Delayed right coronary ostial obstruction after J-valve deployment in transcatheter aortic valve implantation:A case report
Zhao Xu,Hong Yu,Peng Liang
Zhao Xu,Hong Yu,Peng Liang,Department of Anesthesiology,West China Hospital,Sichuan University and The Research Units of West China(2018RU012),Chinese Academy of Medical Sciences,Chengdu 610041,Sichuan Province,China
Abstract
Key words:Transcatheter aortic valve implantation;Right coronary artery;Obstruction;Complication;Management;Case report
INTRODUCTION
Aortic stenosis(AS)is the most common valve disease in adults in China.However,most patients with valve diseases over 50-years-old in China did not receive standard treatment according to the 2014 report from the cardiopulmonary bypass(CPB)Board of the Chinese Medical Association.Surgical aortic valve replacement has been the standard approach,with an overall 2.5%-4% mortality[1].However,transcatheter aortic valve implantation(TAVI)is being increasingly used for the treatment of symptomatic AS.
Recently,an increasing number of intermediate- to low-risk patients have been treated with TAVI[2,3].Along with its application,several complications have been encountered such as pericardial bleeding,paravalvular leakage,conduction abnormalities,and coronary artery obstruction.Coronary artery obstruction is the most severe complication.Here,we describe an uncommon complication of delayed right coronary obstruction in a low-risk transapical TAVI case.
CASE PRESENTATION
Chief complaints
A 73-year-old woman presented to the Department of Cardiovascular Surgery of our hospital complaining of palpitation and precordial discomfort.
History of present illness
The patient’s symptoms started 5 mo ago with recurrent episodes of palpitation and precordial discomfort,which had been worsened by exertion.The patient experienced occasional chest pain and syncope without dizziness,nausea,and vomiting.
History of past illness
The patient was diagnosed with hypertension 10 years ago.The blood pressure was controlled with reserpine.
Personal and family history
The patient had a disease-free personal and family history.
Physical examination upon admission
The patient’s temperature was 36.7 °C,heart rate was 90 bpm,respiratory rate was 20 breaths per min,and blood pressure was 145/87 mmHg.The heart border expanded to the left.Systolic ejection murmur could be auscultated over the aortic and pulmonary areas.Our clinical consideration was AS.
Laboratory examinations
Arterial blood gas analysis revealed a mild decrease of oxygen partial pressure(78 mmHg)on room air with normal hematocrit and hemoglobin count.Prothrombin,partial thromboplastin times,and d-dimers were normal.The blood biochemistries,as well as urine analysis were normal.Electrocardiogram showed a sinus rhythm with complete left bundle branch block.Chest X-ray was also normal.
Imaging examinations
Coronary artery disease was excluded before the procedure by angiography.Transthoracic echocardiography and intraoperative transesophageal echocardiography(TEE)confirmed severe aortic valve calcification and stenosis causing left ventricular concentric hypertrophy with an ejection fraction of 66%.
FINAL DIAGNOSIS
The final diagnosis of the presented case was severe AS with sinus rhythm and New York Heart Association functional class grade III.
TREATMENT
The preoperative evaluation of the patient revealed a logistic EuroSCORE II of 1.21%.Transapical TAVI was scheduled.After routine monitoring in the hybrid operating room,anesthesia was induced.Then TEE was used to guide the transapical approach.Under the guidance of digital subtraction angiography,aortic valve balloon expansion was performed by a temporary pacemaker at 160 beats per min.TEE after balloon expansion showed a 21.5 mm aortic valve annulus(Video 1).A 23 mm J-valve,a second-generation TAVI device with three unique U-shape graspers(Jie-Cheng Medical Technology,Suzhou,China),was implanted uneventfully.The heart function recovered immediately without any support of vasoactive agents.The electrocardiography showed a 95-bpm sinus rhythm with normal ST-segment.TEE showed excellent placement and function of the new valve(Video 2).The coronary arteries were intact on angiography(Figure 1A and B).The hemodynamic state was stable with a mean arterial blood pressure of 74 mmHg.At 9 min after valve deployment,the heart rate of the patient decreased,systolic blood pressure dropped sharply from 115 to 60 mmHg and central venous pressure abruptly increased from 10 to 33 cmH2O.Epinephrine,norepinephrine,ephedrine,and other vasoactive agents were given immediately to stabilize the hemodynamic status.However,the patient had a poor response to these drugs.At this time,TEE inspection showed poor myocardial contractility.Electrocardiography monitoring showed remarkable STsegment depression.Another angiography was performed immediately.Complete obstruction of the right coronary artery was found(Figure 1C).Angiographic findings are shown in Videos.(Supplementary videos 1,2 and 3)The right coronary ostial obstruction was diagnosed.An emergency protocol was initiated.CPB was established immediately.After aortotomy,the severely calcified left coronary leaflet was found to be dislocated to the opening of the right coronary artery causing complete obstruction(Figure 2).Then aortic biological valve replacement under CPB was performed.
OUTCOME AND FOLLOW-UP
The patient was extubated on the same day and was discharged from the hospital 1 wk after surgery without complications.
