Clinical characteristics and 28-d outcomes of bacterial infections in patients with hepatitis B virus-related acute-on-chronic liver failure
Chen Li,Hai-Bin Su,Xiao-Yan Liu,Jin-Hua Hu
Chen Li,Hai-Bin Su,Xiao-Yan Liu,Jin-Hua Hu,Liver Failure Treatment and Research Center,The Fifth Medical Center of Chinese PLA General Hospital,Beijing 100039,China
Abstract
BACKGROUND
Acute-on-chronic liver failure(ACLF),which includes hepatic and multiple extrahepatic organ failure,is a severe emergency condition that has high mortality.ACLF can rapidly progress and requires an urgent assessment of condition and referral for liver transplantation.Bacterial infections(BIs) trigger ACLF and play pivotal roles in the deterioration of clinical course.
AIM
To investigate the clinical characteristics and 28-d outcomes of first BIs either at admission or during hospitalization in patients with hepatitis B virus(HBV)-ACLF as defined by the Chinese Group on the Study of Severe Hepatitis B(COSSH).
METHODS
A total of 159 patients with HBV-ACLF and 40 patients with acute decompensation of HBV-related chronic liver disease combined with first BIs were selected for a retrospective analysis between October 2014 and March 2016.The characteristics of BIs,the 28-d transplant-free survival rates,and the independent predictors of the 28-d outcomes were evaluated.
RESULTS
A total of 194 episodes of BIs occurred in 159 patients with HBV-ACLF.Among the episodes,13.4% were community-acquired,46.4% were healthcare-associated,and 40.2% belonged to nosocomial BIs.Pneumonia(40.7%),spontaneous bacterial peritonitis(SBP)(34.5%),and bloodstream infection(BSI)(13.4%) were the most prevalent.As the ACLF grade increased,the incidence of SBP showed a downward trend(P = 0.021).Sixty-one strains of bacteria,including 83.6% Gramnegative bacteria and 29.5% multidrug-resistant organisms,were cultivated from 50 patients with ACLF.Escherichia coli(44.3%) and Klebsiella pneumoniae(23.0%)were the most common bacteria.As the ACLF grade increased,the 28-d transplant-free survival rates showed a downward trend(ACLF-1,55.7%;ACLF-2,29.3%;ACLF-3,5.4%;P < 0.001).The independent predictors of the 28-d outcomes of patients with HBV-ACLF were COSSH-ACLF score(hazard ratio[HR] = 1.371),acute kidney injury(HR = 2.187),BSI(HR = 2.339),prothrombin activity(HR = 0.967),and invasive catheterization(HR = 2.173).
CONCLUSION
For patients with HBV-ACLF combined with first BIs,pneumonia is the most common form,and the incidence of SBP decreases with increasing ACLF grade.COSSH-ACLF score,acute kidney injury,BSI,prothrombin activity,and invasive catheterization are the independent predictors of 28-d outcomes.
Key words:Hepatitis B virus;Acute-on-chronic liver failure;Bacterial infections;Outcomes;Chronic liver disease;Spontaneous bacterial peritonitis
INTRODUCTION
Acute-on-chronic liver failure(ACLF) is a common syndrome that occurs in combination with organ failure and has high mortality rate[1].Although the definitions of ACLF differ between Eastern and Western countries,in the simplest terms,ACLF is an acute deterioration in patients with chronic liver disease(CLD)(usually cirrhosis)and has high short-term mortality[2-4].Alcoholic liver disease is the major etiology in patients with ACLF from Europe and North America,but hepatitis B virus(HBV) is the major etiology in Asia-Pacific and Africa.Based on the European Association for the Study of the Liver definition of ACLF,the Chinese Group on the Study of Severe Hepatitis B(COSSH) has recently developed new criteria for HBV-ACLF and established a relevant prognostic score based on the characteristics of Chinese patients with HBV-CLD.In patients with chronic hepatitis B,total bilirubin(TBIL) ≥ 12 mg/dL and international normalized ratio(INR) ≥ 1.5 are included in the new criteria for HBV-ACLF.The COSSH-ACLF criteria bridge a gap in the European Association for the Study of the Liver-ACLF definition for HBV-ACLF diagnosis.The new criteria increased the number of patients diagnosed with HBV-related ACLF by 20%,thereby increasing their opportunity to receive intensive management[5].
Bacterial infections(BIs) play pivotal roles in the development and progression of ACLF[6,7].BIs mainly trigger the occurrence of ACLF in patients with cirrhosis.About 32.6% of patients with ACLF are triggered by BIs in the Chronic Liver Failure Consortium ACLF in Cirrhosis study[8].The 30-d survival rates of patients with BIs triggered ACLF(71.6%) were distinct from those with non-BIs triggered ACLF(33.8%);moreover,BIs triggered ACLF was independently associated with 30- and 90-d mortality[6].
The study of COSSH show that patients with HBV-CLD combined with BIs are prone to ACLF[5].However,the clinical characteristics,survival rates,and prognostic effects of BIs in the COSSH definition for patients with HBV-ACLF are unclear.Patients with COSSH-HBV-ACLF combined with first BIs were selected for thisretrospective study.This study aimed to evaluate the clinical characteristics of BIs,infection sites,etiology,and 28-d outcomes of patients.To avoid some confounding factors,we did not include patients in the intensive care unit(ICU).
