Upper esophageal sphincter abnormalities on high-resolution esophageal manometry and treatment response of type ll achalasia
Can-Ze Huang,Zai-Wei Huang,Hua-Min Liang,Zhen-Jiang Wang,Ting-Ting Guo,Yu-Ping Chen
Can-Ze Huang,Zai-Wei Huang,Hua-Min Liang,Zhen-Jiang Wang,Ting-Ting Guo,Yu-Ping Chen,Department of Gastroenterology,Zhuhai People’s Hospital(Zhuhai Hospital Affiliated with Jinan University),Zhuhai 519000,Guangdong Province,China
Abstract
Key words:Upper esophageal sphincter;High-resolution esophageal manometry;Achalasia;Treatment response
INTRODUCTION
Many studies involving esophageal motility disorders have been published since the emergence of high-resolution esophageal manometry(HREM).Three versions of the Chicago Classification of Esophageal Motility Disorders have been published[1-3].However,none of the versions has defined upper esophageal sphincter(UES)abnormality metrics or their function.In fact,little is known about the pathophysiology of UES motility disorders.On the one hand,the UES has a complex anatomy,radial asymmetry,and rapid contraction ability[4],which limit the evaluations using conventional manometry.On the other hand,UES abnormalities are often considered incidental findings with no clear clinical significance[5].
However,in recent years,several studies have considered that UES abnormalities correlate with treatment response in patients with achalasia[6,7].Both increased UES basal pressure and residual pressure(RP)have been found in patients with achalasia[7],and pneumatic dilation of the lower esophageal sphincter(LES)has improved intraesophageal and UES minimal relaxation pressures in patients with achalasia[8].Nevertheless,most studies focus on patients with achalasia.In fact,Chavezet al[9]divided their subjects,including patients without achalasia,into those with normal and abnormal UES function.They found that in patients with achalasia or esophagogastric junction(EGJ)outflow obstruction,UES abnormalities are a frequent finding on HREM.Patients with both achalasia and UES dysfunctions had significantly poorer symptomatic improvement after treatment compared with those without UES abnormalities.To date,no studies have investigated the clinical implications of UES abnormalities and their alteration after balloon dilation in patients with achalasia who have both subjective symptomatic improvements using HREM and objective posttreatment manometry.
Therefore,in this study,we analyzed the types of UES abnormalities present and their frequency in consecutive patients with esophageal motility disorders undergoing HREM according to the current Chicago classification.We also determined the association between common clinical symptoms and UES abnormalities.Finally,we assessed the treatment-induced changes in LES and UES objective parameters to evaluate the treatment response among subjects with achalasia and UES dysfunctions.
MATERIALS AND METHODS
Study sample
A total of 498 consecutive patients undergoing clinical HREM studies at our hospital motility laboratory from November 2013 to April 2018 were eligible for inclusion in this study.Further inclusion criteria consisted of symptoms suggestive of an esophageal motility disorder,including dysphagia,noncardiac chest pain,reflux,regurgitation,cough,belching,hiccups,globus,nausea,and vomiting.Patients with upper gastrointestinal surgery,intolerance of HREM,and incomplete data were excluded.All subjects signed an informed consent form about the manometry.This study was approved by the Ethics Committee of Zhuhai People’s Hospital.
High-resolution esophageal manometry
A solid-state high-resolution manometer was employed for all data collection(ManoScan360 High-resolution Manometry System;Given Imaging,Yoqneum,Israel).The characteristics of this device,calibration procedure,and thermal correction measures have been reported in detail previously[10,11].Manometric studies were performed with the patients in the supine position after at least a 6-h fast.Manometric data of the hypopharynx,UES,body of the esophagus,LES,and the stomach,with 3-5 sensors positioned in the stomach,were recorded during the scan.Scanning was done while the patient swallowed 5 mL of water ten times,20-30 s apart.A resting period was assessed either at the beginning or at the end of the session,according to patient tolerance[10].
