotid revascularization, but carotid artery stenting constitutes a good alternative when the procedures are selected based on patient-specific risk factors[11].
The case reported here is considered to be due to embolic events and is thus different from tandem occlusion due to atherosclerotic plaques and arterial dissection.It is also different from the occlusion of the internal carotid artery and middle cerebral artery caused by a high load embolism. The embolus in this patient was located in the bifurcation of the carotid artery and the ipsilateral middle cerebral artery, and no obvious embolus was found in the remaining internal carotid artery, so there was positive blood flow in the internal carotid artery. If a carotid artery embolization is treated with carotid stent implantation in such patients, it may result in distal escape of the thrombus. Studies have shown that aortic arch and proximal carotid artery anatomic factors seriously affect the time required for thrombectomy and are independent risk factors leading to a poor prognosis[12,13]. Carotid puncture is an option. It is difficult to stop the bleeding after postoperative removal of the artery sheath tube after carotid artery puncture. Niiet al[14]applied percutaneous carotid artery puncture for intracranial aneurysm embolization in 27 patients, and 4% of the patients developed a neck hematoma after surgery. In this case, the thrombus was located at the bifurcation of the carotid artery, and percutaneous carotid artery puncture was likely to cause embolus shedding and embolization of the distal blood vessel.
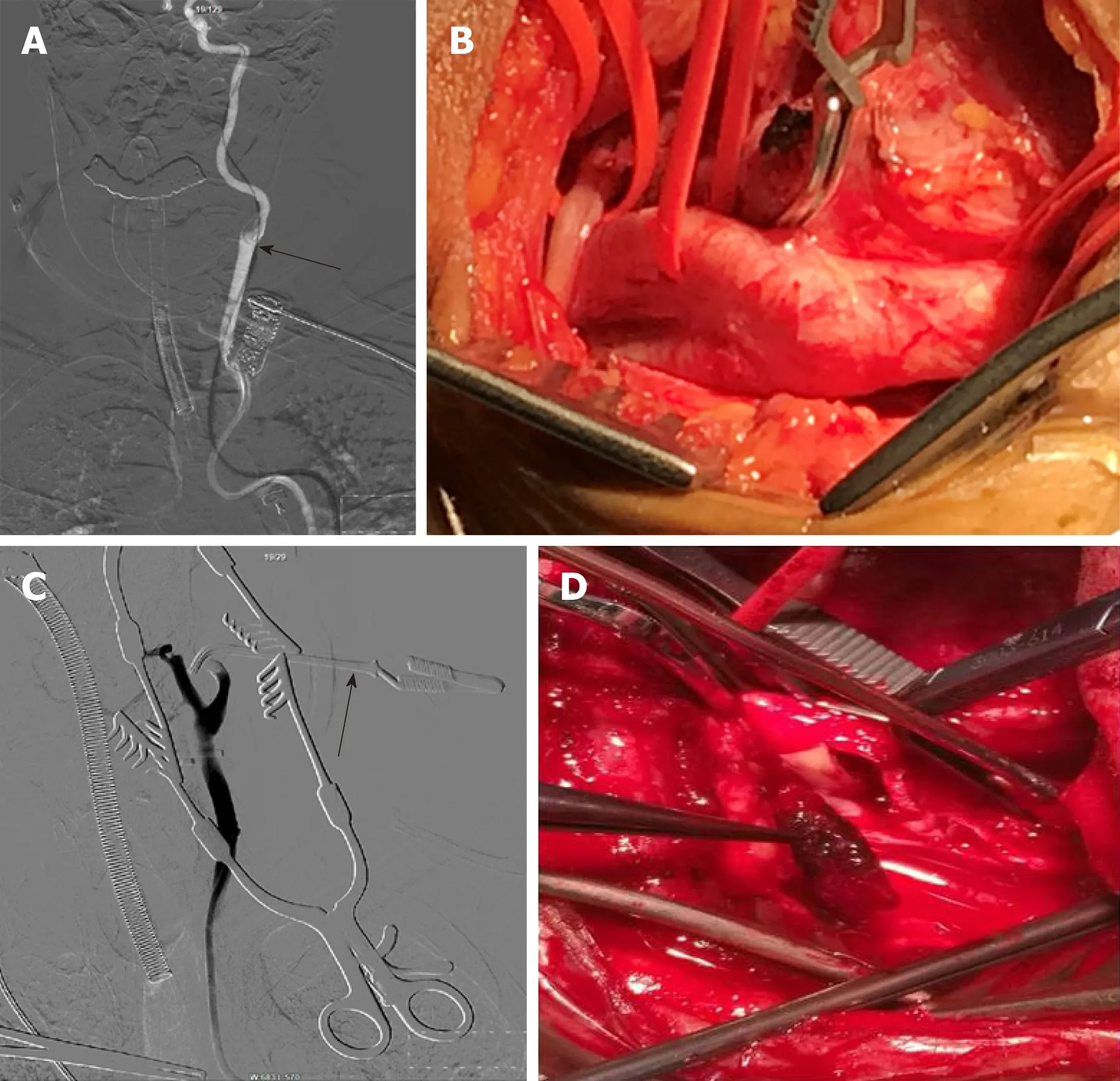
Figure 3 Imaging during surgery. A: An 8F guiding catheter was aspirated at the bifurcation of the left carotid artery, and no blood was observed; B: Percutaneous incision to expose the carotid artery, and the internal carotid blood flow was occluded; C: Partial recanalization of the external carotid artery was obtained by low-flow hand push angiography, but some clots remain unremoved; D: Carotid artery incision thrombectomy.