MATERIALS AND METHODS
Patient enrollment and study design
Patients with HBV-ACLF and acute decompensation(AD) of HBV-related CLD combined with first BIs who were hospitalized at the Fifth Medical Center of Chinese PLA General Hospital of China from October 2014 to March 2016 were selected from the electronic database for retrospective analysis.Patients with diseases resulting in bilirubin elevation,such as hemolytic,congenital non-hemolytic,and obstructive jaundice,malignant tumor,and extrahepatic diseases that seriously influence life were excluded.Patients with hospital length of stay < 3 d or incomplete laboratory results,patients in ICU,and pregnant women were also excluded from the electronic database.All patients with HBV-ACLF received antiviral therapy with nucleoside analogues after admission.Those patients were assessed for nutritional status by nutritionist after hospitalization.The target of energy intake for those patients was 30-35 kcal/kg·d.
The inclusion criteria were as follows: Presence of CLD,AD manifestation,and first BIs either at admission or during hospitalization.The exclusion criteria were as follows: Viral infections other than HBV and hepatic lesions because of other factors,such as alcoholic hepatitis,autoimmune liver diseases,drug-induced liver injury,Wilson's Disease,hemochromatosis,and schistosomiasis.
A total of 408 patients satisfied the inclusion criteria,and 209 patients were excluded based on the exclusion criteria.Finally,199 patients were selected.According to the definition of COSSH-HBV-ACLF,159 patients were diagnosed with HBV-ACLF and 40 patients were diagnosed with AD-HBV-CLD.Eighty cases were ACLF grade 1(ACLF-1),42 cases were ACLF grade 2(ACLF-2),and 37 cases were ACLF grade 3(ACLF-3).The patients were followed 28 d after their first BIs.We considered death as the primary endpoint.Information on prognosis was verified through medical records and telephone contact.Two patients(one case with ACLF-1 and one case with ACLF-2) with HBV-ACLF received orthotopic liver transplantation during the follow-up period(Figure 1).
Definitions
Based on the COSSH-HBV-ACLF criteria,patients with HBV-CLD were divided into an HBV-ACLF(abbreviated as ACLF) group and an AD of HBV-CLD(abbreviated as AD) group.According to the degree and number of organ failures,ACLF was divided into ACLF-1,ACLF-2,and ACLF-3.The severity of ACLF was assessed using COSSHACLF scores.COSSH-ACLF scores were calculated using the formula 0.741 × INR +0.523 × HBV-SOFA + 0.026 × age + 0.003 × TBIL.HBV-SOFA was assessed based on the severity of kidney injury,hepatic encephalopathy(HE),circulation,and respiratory function by COSSH-ACLF criteria[5].
Complications of ACLF were diagnosed based on the following criteria.HE was defined based on the West Haven criteria[9].Acute variceal bleed was diagnosed based on the Baveno V endoscopic criteria[10].Acute kidney injury(AKI) was defined using the criteria of revised consensus recommendations of the International Club of Ascites[11].
First BIs were referred to as the first BIs that occurred either at admission or during hospitalization in patients.BIs were diagnosed based on the following criteria.Spontaneous bacterial peritonitis(SBP) was diagnosed based on polymorphonuclear cell count in ascitic fluid ≥ 250/mm3with/without a positive fluid culture[12].Pneumonia was diagnosed based on the presence of radiological evidence of consolidation with at least two of the following criteria: Fever higher than 38 °C or hypothermia less than 35 °C;dyspnea;cough;purulent sputum;pleuritic chest pain;and white blood cells > 1000/mm3or < 4000/mm3[13].Bloodstream infection(BSI) was diagnosed based on the growth of a non-common skin contaminant from ≥ 1 blood culture(BC) and of a common skin contaminant from ≥ 2 BCs drawn on separate sites with signs of infection[14].Spontaneous bacterial empyema(SBE) was diagnosed based on polymorphonuclear cell count in pleural fluid ≥ 250/mm3[15].Urinary tract infection(UTI) was diagnosed based on urine white blood cells count > 10/high-power field with a positive urine Gram stain or urine culture or uncountable leucocytes per field if negative cultures[16].Cellulitis was diagnosed based on the clinical signs of infection of the skin associated with discomfort,erythema,swelling,and warmth of the affected area[17].Unproven BIs were diagnosed based on the presence of fever and leucocytosisthat requires antibiotic therapy without any identifiable source[15].In the present study,we defined spontaneous bacterial empyema,UTI,cellulitis,and unproven BIs as other BIs.

Figure 1 Outline of the screening and case selection protocol.
Systemic inflammation response syndrome(SIRS) was assessed according to the recommendations of the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference[18].The definitions of community-acquired(CA),healthcare-associated(HCA),and nosocomial infections were based on the time of acquisition[19,20].Multidrug-resistant organisms(MDROs) was defined as acquired non-susceptibility to at least one agent in three or more antimicrobial categories[21].
Statistical analysis
Categorical variables are expressed as number(%),and continuous variables are described as the mean ± SD or median(inter-quartile range,Q1-Q3).Continuous variables were compared by Student'sttest.Mann-WhitneyUtest was used to compare the parameters under nonnormal distribution.Categorical data were compared byχ2or Fisher's exact test.Trend test of categorical data was carried out using linear-by-linear association approach.Cumulative survival probability curves were calculated by Kaplan-Meier method and compared by log-rank test.Univariate COX proportional hazard regression analysis was first used to screen candidate factors.Candidate variables(P< 0.05) were used as input into a multivariate COX proportional hazard regression analysis following a forward stepwise approach(P-in:0.05 andP-out: 0.01).All statistical analyses were conducted using SPSS 19.0 software(IBM,Armonk,NY).For all analyses,P< 0.05 was considered statistically significant.
