Extrapleural solitary fibrous tumor of the thyroid gland:A case report and review of literature
Yong Joon Suh,Jung Ho Park,Jae Hyeon Jeon,Sanchir-Erdene Bilegsaikhan
Yong Joon Suh,Jung Ho Park,Department of Breast and Endocrine Surgery,Hallym University Sacred Heart Hospital,Gyeonggi-do 14068,South Korea
Jae Hyeon Jeon,Sanchir-Erdene Bilegsaikhan,Department of Biomedical Science,Hallym University,Chuncheon 24252,South Korea
Abstract
Key words:Solitary fibrous tumor;Mesenchymal neoplasm;Thyroid gland;Surgery;Case report;Review
INTRODUCTION
Solitary fibrous tumor(SFT)is an uncommon spindle-cell neoplasm.In 1931,it was first reported by Klemperer and Coleman[1]as a pleural tumor.Since then,and for many years,as more cases of pleural SFT have been reported in the literature,such neoplasms have been thought to be confined to the pleura as a type of localized fibrous mesothelioma.It has subsequently been recognized in other organs of the body.Now,it is widely accepted that SFT is a rare neoplasm of mesenchymal origin[2].In 1993,SFT derived from the thyroid gland(SFT-T)was first described in three patients presenting with nodular goiters[3].To the best of our knowledge,37 cases have been reported to date,with an increased frequency in the past few years.Typically,patients presented with a slow-growing asymptomatic mass around the neck[4].Microscopically,the tumors are characterized by hypocellular and hypercellular areas,cytologically-bland spindle cells with patternless growth,ectatic branching blood vessels,and variable amounts of collagen[5,6].Well-defined immunohistochemical features and electron microscope findings support a fibroblastic,rather than mesothelial,differentiation of the tumor[7,8].Herein,we report a case of SFT originating from the thyroid gland,as well as a literature review.The patient provided informed consent for the publication of this report.
CASE PRESENTATION
Chief complaints
A 59-year-old man visited our hospital in July 2017 complaining of neck discomfort.
History of present illness
The patient had a history of an enlarged neck mass associated with dysphagia to solids.
Physical examination
At the physical examination,a neck mass with a homogeneous and tender consistency was palpated on the left side of the neck.
Laboratory examination
The patient’s thyroid function test results,including antibody levels,were within normal limits.
Imaging examination
Ultrasonography demonstrated a left-sided thyroid nodule with deviation of the trachea,showing a 4.7 cm × 4.0 cm × 3.2 cm solitary mass of intermediate suspicion in the left lobe(Figure 1).However,the size of the nodule was increased to 5.5 cm × 5.0 cm × 3.4 cm on a follow-up ultrasonography in April 2018.Computed tomographyrevealed a bulky and solid thyroid nodule in the transverse view(Figure 2).
Pathologic evaluation
A fine-needle aspiration biopsy was subsequently performed.The pathologist reported a benign follicular lesion.
FINAL DIAGNOSIS
The final diagnosis was extrapleural SFT-T with a clear resection margin.The specimen showed a well-demarcated and partly encapsulated soft nodule of whitish and tan/brown color on the cut surface(Figure 3A).Light microscopy examination of the surgical specimen revealed high cellularity with moderate cytologic atypia(Figure 3B).The mitotic count was 5/10 high-power fields.There was no tumor necrosis or lymphovascular invasion.Immunohistochemistry staining demonstrated that the tumor cells expressed CD34-positivity and signal transducer and activator of transcription 6(STAT6)-positivity(Figure 3C and D).Neither cytokeratin nor thyroid transcription factor-1 expression was detected(Figure 3E and F).The Ki-67 showed intermediate proliferative activity.
TREATMENT
After a multidisciplinary discussion,the patient underwent a left lobectomy in May 2018.The recurrent laryngeal nerve,as well as the parathyroid glands,was preserved.No vocal cord dysfunction was found in the laryngoscopic evaluation performed after the surgery.
OUTCOME AND FOLLOW-UP
The patient was discharged without complication three days after the surgery.Follow-up examinations have been performed every six months,without any evidence of recurrence.The patient is doing well after 17 mo.
DISCUSSION
SFTs are rare ubiquitous neoplasms of mesenchymal origin[9].The etiology is unknown[10].They have been described as pleural-based lesions[1],but there have been subsequent reports of SFTs in other anatomic sites as well.Less than 0.1% of all tumors arise on the head and neck area[11].The first report of SFT-T was described in 1993[3].Since then,only 37 cases have been published in English articles.A review of this literature is summarized in Table 1.According to the accumulative data,the mean age for the appearance of SFT-T is 54.1 ± 13.0 years(ranging from 28 to 88 years),with no sex predilection(20 females and 18 males).The size of the tumors ranged from 1.5 to 13.8 cm,with a mean size of 5.6 ± 2.8 cm.Sixteen tumors were located on the left lobe,whereas 15 tumors were on the right lobe.Two tumors were found in intrathoracic locations.Among 25 patients with available follow-up data(mean 39.4 ±34.0 mo),one patients experienced a local recurrence and distant metastasis[12].The clinical presentation of SFT-Ts is similar to regular thyroid neoplasms[13].The patient commonly refers to a painless slow-growing mass,but,there may be a rapid increase in volume occasionally[14,15].