High-resolution esophageal manometry data analysis
All manometric data were analyzed using ManoView software(Sierra Scientific Instruments)and were corrected for thermal sensitivity of the pressure-sensing elements using temperature compensation.Based on the current Chicago classification,manometric diagnoses included normal,peristaltic abnormalities(weak peristalsis and frequent failed peristalsis),achalasia(types I,II,and III),EGJ outflow obstruction,hypertensive peristaltic disorders(nutcracker esophagus and jackhammer esophagus),aperistalsis,and distal esophageal spasm[1].Types of achalasia were defined as follows:(1)Elevated median LES integrated relaxation pressure(IRP)(> 15 mmHg)and 100% failed peristalsis(distal contraction integral <100 mmHg)in type I achalasia;(2)Elevated median LES IRP(> 15 mmHg),100%failed peristalsis,and panesophageal pressurization with ≥ 20% of swallows in type II achalasia;(3)Elevated median LES IRP(> 15 mmHg),no normal peristalsis,and premature(spastic)contractions with distal contraction integral > 450 mmHg/s/cm and ≥ 20% of swallows in type III achalasia;and(4)EGJ outflow obstruction,where none of the above criteria were met.
Definition of UES pressure and abnormalities
The UES segment length,mean resting pressure(restP),RP,time to nadir pressure,and recovery time were extracted from the analysis software.These parameters of UES were measured throughout the study prior to each of the ten water swallows,and the UES abnormalities recorded included hypotensive UES restP(< 34 mmHg),hypertensive UES restP(> 104 mmHg),and impaired UES relaxation(UES RP > 12 mmHg,time to nadir pressure > 365 ms,relaxation duration time < 480 ms,or recovery time < 259 ms).Normal values were established based on previous studies[12,13].
Treatment method and evaluation in achalasia
All patients with achalasia underwent pneumatic dilation using Rigiflex balloons(Microvasive,Boston Scientific,Watertown,MA,United States)with increasing balloon diameter by an experienced endoscopy specialist.During pneumatic dilation,the balloon was inflated twice in 30 s at pressures of 5 and 7 psi and again within 60 s at 10 psi.If one dilation was not enough,an additional dilation was performed.An HREM was employed after dilation to ensure the LES IRP was significantly reduced.Favorable treatment response was defined qualitatively by Eckardt score(decrease to 3 or below)and quantitatively by posttreatment HREM(LES IRP was significantly reduced in the posttreatment stage compared with that in the pretreatment stage).
Statistical analysis
HREM parameters are reported as the mean ± SE.Comparisons of UES abnormality and categorical variables were performed usingχ2test for binary data and Fisher’s exact test for small samples.Age was compared using a two-samplet-test.For the achalasia subtypes and UES abnormalities,one-way ANOVA and Bonferroni correction were used for continuous variables andχ2test was used for binary data.Linear mix effects model was built with the LES restP,LES IRP,and UES RP as the dependent variables and age,sex,and treatment stage(pre-vspost-treatment)as the independent variables.The Wilcoxon signed rank test was used to assess associations between treatment-induced changes in LES and UES,controlling for the type of achalasia.Two-sidedP≤ 0.05 was considered statistically significant.
RESULTS
Patient characteristics,symptom profiles,and HREM diagnoses based on UES parameters
Of the 498 consecutive patients(age 45.73 ± 12.73 years,52.4% female)who underwent clinical HREM studies,246(49.40%)were found to have UES abnormalities,and 252(50.60%)had normal UES(Figure 1).UES abnormalities were frequently identified at our hospital motility laboratory.There was no significant difference in the sex distribution between subjects with abnormal UES(51.22%female)and normal UES(51.98% female;Table 1).However,subjects with UES abnormalities were older than the UES normal group(48.05 ± 13.28 yearsvs43.71 ±12.18 years,P< 0.002).Chest pain was less likely to be present in subjects with abnormal UES(16.26%vs25.79%,P< 0.05),but other symptoms(including dysphagia,heartburn,abdominal pain,sour regurgitation,ructus,cough,hiccup,and globus hystericus)were not significantly different between the two groups(Table 1;P> 0.05).