During the operation in the presented case, simple endovascular treatment was considered first. Repeated attempts were made to place the 8F guiding catheter into the left carotid artery, which took 40 min. The 8F catheter was used to aspirate the thrombus at the bifurcation. There was no obvious recanalization of blood after the aspiration, and it was believed that the catheter was stuck against the vessel wall or the thrombus blocked the tube. Then, the 8F catheter was withdrawn to the common carotid artery at the time of aspiration, and no reverse blood was found. The thrombus was considered to be large and stiff and obstructed the 8F catheter. If the 8F catheter is withdrawn from the body, it will take too long to replace the catheter and the thrombus may detach into the femoral artery sheath during retraction. So we chose to dissect and expose the carotid bifurcation. First, the internal carotid artery blood flow was blocked and partial recanalization of the external carotid artery was found by low-flow hand push angiography. However, some thrombus had still not been removed, so carotid artery incision thrombectomy was selected. The internal carotid artery was blocked during the process to avoid the distal escape of the embolus. The safety of emergency carotid endarterectomy (CEA) after intravenous thrombolysis has been confirmed by many reports, and the shortest time reported so far for CEA surgery after intravenous thrombolysis is 120 min[10,15,16].
CONCLUSION
Carotid artery incision thrombectomy combined with stenting for the treatment of carotid artery plus cerebral artery tandem embolization is clinically feasible. For patients with a complicated aortic arch and an extremely tortuous carotid artery who cannot receive simple endovascular treatment, carotid artery incision can be chosen to establish the interventional path. A large sample of cases is still needed for further study and confirmation.
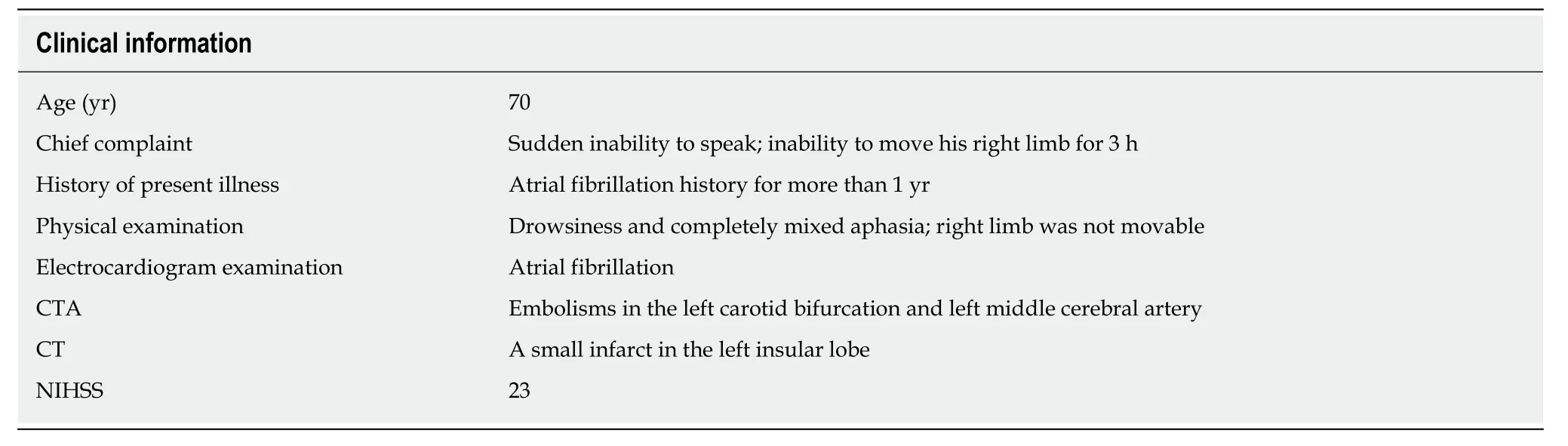
Table 1 Main characteristics of the patient
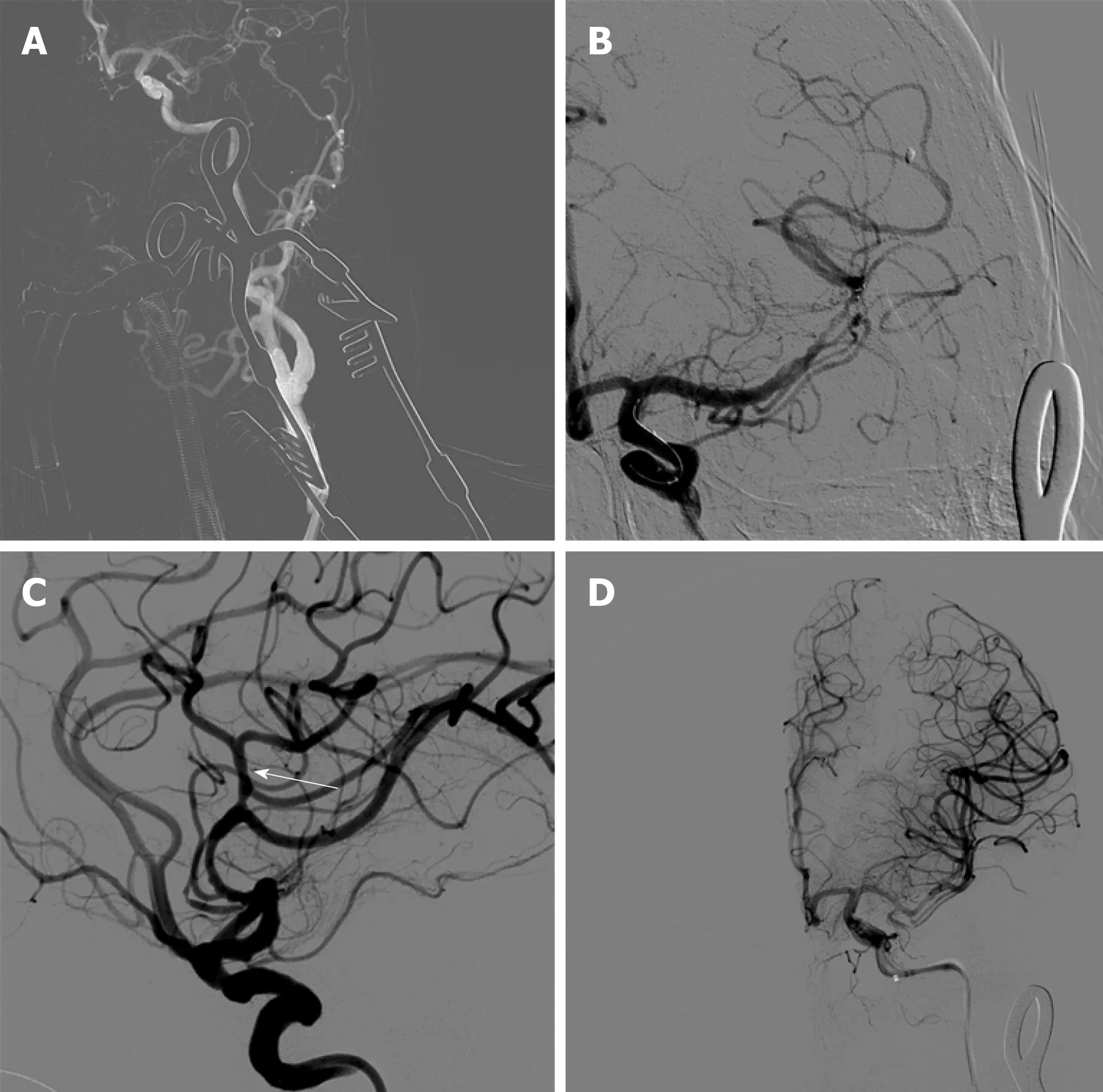
Figure 4 Middle cerebral artery blood flow recanalization modified thrombolysis in cerebral infarction level III. A: The upper trunk of the left middle cerebral artery is occluded, and the thrombus did not escape; B: Thrombectomy was performed with a Solitaire FR 6–30 mm stent; C: After thrombectomy, the blood flow was restored; D: Modified thrombolysis in cerebral infarction was stage III.
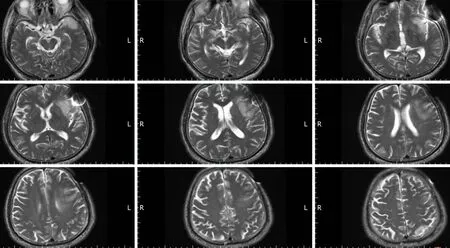
Figure 5 Brain magnetic resonance imaging shows small infarcts in the frontal and temporal lobes.