RESULTS
Baseline clinical characteristics in ACLF and AD groups
This study involved 199 patients,including 159 patients with HBV-ACLF and 40 patients with AD-HBV-CLD,with an average age of 48.0 ± 10.9 years.About 85.4% of the patients were male,and 86.4% had cirrhosis.At the time of BIs,96.5% had ascites,47.7% had AKI,53.3% had HE,19.6% had acute variceal bleeding,45.2% had SIRS,and 19.1% had invasive catheterization.Moreover,18.1% of the patients developed multiple-site BIs.
TBIL,direct bilirubin,alanine aminotransferase,aspartate amino transferase,creatinine,INR,AKI ratio,HE ratio,and COSSH-ACLF scores in the ACLF group were higher than those in the AD group(P< 0.05)(Table 1).The prothrombin activity(PTA) in the ACLF group was lower than that in the AD group(P< 0.05)(Table 1).No differences in the other clinical indicators were observed between the two groups(P>0.05)(Table 1).
Characteristics of all the 241 episodes of BIs in the ACLF and AD groups
A total of 194 episodes of BIs occurred in 159 patients with HBV-ACLF,of which 13.4% belonged to CA BIs,46.4% belonged to HCA BIs,and 40.2% belonged to nosocomial BIs.Forty-seven episodes of BIs occurred in 40 patients with AD of HBVCLD,of which 19.1% belonged to CA BIs,57.4% belonged to HCA Bis,and 23.4%belonged to nosocomial BIs.The percentage of nosocomial BIs in the ACLF group was higher than that in the AD group(P= 0.032)(Table 2).Pneumonia,SBP,and BSI were the most common forms of BIs in the ACLF and AD groups.Pneumonia was the most common form in the ACLF group,and SBP was the most common form in the AD group(Table 2).
Relationship between the site of BIs and grade of ACLF
SBP was the most common form of BI in the AD and ACLF-1 groups.Pneumonia was the most common form of BIs in the ACLF-2 and ACLF-3 groups(Table 3).The trend test displayed that as the ACLF grade increased,the incidence of SBP showed a downward trend(trend value = 5.291,P= 0.021).No significant changes were observed in pneumonia(trend value = 2.357,P= 0.125),BSI(trend value = 0.605,P=0.437),or other BIs(trend value = 0.083,P= 0.774).
Bacterial detection in patients
Fourteen strains of bacteria were cultivated from 13 cases in the AD group,in which 28.6% belonged to CA,21.4% belonged to HCA,and 50.0% belonged to nosocomial BIs.Twelve strains of bacteria(85.7%) were Gram negative,including eight strains of
Escherichia coli(E.coli),three strains ofKlebsiella pneumoniae(K.pneumoniae),and one strain ofEnterobacter aerogenes.Two strains of Gram-positive bacteria were detected,including one strain ofStaphylococcus aureus(S.aureus) and one strain ofStaphylococcus epidermidis(S.epidermidis).Sixty-one strains of bacteria were cultivated from 50 cases in the ACLF group,in which 16.4% belonged to CA,44.3% belonged to HCA,and 39.3% belonged to nosocomial BIs.Fifty-one strains of bacteria(83.6%)were Gram negative,including 27 strains ofE.coli,14 strains ofK.pneumoniae,four strains ofPseudomonas aeruginosa,two strains ofAcinetobacter baumannii,one strain ofEnterobacter cloacae,one strain ofAeromonas hydrophila,one strain ofAeromonas guinea,and one strain ofStenotrophomonas maltophilia.Ten strains of Gram-positive bacteria were observed,including five strains ofEnterococcus faecium,two strains ofS.epidermidis,two strains ofS.aureus,and one strain ofStreptococcus oralis.E.coliandK.pneumoniaewere the most common bacteria in the AD and ACLF groups.No significant difference in the proportion of Gram-negative or -positive bacteria was found between the two groups(P> 0.05).In the ACLF group,the most common cultivated bacteria for SBP,BSI,and other BIs wereE.coli,butK.pneumoniaewas the most common cultivated bacterium for pneumonia(Table 4).
In the AD group,five strains of bacteria(35.7%) were MDROs,including four strains ofE.coliand one strain ofS.aureus.In the ACLF group,18 strains of bacteria(29.5%) were MDROs,including ten strains of Gram-negative bacteria(four strains ofE.coli,two strains ofK.pneumoniae,two strains ofAcinetobacter baumannii,one strain ofEnterobacter cloacae,and one strain ofPseudomonas aeruginosa) and eight strains of Gram-positive bacteria(five strains ofEnterococcus faecium,two strains ofS.aureus,and one strain ofS.epidermidis).In the ACLF group,the MDRO rate of cultivated Gram-positive bacteria(80.0%) was higher than that of cultivated Gram-negative bacteria(19.6%)(χ2= 11.900,P= 0.001),and the proportion of multidrug-resistant Gram-positive organisms in BSI(83.3%) was higher than that of multidrug-resistant Gram-negative organisms(15.0%)(χ2= 7.164,P= 0.007)(Table 4).