DISCUSSION
We report a rare case of delayed-onset right coronary ostial obstruction after successful deployment of the prosthesis in transapical TAVI.Informed consent was signed by the patient.There were some reports of delayed obstruction of a left coronary artery after uneventful TAVI[4,5].Our case showed that obstruction of coronary arteries,either left or right,could occur in the early post-procedural period although the patient had a low perioperative risk.To the best of our knowledge,this is one of the few cases of delayed-onset right coronary ostial obstruction after successful TAVI.
Coronary obstruction during TAVI is commonly caused by calcified aortic valve leaflet,which is compressed to the openings of the coronary arteries[1].In some cases,the original valve itself can block blood flow after balloon expansion.The implant itself can also cause obstructions if not positioned properly.However,in this case,JValve was used.The crown-shaped three-prong claspers of J-Valve were designed to match the annulus of the aortic valve.Such unique design allows the surgeons to holdthe original valve leaflet between the claspers and the new valve,preventing the original valve from shifting to the openings of the coronary arteries[6].Thus obstruction caused by the original valve is avoided[7,8].In this case,the original valve and the annulus were found to be severely calcified.The patient had an enlarged right-coronary cusp.The balloon expansion before valve placement was initially intended to tear the calcified and adhesive leaflets along the physiological fissure.However,the leaflet was torn along the aortic annulus and the valve was divided into a large left-right-coronary portion and a small non-coronary portion(Figure 2).Then the large portion was squeezed between the implanted valve and the claspers.After successful valve deployment,the calcified left-non-coronary portion slowly shifted due to the contraction of the heart and the reciprocating motion of the implanted biological aortic valve.Eventually,the right coronary ostium was blocked.
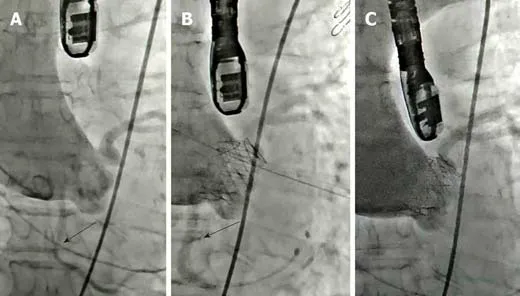
Figure 1 Angiography of J-valve placement.
The typical clinical symptoms of right coronary obstruction during general anesthesia include hemodynamic instability,which is difficult to correct using vasoactive agents,acute right ventricular failure,and various types of arrhythmia according to the blood supply area by the right coronary artery.Thus,prompt recognition by anesthesiologists is particularly important.TEE is a productive diagnostic and monitoring tool that could immediately recognize the reduced myocardial contractility[9].In addition,it can guide the apex puncture,measure the distance between the aortic valve and the ostia of coronary arteries,and evaluate aortic regurgitations and paravalvular leakages.Therefore,we suggest that TEE should be applied in all transapical TAVI cases.Although TEE inspection sometimes could not reveal the actual state of the blood flow to the coronary arteries due to attenuation by implant and calcifications,it is still an extraordinary monitoring tool in addition to angiography.
For such emergencies,a standard protocol should be established and implemented by all the team members.Tamet al[10]reported that emergencies during TAVI required cardiopulmonary resuscitation,CPB,and stabilizing hemodynamic state.However,many large centers are insufficiently prepared for this kind of emergencies.For instance,Fernandeset al[11]reported that in emergent conditions during TAVI,there is a lack of personnel cooperation,leading to the loss of valuable resuscitation time.In our hospital,all transapical TAVI cases are performed by our experienced TAVI team.A standardized transapical TAVI protocol is followed,which requires installation of standby CPB circuit before surgery in case of emergency.
Recently,TAVI has been increasingly performed in intermediate- to low-risk patients.Although these patients have low perioperative risks,severe complications can still occur.Apex puncture,high-rate ventricular pacing,and balloon expansion can cause complications such as coronary obstruction,atrioventricular block,bleeding,and heart rupture.
CONCLUSION
From the perspective of anesthesiologists,transapical TAVI patients should be closely monitored,even after surgery.Sufficient knowledge about the procedure is requiredby the whole team.A comprehensive preoperative evaluation should be performed,and emergency protocols should be established in advance,so that prompt and accurate decisions can be made in emergencies,ensuring timely resuscitation of the patients.
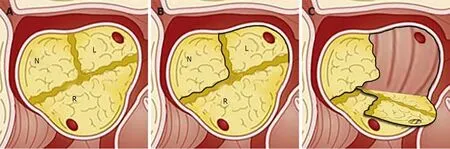
Figure 2 lllustration of the uncommon tear after balloon expansion of the original aortic valve.
World Journal of Clinical Cases2020年4期
- World Journal of Clinical Cases的其它文章
- Extrapleural solitary fibrous tumor of the thyroid gland:A case report and review of literature
- Effectiveness of a microabrasion technique using 16% HCL with manual application on fluorotic teeth:A series of studies
- Prevalence and associated factors of suicide among hospitalized schizophrenic patients
- Lymphoepithelioma-like carcinoma of the upper urinary tract:A systematic review of case reports
- Using Materialise's interactive medical image control system to reconstruct a model of a patient with rectal cancer and situs inversus totalis:A case report
- Diverticulum of the buccal mucosa:A case report