Referring to the current Chicago Classification of Esophageal Motility Disorders,the rate of ineffective esophageal motility was found to be significantly different between subjects with abnormal UES and normal UES(16.67%vs9.13%;Table 2;P<0.05).Achalasia was more likely if an UES abnormality was present.The incidence rate of achalasia,especially type II achalasia,was higher in subjects with abnormal UES than in subjects with UES normal(5.28%vs1.59%;Table 2;P< 0.05).Other manometric diagnoses,such as EGJ outflow obstruction,contraction vigor(failed,weak,and normal),distal esophageal spasm,hypercontractile esophagus,and fragmented contraction,were not significantly different between the two groups(Table 2;P> 0.05).
UES abnormality subtypes
To further investigate UES abnormalities,we divided subjects with abnormal UES into five subgroups:Hypertensive alone(UES RP > 104 mmHg),hypotensive alone(UES restP < 34 mmHg),impaired relaxation alone(UES RP > 12 mmHg,time to nadir pressure > 365 ms,relaxation duration time < 480 ms,or recovery time < 259 ms),hypertensive with impaired relaxation,and hypotensive with impaired relaxation.As shown in Table 3,impaired relaxation alone was the most common abnormality in UES(52.85%,n= 130),followed by hypotension alone(17.07%,n= 42).There was a significant difference in age among the five subgroups(Table 3;P< 0.01).Based on HREM diagnosis,fragmented contraction was significantly different among the subgroups.It was more likely for fragmented contraction to occur in the hypotensive with impaired relaxation subgroup than in the other subgroups(21.88%;Table 3;P< 0.01).There was also a significant difference in the achalasia rate among the five subgroups.The highest incidence rate of achalasia was found in the hypertensive with impaired relaxation subgroup(20.00%;Table 3;P< 0.05).The rates of other manometric diagnoses,such as EGJ outflow obstruction,contraction vigor(failed,weak,and normal),distal esophageal spasm,hypercontractile esophagus,and ineffective esophageal motility,were not significantly different among the subgroups(Table 3;P> 0.05).
With regard to symptoms in UES abnormality subtypes,heartburn most frequently occurred in the hypotensive with impaired relaxation subgroup(53.13%;P< 0.05),followed by the hypertensive alone subgroup(40.74%;P< 0.05).Other symptoms(including dysphagia,abdominal pain,chest pain,sour regurgitation,ructus,cough,hiccup,and globus hystericus)had similar rates among the subgroups(Table 3;P>0.05).
Secondary analyses of UES parameters after combined LES function
Subjects were divided into LES normal and LES abnormal groups in accordance with LES restP and LES IRP.In the LES normal group,both LES restP and LES IRP were in the normal range according to the current Chicago Classification of Esophageal Motility Disorders.In contrast,in the LES abnormal group,either LES restP or LES IRP was outside the normal range.We found that age and dysphagia symptoms were significantly different between subjects with abnormal and normal UES in the LESnormal group(Table 4;P< 0.05):Patients with UES abnormalities were older than UES normal subjects(47.35 ± 13.40 yearsvs42.82 ± 12.08 years,P< 0.05),and dysphagia was less likely in UES abnormal than in UES normal patients(P< 0.05).Additionally,in the LES abnormal subgroup,the incidence rate of type II achalasia was significantly higher in subjects with abnormal UES compared with the UES normal group(9.77%vs2.58%;Table 5;P= 0.01),but other HREM diagnoses were not different(Table 5;P> 0.05).There was also no significant difference in symptoms between the two groups in the LES abnormal subgroup(Table 5;P> 0.05).