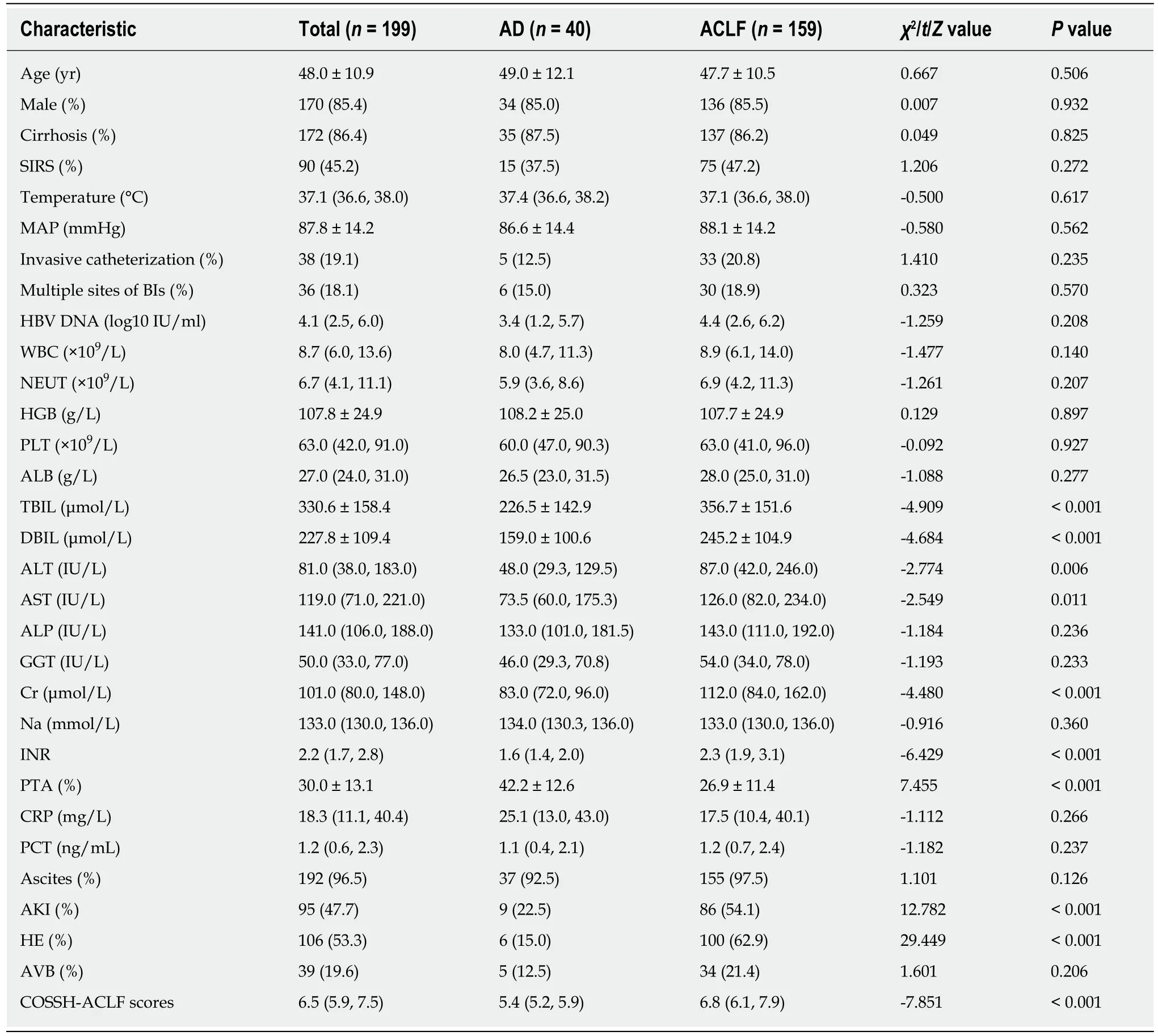
Table 1 Baseline characteristics and laboratory results of the overall study collective
28-d outcomes of patients
Using the Kaplan-Meier method,the 28-d transplant-free survival rate in the ACLF group(36.9%) was significantly lower than that in the AD group(85.0%)(χ2= 25.488,P< 0.001)(Figure 2A).Generally,differences were observed in the 28-d transplantfree survival rates in the ACLF-1,ACLF-2,and ACLF-3 groups(χ2= 47.422,P< 0.001)(Figure 2B).The 28-d transplant-free survival rate(55.7%) of ACLF-1 was higher than those of ACLF-2(29.3%)(χ2= 7.824,P= 0.005) and ACLF-3(5.4%)(χ2= 44.330,P<0.001).The 28-d transplant-free survival rate of ACLF-2 was higher than that of ACLF-3(χ2= 13.398,P< 0.001)(Figure 2B).As the ACLF grade increased,the 28-d transplant-free survival rates decreased(trend value = 28.557,P< 0.001).
Independent predictors of the 28-d outcomes of the ACLF group
According to the 28-d outcomes,patients with HBV-ACLF were divided into the survivor and non-survivor groups,and two patients who underwent orthotopic liver transplantation were excluded.Univariate Cox regression was conducted on the baseline indices of the cohort.Categorical variables were differentiated and assigned with values based on their sign,and continuous variables were assigned with values according to actual numerical values.Age,SIRS,invasive catheterization,grade ofACLF,WBC,neutrophil count,alanine aminotransferase,aspartate amino transferase,creatinine,INR,PTA,procalcitonin,AKI,HE,pneumonia,SBP,BSI,multiple sites of BIs,and COSSH-ACLF scores were screened out as meaningful variables and used as inputs for multivariate Cox regression(P< 0.05)(Table 5).Multivariate Cox regression showed that COSSH-ACLF scores(hazard ratio [HR] = 1.371),AKI(HR =2.187),BSI(HR = 2.339),PTA(HR = 0.967),and invasive catheterization(HR = 2.173)were the independent predictors of 28-d outcomes of the patients(P< 0.05)(Table 5).