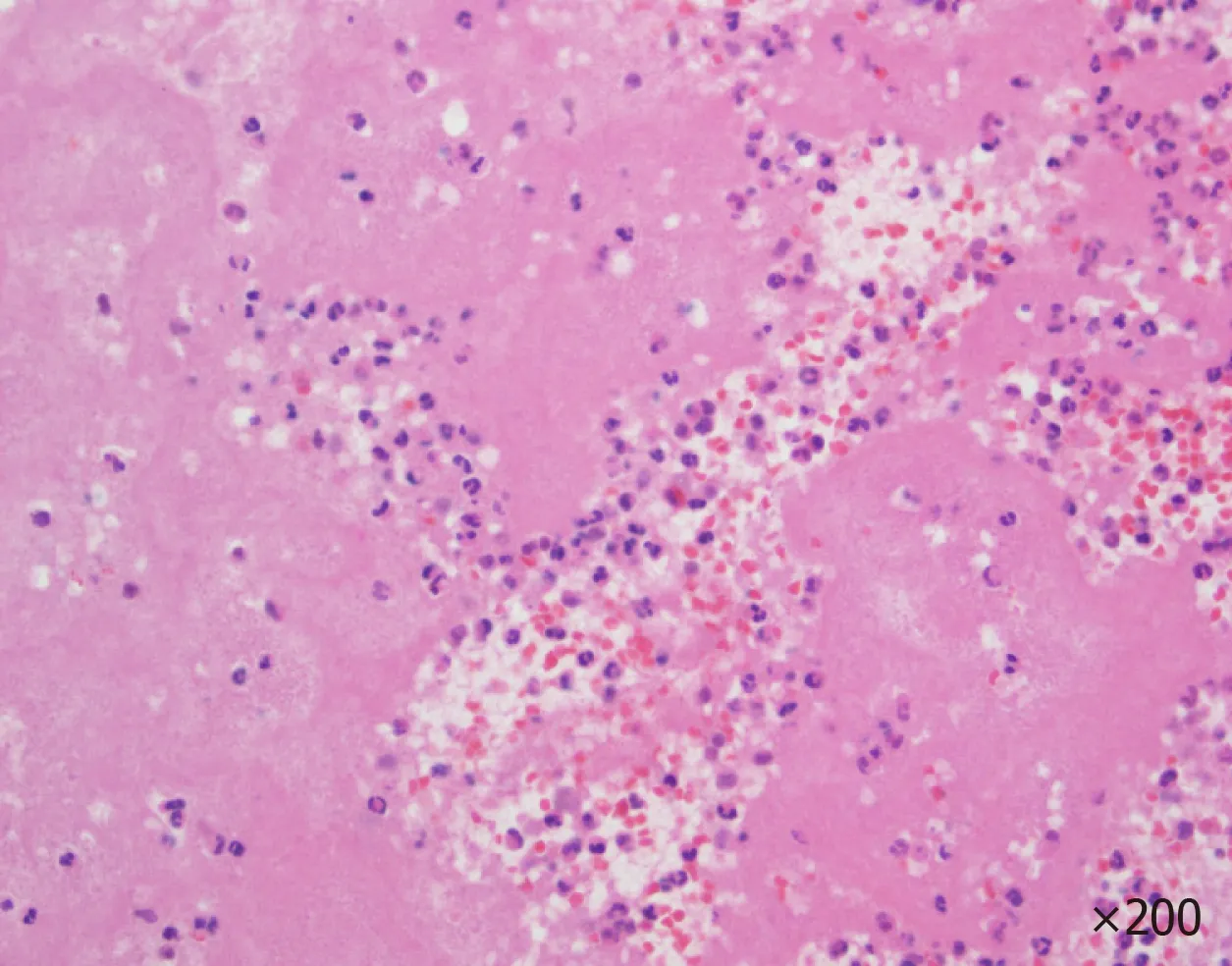
Figure 6 Pathological examination of the thrombus.
 World Journal of Clinical Cases2020年3期
World Journal of Clinical Cases2020年3期
- World Journal of Clinical Cases的其它文章
- Comprehensive review into the challenges of gastrointestinal tumors in the Gulf and Levant countries
- Can cyclin-dependent kinase 4/6 inhibitors convert inoperable breast cancer relapse to operability? A case report
- Ruptured splenic peliosis in a patient with no comorbidity: A case report
- Successful kidney transplantation from an expanded criteria donor with long-term extracorporeal membrane oxygenation treatment: A case report
- Boarding issue in a commercial flight for patients with cavitary pulmonary tuberculosis: A case report
- Cytomegalovirus ileo-pancolitis presenting as toxic megacolon in an immunocompetent patient: A case report