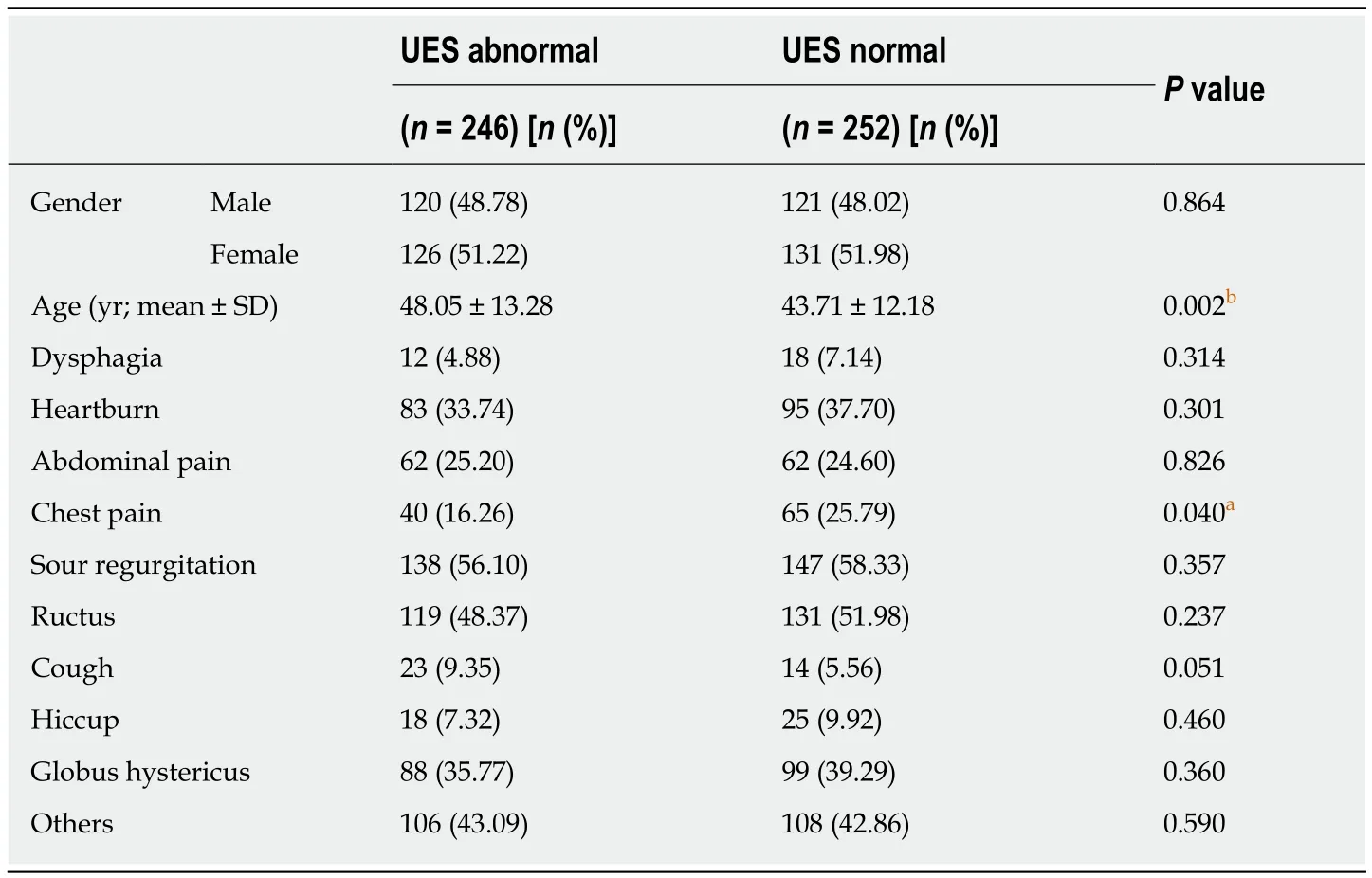
Table 1 Demographic characteristics and symptom profiles of subjects based on upper esophageal sphincter parameters
Treatment response among subjects with type II achalasia
To elucidate the treatment response among subjects with type II achalasia,we performed HREM both in the pre- and post-treatment stages.Ten subjects with achalasia were excluded from the analysis due to a lack of pre- or post-treatment manometric data(Figure 1).After pneumatic dilation,LES restP and LES IRP were significantly decreased(41.91 ± 9.20vs26.18 ± 13.08,38.94 ± 10.28vs16.71 ± 5.65,respectively;Figure 2;Table 6;P< 0.05).This meant that the treatment was effective in these subjects.The UES RP also decreased after dilation(11.18 ± 7.93vs5.35 ± 4.77;Figure 2;Table 6;P< 0.05),but the UES restP,the percentage of failed swallows,the percentage of early contractions,and the percentage of rapid contractions did not(Table 6;P> 0.05).In a mixed analysis,age,sex,and treatment stage were controlled for as between-subject independent variables,considering the random effect of the individual and the effect of repeated measurement before and after treatment.LES restP,LES IRP,and UES RP were significantly reduced in the posttreatment stage(Table 7;LES restP:P< 0.01;LES IRP:P< 0.001;UES RP:P< 0.05).