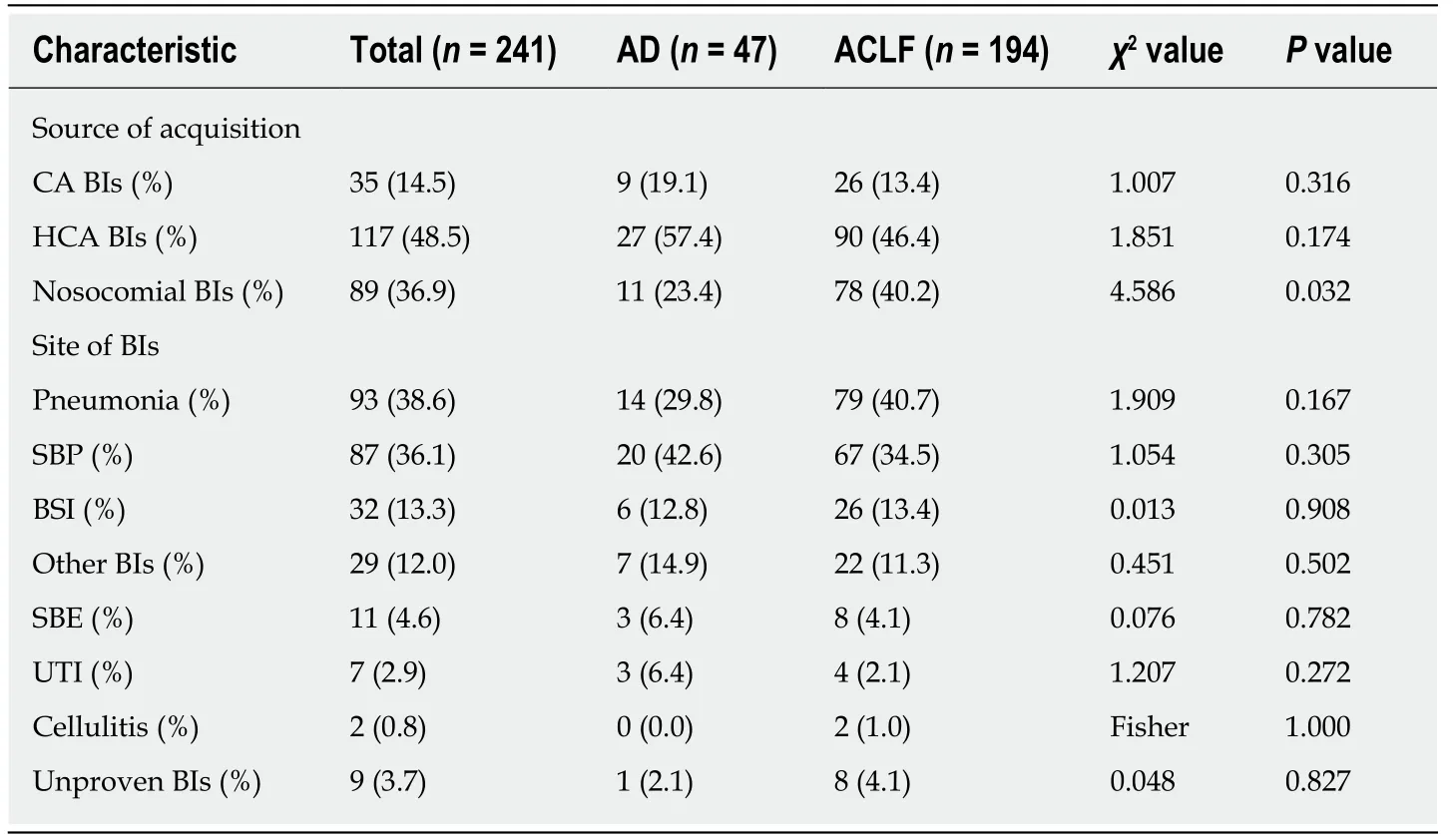
Table 2 Characteristics of all the 241 episodes of bacterial infections in the overall studycollective
DISCUSSION
This study is unique,because it assessed the clinical characteristics,bacterial identification,and outcomes in patients with HBV-ACLF(as defined by COSSH)combined with first BIs in China.The first main finding of our study is that the majority of BIs belong to HCA and nosocomial BIs.Pneumonia,not SBP,was the most common form of BI for patients with HBV-ACLF.Second,E.coliandK.pneumoniaewere the most common cultured bacteria,and the proportion of MDROs was 29.5%.Third,some important clinical indicators,including the COSSH-ACLF scores,can serve as independent predictors of the 28-d outcomes for those patients.