SFT-T can only be diagnosed after the exclusion of other thyroid tumors that exhibit spindle-cell morphology[16].Possible differential diagnoses include anaplastic carcinomas,hemangiopericytomas,medullary carcinomas,sarcomas,leiomyomas,neurofibromas,schwannomas,Riedel’s thyroiditis,and lymphomas[17-20].The paucicellular variant of anaplastic thyroid carcinoma is featured by mildly atypical spindle cells in a sclerotic stromal background,which can morphologically resemble SFT-T[4].Even though fine-needle aspiration biopsy is a proper procedure for the evaluation of thyroid nodules,its efficacy in the diagnosis of SFT-T is limited[2,13].Although two reports presented a diagnosis of spindle-cell neoplasm using cytology combined with immunocytochemistry,a definitive confirmation of SFT-T was impossible using this method alone[7,18].Proper diagnosis can be only ensured by the combination of histopathological and immunohistochemical analysis.Microscopically,SFT-T shows a unique morphology,often referred to as a“patternless” pattern,with spindle cell proliferation,intermingled with hypocellularand hypercellular areas[2,15,21].Immunohistochemical analysis of the tumor cells has revealed positivity for progenitor cell marker(CD34),Ewing’s sarcoma cell marker(CD99),apoptotic marker(Bcl-2),and mesenchymal marker(vimentin).However,no immune reactions against epithelial marker(keratin),muscle cell marker(desmin),neuron-specific marker(S-100),and thyroid transcription factor-1 have been reported[19,22].
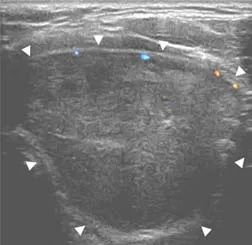
Figure 1 ltrasonography shows a 4.7 cm × 4.0 cm × 3.2 cm heterogeneously enhancing solitary nodule arising from the left lobe of the thyroid gland(white arrow head).
A gene fusion between NAB2 and STAT6 on chromosome 12q13 has been recently identified to be the pathognomonic molecular aberration in SFT[23].NAB2 is a repressor of Early growth response 1(EGR1)target genes.EGR1 is a transcription factor that couples growth factor signaling with the induction of nuclear programs of cellular proliferation and differentiation.The NAB2 fusion gains an activation domain from STAT6,which converts NAB2 into a potent transcriptional activator of EGR1.This leads to constitutive activation of EGR-mediated transcription that drives neoplastic progression.The protein STAT6 detectable by immunohistochemistry,is shown to be a reliable indicator for the NAB2-STAT6 gene fusion[24,25].STAT6 immunohistochemistry is a highly sensitive and specific diagnostic marker for SFT[26,27].In our case,STAT6 immunohistochemistry showed the diffuse strong nuclear positivity.This testing can be considered as a valuable adjunct in the diagnosis of SFT.
SFT-Ts are mainly benign neoplasms and there are no distinct pathologic features to help differentiate benign from malignant lesions[2,9,13].In 1998,Vallat-Decouvelaereet al[28]proposed some characteristics suggesting a more aggressive behavior.The histologic features of malignancy,as defined by the World Health Organization,include the presence of high cellularity,cytological atypia,a higher frequency of mitoses(> 4/10 HPF),and evidence of tumor necrosis or infiltrating margins[29].So far,there has only been one report of malignant SFT-T,which already presented with pulmonary metastasis when diagnosed[12].Even without distant metastasis,the tumor presented two of the above criteria for malignancy(high cellularity and cytological atypia)in the present case.
The primary management of SFT-T is surgical,which also provides a definitive diagnosis[10,13,30].A thyroid lobectomy may be sufficient,if there is no suspicion of malignancy,such as the invasion of surrounding structures.In the present case,there was no intraoperative finding of malignancy.Combined with the intraoperative finding of a normal right lobe,we chose to perform a left thyroid lobectomy.Thyroidstimulating hormone suppression therapy with hormones has no rationale in the management of SFT-T,as the origin of the tumor cells is stromal[12].Indications for chemotherapy or external radiation therapy is controversial,even in malignant tumors[12,17].Specially in cases of malignancy,not much is known about its behavior or prognosis because of the rarity of these tumors.Close follow-up after surgical resection of the lesions seems to be the best management.A review of this literature is summarized in Table 1[31-36].This is the 38thcase of SFT-T reported in English literature to date.
CONCLUSION
SFT-T has been reported to behave indolently with the capacity for potential recurrence and rare metastasis.The literature shows that surgical resection is the treatment of choice.Understanding this disease entity is important for accurate diagnosis and proper management.

Table 1 summary of the clinicopathological features in the reported cases of solitary fibrous tumor derived from the thyroid gland

Figure 2 omputed tomography reveals a bulky and solid thyroid nodule at transverse view(orange arrow head).

Figure 3 istology of a surgical specimen examined under light microscope.
 World Journal of Clinical Cases2020年4期
World Journal of Clinical Cases2020年4期
- World Journal of Clinical Cases的其它文章
- Diverticulum of the buccal mucosa:A case report
- Delayed right coronary ostial obstruction after J-valve deployment in transcatheter aortic valve implantation:A case report
- Using Materialise's interactive medical image control system to reconstruct a model of a patient with rectal cancer and situs inversus totalis:A case report
- Must pilots permanently quit flying career after treatment for colorectal cancer? - Medical waiver for Air Force pilots with colorectal cancer:Three case reports
- Lymphoepithelioma-like carcinoma of the upper urinary tract:A systematic review of case reports
- Prevalence and associated factors of suicide among hospitalized schizophrenic patients