An additional analysis to assess for clinical treatment improvement after therapy among the patients with type II achalasia was performed based on an Eckardt score scale.This score was collected from the patient’s subjective report of symptoms in pre- and post-treatment follow-up visits.As shown in Table 8,subjects with type II achalasia and abnormal UES presented a significantly poorer treatment response compared with those with normal UES(83.33%vs0.00%;Table 8;P< 0.05).
DISCUSSION
UES abnormalities are frequently found on HREM,e.g.,49.40% in the current study.However,little is known about the clinical significance of UES motility disorders.In this study,we aimed to demonstrate the manometric differentiation on HREM between subjects with abnormal UES and normal UES,and the association between UES type and the treatment response of type II achalasia.
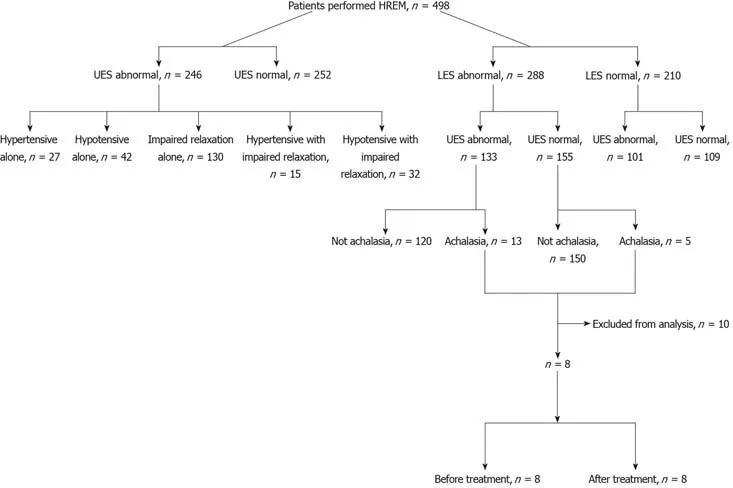
Figure 1 Study profile.
UES abnormalities are often ignored because manometry is challenging in traditional esophageal motility analysis.Many interesting discoveries on UES manometric abnormalities using HREM have been reported in recent years.In a previous study,the majority of UES abnormalities were hypertensive[9].The current study is the first to divide patients into subgroups considering abnormal UES factors jointly.It is worth noting that hypertensive or hypotensive UES pressure often combines with impaired relaxation.Hence,we divided subjects with UES abnormalities into five subgroups:Hypertensive alone,hypotensive alone,impaired relaxation alone,hypertensive with impaired relaxation,and hypotensive with impaired relaxation.We found that impaired relaxation alone was the most common UES abnormality(52.85%,n= 130),followed by hypotension alone(17.07%,n= 42).The definition of UES impaired relaxation is not concordant.UES relaxation involves inhibition of cricopharyngeus and contraction of suprahyoid muscles.It is not only a lower UES RP but also comprises the time to nadir pressure,relaxation duration time,and recovery time.Elevated UES RP has been seen in impaired anterior traction,large bolus swallows,extreme neck extension,and impaired relaxation of the UES[14].Note that medullary swallow center lesions also cause impaired UES relaxation[4];this has also been observed in Parkinson's disease and myopathy[15].