For patients with HBV-ACLF combined with BIs,CA BIs accounted for 13.4%,HCA BIs accounted for 46.4%,and nosocomial BIs accounted for 40.2%.HCA and nosocomial BIs constituted the main types of BIs in those patients,and the results were similar to those of previous studies in Eastern countries[22,23].However,in Western countries,CA BIs account for 25.0%-52.1%[6,7,24],which is significantly higher than the proportion in Eastern countries(15.7%-18.7%)[22,23]and in our study(13.4%).The large number of HCA and nosocomial BIs observed in ACLF patients may be attributed to the use of invasive procedures and ICU admissions in patients before they are transferred to a tertiary referral hospital in China[22].Hence,patients with ACLF,who have been treated in a hospital over the past 180 d,should be screened for BIs after admission.
In our study,pneumonia(40.7%),SBP(34.5%),and BSI(13.4%) were the three most common forms of first BIs in patients with HBV-ACLF.Our findings are consistent with some studies in China and India in which pneumonia(45.0%-49.4%) is the most common form of BI[22,23,25],but studies in Western countries show that SBP(25.0%-32.4%) is the most common form of BI in patients with ACLF[6,8,24].Moreover,pneumonia is the most common form in patients with ACLF-2 and ACLF-3,and SBP is most common form in patients with AD and ACLF-1.As the ACLF grade increased,the incidence of SBP decreased.A correlation was observed between the occurrence of pneumonia and the severity of ACLF.Patients with end-stage liver disease combined with pneumonia had higher mortality than other infections[12],and poor air quality isrelated to the high prevalence of pneumonia[26],which may be related to this phenomenon in China.Another interesting phenomenon is that the proportion of urinary tract infection(2.1%) in our study was significantly lower than that in previous studies(>10%)[7,25].The likely reason is that patients in the present study were recruited from non-ICU and in a single hospital,and the rate of urinary catheter placement should be lower than that of patients from ICU.

Table 3 Relationship between site of bacterial infections and grade of acute-on-chronic liver failure
Similar to previous research,the present study showed that Gram-negative bacteria(83.6%) comprised the majority of cultured bacteria,andK.pneumoniae(44.3%) andE.coli(23.0%) were the most common.However,the proportion of Gram-positive bacteria in cultured bacteria was low(16.4%),and the MDRO rate was 80.0%.Previous studies reported that more than half of the cultured bacteria were Gram positive[6,22].This finding is inconsistent with our present study possibly because the subjects selected were non-ICU patients and that the bacterial spectrum differs in each region.Moreover,Gram-positive bacteria have a higher rate of MDROs,and the empirical treatment of antibiotics should be adjusted in time according to the results of bacterial susceptibility testing.
Similar to previous studies[24,25],the prevalence of MDRO strains(29.5%) was high in patients with ACLF in the present study.This condition might be related to the large numbers of diagnosed HCA(44.3%) and nosocomial BIs(39.3%).HCA and nosocomial BIs are caused more frequently by antibiotic-resistant bacteria and associated with worse clinical outcome than CA BIs[27].Selective intestinal decontamination with non-absorbable antibiotics is often used to prevent the occurrence of SBP and HE in patients with ACLF,but it could also promote the development of MDROs[28].
We observed significantly higher mortality rate and shorter probability of survival in patients with ACLF combined with BIs than in patients with ACLF without BIs through comparison with previous studies[7,22,29].As the ACLF grade increased,the 28-d transplant-free survival rates decreased.Hence,BIs exert a major effect on the prognosis of patients with ACLF.This finding is supported by the finding of previous studies that BIs are an independent predictor of mortality in patients with ACLF.BIs can aggravate the extent of liver failure,and multiple extra-hepatic organ failures can also occur in the presence of organ damage from exaggerated inflammation[30].In comparison with patients with cirrhosis,monocytes from patients with ACLF featured elevated frequencies of interleukin-10 producing cells,reduced human leucocyte antigen DR isotype expression,and impaired phagocytic and oxidative burst capacity[31].Therefore,the 28-d transplant-free survival rate of patients with AD combined with BIs was significantly higher than that of patients with ACLF combined with BIs.
In this study,we identified five independent factors that can predict the 28-d outcomes of patients with HBV-ACLF combined with BIs.Regardless of the presence of BIs in patients with ACLF,PTA and AKI are important risk factors for prognosis[32,33].The COSSH-ACLF scores for severity and short-term mortality of patients with HBV-ACLF were superior or comparable with other scores obtained in previous studies[5,34].In our study,the COSSH-ACLF score has also been shown to be a very important prognostic factor for patients with HBV-ACLF combined with BIs.Notably,BSI and invasive catheterization were independent predictors of the 28-d outcomes of patients with HBV-ACLF combined with BIs.MDROs accounted for 31%of BSI in cirrhotic patients(30.8% in our study),and its occurrence was found to be related to previous antimicrobial exposure and invasive procedures.This condition often results in delayed or inadequate empirical antimicrobial therapy and increased mortality rates[35].Continuous/extended infusion beta-lactams or carbapenems,as adequate empiric treatment in cirrhotic patients with BSI,may deal with MDROs and improve the outcomes compared with intermittent bolus infusion[36].We believe that the unreasonable and prolonged placement of invasive catheters may increase theincidence of HCA and nosocomial BIs and MDROs,which may affect the outcomes of patients with ACLF[35,37].Hence,disinfection and care of invasive catheters should be beneficial to these patients.

Table 4 Bacterial identification and detection of multidrug-resistant organisms in patients with acute-on-chronic liver failure
Our study has some limitations.First,the history of the use of steroids,antibiotics,and proton pump inhibitors and the phenomenon of HBV reactivation of patients before BIs were unclear in our electronic database.Such information may be related to the clinical manifestations and prognosis of patients.Second,considering the first BIs of the patients,fungal infections and second BIs were not evaluated in the present cohort,which may have a certain impact on the true prognosis.Third,BIs can be as acute insult in triggering ACLF.But this was a retrospective study and many patients were transferred from other lower-level hospitals,so the direct contribution of BIs was unclear.Fourth,because some patients were transferred to other hospitals during treatment,the specific cause of death was not completely clear.Fifth,this single-center retrospective study had a small sample size.Hence,additional prospective randomized studies should be conducted in the future.
In conclusion,HCA and nosocomial BIs are the most common types for patients with HBV-ACLF combined with BIs.Pneumonia is the most common form of BI in patients with ACLF-2 and ACLF-3,and SBP is the most common form of BI in patients with AD and ACLF-1.Gram-negative bacteria account for the majority of cultured bacteria,and MDROs are common.The 28-d transplant-free survival rate of patients is very low and decreases with increasing ACLF grade.The independent predictors of the 28-d outcomes of these patients are COSSH-ACLF scores,AKI,BSI,PTA,and invasive catheterization.
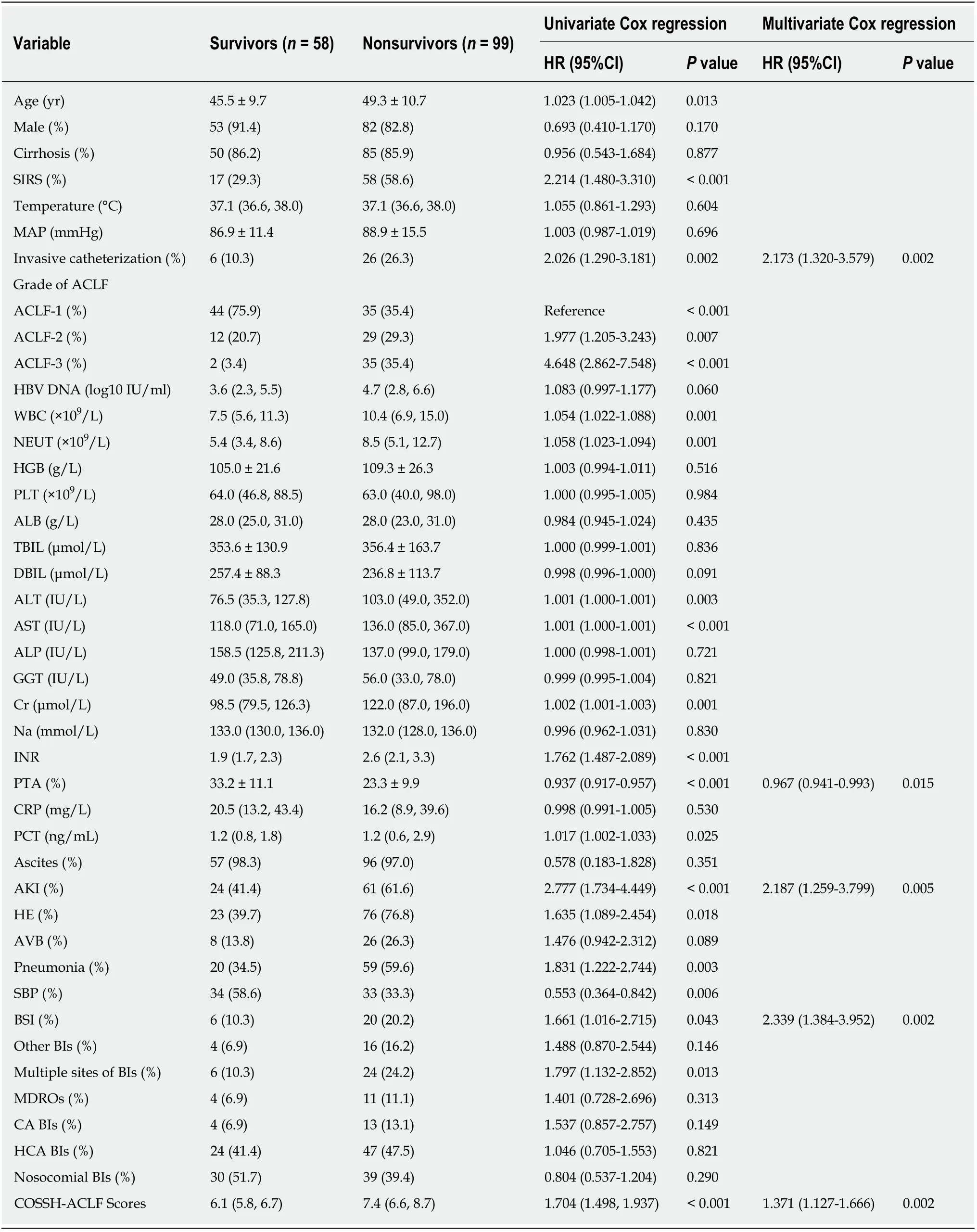
Table 5 lndependent predictors of 28-d outcomes in hepatitis B virus-related acute-on-chronic liver failure patients combined with bacterial infections
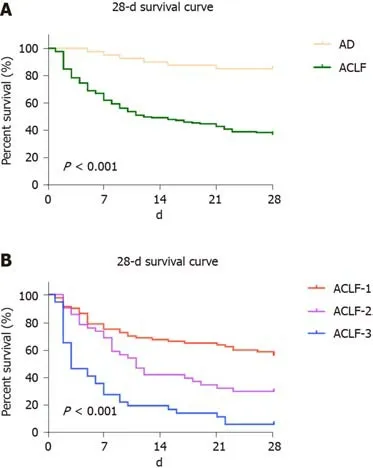
Figure 2 Comparison of the 28-d transplant-free survival rates in each group.