It is mostly acknowledged that UES function is influenced by LES function.Thus,it is necessary to combine LES function when investigating UES dysfunction.In a previous study,it was demonstrated that patients with impaired LES relaxation were more likely to have an UES abnormality present[9].In our current study,we discovered that the incidence rates of UES abnormalities in subjects with normal LESvsin subjects with abnormal LES were not significantly different.It is noteworthy that the incidence rate of type II achalasia was significantly higher in the UES abnormal group than in the UES normal group,but other HREM diagnoses were not.In fact,UES RP can be used to differentiate achalasia subtypes within the EGJ outflow obstruction[16].These findings suggest that abnormal UES is associated with type II achalasia.UES abnormalities may be a feature of type II achalasia and may contribute to the diagnosis of this disease.
Another characteristic of type II achalasia with abnormal UES is a poor treatment response.Previous researchers reported that abnormal UES was significantly associated with a poor treatment response in the presence of achalasia[6,9].Interestingly,only type II achalasia with abnormal UES,but not type I or type III,has been correlated with a poorer therapeutic effect[8].In fact,UES RP and UES IBP were increased after balloon dilation in type I achalasia[8].Thus,we analyzed the treatment response in subjects with type II achalasia through both subjective symptomaticimprovement and objective posttreatment manometry.We observed that LES restP and LES IRP were significantly decreased after balloon dilation.These findings are consistent with those of Pandolfinoet al[17],who found that patients with type II achalasia had the best response to therapeutic interventions for the EGJ.However,we discovered that a poorer treatment response was associated with abnormal UES in type II achalasia.Achalasia is characterized by an elevated median LES IRP(> 15 mmHg)and an absence of esophageal body peristalsis with or without panesophageal pressurization with ≥ 20% of swallows[1].The mechanism of the poor treatment response in type II achalasia with UES dysfunction remains unclear.Within achalasia subtypes,UES RP was the most common in type II achalasia[16].Chavezet al[9]hypothesized that elevated UES pressure resulted from a compensatory and protective effect against inadequate esophageal clearance and/or regurgitation due to impaired LES relaxation.Wauterset al[8]also pointed out that increased UES RP may be a secondary response to poor esophageal emptying and higher intraesophageal pressures.Consequently,we suppose that reducing intraesophageal pressure by EGJ balloon dilation in type II achalasia patients leads to less compensatory reflex in UES function.This is further supported by the fact that the UES RP was significantly reduced in the posttreatment stage in our study.Importantly,abnormal UES appears to be a potentially prognostic indicator of treatment in subjects with type II achalasia.

Table 2 High-resolution esophageal manometry diagnoses based on the presence of upper esophageal sphincter abnormalities
A potential limitation of this study is its retrospective and single-center design.This inevitably limits our ability to draw causative conclusions.Another drawback is the limited number of achalasia patients in each category,especially excluding ten patients with achalasia.This hindered us in analyzing treatment response in each subtype of achalasia and after other treatment methods.A prospective and multicenter study is necessary to obtain causal conclusions.In future HREM studies,a large number of subjects are needed to enroll to elucidate the relationship between treatment response and UES dysfunction in all achalasia subtypes and under other treatment methods.
In conclusion,our study illustrates that UES abnormalities are frequently found on routine HREM.Impaired relaxation alone is the most common UES abnormality,followed by hypotension alone.The incidence of type II achalasia is associated with abnormal UES in the LES abnormal subgroup.A poorer treatment response of type IIachalasia is seen with abnormal UES,which is potentially a prognostic indicator of treatment in this disease.

Table 3 Upper esophageal sphincter abnormality subtypes based on high-resolution esophageal manometry diagnosis

Table 4 Comparisons between upper esophageal sphincter abnormal and upper esophageal sphincter normal patients in the lower esophageal sphincter normal group

Table 5 Comparisons between upper esophageal sphincter abnormal and upper esophageal sphincter normal patients in the lower esophageal sphincter abnormal group
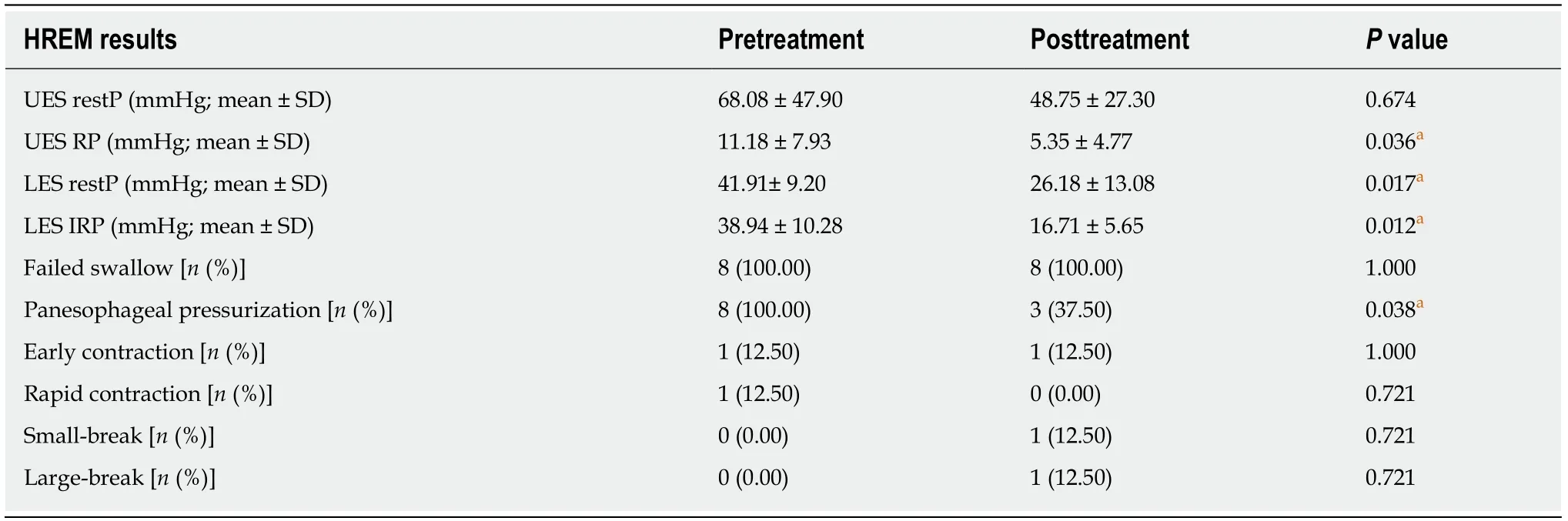
Table 6 Comparisons of high-resolution esophageal manometry results between pretreatment and posttreatment

Table 7 Mixed analysis of lower esophageal sphincter mean resting pressure,lower esophageal sphincter integrated relaxation pressure,and upper esophageal sphincter residual pressure
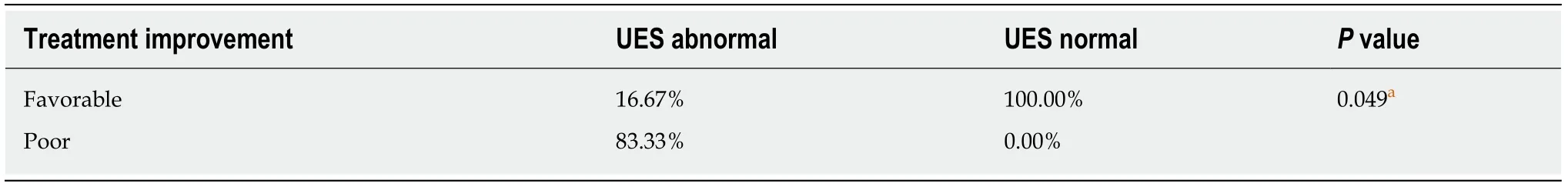
Table 8 Treatment improvement in subjects with type ll achalasia based on upper esophageal sphincter dysfunction
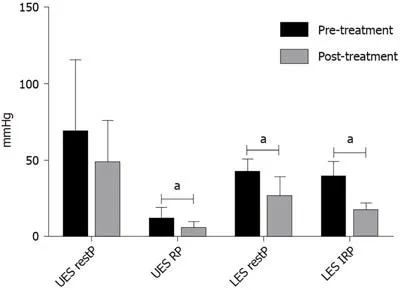
Figure 2 Differences in lower esophageal sphincter mean resting pressure,lower esophageal sphincter integrated relaxation pressure,upper esophageal sphincter mean resting pressure,and upper esophageal sphincter residual pressure between pretreatment and posttreatment stages.