ARTICLE HIGHLIGHTS
Research background
Hepatitis B virus(HBV) related acute-on-chronic liver failure(ACLF) is a complicated syndrome with a high short-term mortality rate that develops in patients with HBV related chronic liver disease(CLD) regardless of the presence of cirrhosis and is characterized by acute deterioration of liver function and hepatic and/or extrahepatic organ failure.Bacterial infections(BIs) trigger ACLF and play pivotal roles in the deterioration of clinical course.
Research motivation
The Chinese Group on the Study of Severe Hepatitis B(COSSH) has recently developed a new criterion for HBV-ACLF.However,the clinical characteristics,survival rates,and prognostic effects of BIs in the COSSH definition for patients with HBV-ACLF are unclear.Patients with COSSH-HBV-ACLF combined with first BIs were selected for this study.
Research objectives
This study aimed to investigate the clinical characteristics,the site of BIs,bacterial detection,28-d outcomes,and independent predictors of outcomes of first BIs either at admission or during hospitalization in patients with HBV-ACLF as defined by the COSSH.
Research methods
A total of 159 patients with HBV-ACLF and 40 patients with acute decompensation of HBV-CLD combined with first BIs were selected for a retrospective analysis between October 2014 and March 2016.The characteristics of BIs,the site of BIs,and bacterial detection were evaluated.Cumulative survival probability curves of the 28-d transplant-free survival rates were calculated by Kaplan-Meier method and compared by log-rank test.COX proportional hazard regression analysis was used to screen the independent predictors of 28-d outcomes.
Research results
A total of 194 episodes of BIs occurred in 159 patients with HBV-ACLF.Among the episodes,13.4% were community-acquired,46.4% were healthcare-associated,and 40.2% belonged to nosocomial BIs.Pneumonia(40.7%),spontaneous bacterial peritonitis(SBP)(34.5%),and bloodstream infection(BSI)(13.4%) were the most prevalent.As the ACLF grade increased,the incidence of SBP showed a downward trend(P= 0.021).Sixty-one strains of bacteria,including 83.6% of Gram-negative bacteria and 29.5% of multidrug-resistant organisms(MDROs),were cultivated from 50 patients with ACLF.E.coli(44.3%) andK.pneumoniae(23.0%) were the most common bacteria.As the ACLF grade increased,the 28-d transplant-free survival rates showed a downward trend(ACLF-1,55.7%;ACLF-2,29.3%;ACLF-3,5.4%;P< 0.001).The independent predictors of the 28-d outcomes of patients with HBV-ACLF were COSSH-ACLF score(hazardratio [HR] = 1.371),acute kidney injury(AKI)(HR = 2.187),BSI(HR = 2.339),prothrombin activity(PTA)(HR = 0.967),and invasive catheterization(HR = 2.173).
Research conclusions
For patients with COSSH-HBV-ACLF combined with first BIs,pneumonia is the most common,and the incidence of SBP decreases with increasing ACLF grade.Gram-negative bacteria account for the majority of cultured bacteria,and MDROs are common.The 28-d transplant-free survival rate of patients is very low and decreases with increasing ACLF grade.The independent predictors of the 28-d outcomes are COSSH-ACLF score,AKI,BSI,PTA,and invasive catheterization.
Research perspectives
The clinical characteristics,the site of BIs,bacterial detection,28-d outcomes and independent predictors of outcomes of first BIs in patients with COSSH-HBV-ACLF were described in detail in this study.However,this single-center retrospective study had a small sample size.Hence,additional multi-center prospective randomized study studies should be conducted to reveal the role of BIs in the deterioration of clinical course in patients with COSSH-HBV-ACLF in the future.
ACKNOWLEDGEMENTS
The authors would like to thank Dr.Xiang Xu,Dr.Yu-Hui Peng,Dr.Li-Long Yan,and Dr.Hui Li from Liver Failure Treatment and Research Center,The Fifth Medical Center of Chinese PLA General Hospital for their help in collecting the data of patients and Dr.Jing-Feng Bi from Department of Epidemiology and Public Health,The Fifth Medical Center of Chinese PLA General Hospital for his help with statistical analysis.
 World Journal of Clinical Cases2020年5期
World Journal of Clinical Cases2020年5期
- World Journal of Clinical Cases的其它文章
- Gut microbiota and nutrient interactions with skin in psoriasis: A comprehensive review of animal and human studies
- Microbiota-gut-brain axis and its affect inflammatory bowel disease:Pathophysiological concepts and insights for clinicians
- Distal esophageal spasm: Update on diagnosis and management in the era of high-resolution manometry
- Clinical course of percutaneous cholecystostomies: A crosssectional study
- Application of hybrid operating rooms for treating spinal dural arteriovenous fistula
- Ruxolitinib add-on in corticosteroid-refractory graft-vs-host disease after allogeneic stem cell transplantation: Results from a retrospective study on 38 Chinese patients