ARTICLE HIGHLIGHTS
Research background
Little is known about the clinical significance of upper esophageal sphincter(UES)motility disorders and their association with the treatment response of type II achalasia.None of the three versions of the Chicago Classification of Esophageal Motility Disorders has defined UES abnormality metrics or their function.UES abnormalities exist in some patients and indicate a clinically significant problem in patients with achalasia.
Research motivation
We analyzed the types of UES abnormalities present and their frequency in consecutive patients with esophageal motility disorders undergoing HREM according to the current Chicago classification.We also determined the association between common clinical symptoms and UES abnormalities.Finally,we assessed the treatment-induced changes in LES and UES objective parameters to evaluate the treatment response among subjects with achalasia and UES dysfunctions.
Research objectives
The research objectives of this study were to demonstrate the manometric differentiation on high-resolution esophageal manometry between subjects with abnormal UES and normal UES,and the association between UES type and the treatment response of type II achalasia.
Research methods
In total,498 consecutive patients referred for high-resolution esophageal manometry were analyzed retrospectively.Patients were divided into those with normal and abnormal UES function.UES parameters were analyzed after determining lower esophageal sphincter(LES)function.Patients with type II achalasia underwent pneumatic dilation for treatment.Using mixed model analyses,correlations between abnormal UES and treatment response were calculated among subjects with type II achalasia.
Research results
Of the 498 consecutive patients,246(49.40%)were found to have UES abnormalities.Impaired relaxation alone was the most common UES abnormality(52.85%,n= 130).The incidence rate of type II achalasia was significantly higher in subjects with abnormal UES than those with normal UES(9.77%vs2.58%,P= 0.01).After pneumatic dilation,LES resting pressure,LES integrated relaxation pressure,and UES residual pressure were significantly decreased(41.91 ± 9.20vs26.18± 13.08,38.94 ± 10.28vs16.71 ± 5.65,and 11.18 ± 7.93vs5.35 ± 4.77,respectively,P< 0.05).According to the Eckardt score,subjects with type II achalasia and abnormal UES presented a significantly poorer treatment response than those with normal UES(83.33%vs0.00%,P< 0.05).
Research conclusions
Our study illustrates that UES abnormalities are frequently found on routine HREM.Impaired relaxation alone is the most common UES abnormality,followed by hypotension alone.The incidence of type II achalasia is associated with abnormal UES in the LES abnormal subgroup.A poorer treatment response of type II achalasia is seen with abnormal UES,which is potentially a prognostic indicator of treatment in this disease.
Research perspectivesThis article reflects a poorer treatment response of type II achalasia with abnormal UES,which is potentially a prognostic indicator of treatment in this disease.However,the limited number of achalasia patients in each category hindered us in analyzing treatment response in each subtype of achalasia.A prospective and multicenter study is necessary to obtain causal conclusions.In future HREM studies,a large number of subjects are needed to enroll to elucidate the relationship between treatment response and UES dysfunction in all achalasia subtypes and under other treatment methods.
World Journal of Clinical Cases2020年4期
- World Journal of Clinical Cases的其它文章
- Must pilots permanently quit flying career after treatment for colorectal cancer? - Medical waiver for Air Force pilots with colorectal cancer:Three case reports
- Prevalence and associated factors of suicide among hospitalized schizophrenic patients
- Lymphoepithelioma-like carcinoma of the upper urinary tract:A systematic review of case reports
- Extrapleural solitary fibrous tumor of the thyroid gland:A case report and review of literature
- Delayed right coronary ostial obstruction after J-valve deployment in transcatheter aortic valve implantation:A case report
- Diverticulum of the buccal mucosa:A case report
