Risk factors for long-term prognosis of hepatocellular carcinoma patients after anatomic hepatectomy
Ya-Li Tian,Jing-Jing Ji,Lu-Ning Chen,Xin-Long Cui,Shi-Teng Liu,Liang Mao,Yu-Dong Qiu,Bing-Bing Li
Ya-Li Tian,Jing-Jing Ji,Lu-Ning Chen,Xin-Long Cui,Bing-Bing Li,Department of Anesthesiology,Drum Tower Hospital Affiliated with the Nanjing University Medical School,Nanjing 210008,Jiangsu Province,China
Shi-Teng Liu,Liang Mao,Yu-Dong Qiu,Department of Surgery,Division of Hepatobiliary and Pancreatic Surgery,Drum Tower Hospital Affiliated with the Nanjing University Medical School,Nanjing 210008,Jiangsu Province,China
Abstract
Key words:Hepatocellular carcinoma;Hepatectomy;Risk factors;Prognosis
INTRODUCTION
Primary hepatocellular carcinoma(HCC)associated with hepatitis B infection is the second most common cause of cancer-related death in China,with an estimated annual death of 383000,accounting for 45% of the total number of liver cancer deaths worldwide[1,2].HCC is an insidious illness and has no specific or prominent symptoms,even in the later stage of this disease;HCC is commonly complicated by microscopic vascular invasion when a definitive diagnosis is first made.Liver surgery is still the mainstay for curing HCC,including liver resection or liver transplantation,but the prognosis of those patients is still poor[3,4].Previous data have indicated that HCC has an estimated annual recurrence rate of 15%-20%,which is the leading factor responsible for the compromised therapeutic efficacy of hepatectomy[5].Makuuchiet al[6]first introduced the procedure of precise anatomic hepatectomy in 1985;the procedure features complete excision of the tumor-bearing portal tributaries.With the practice of precise anatomic hepatectomy emerging in recent years,this procedure provides the maximal safety margin of tumor resection,playing a crucial role in reducing cancer metastasis and recurrence.Many studies have identified that the complete removal of tumor-bearing portal tributaries compared with non-anatomical resection improves survival in patients after hepatectomy[7,8].The data from our institute indicated that the 3-year survival rate of solitary HCC patients undergoing anatomic hepatectomy was significantly improved compared with that of patients undergoing non-anatomical resection(64.9%vs48.1%).The recurrence rate and median time to recurrence in the anatomic resection group were 41.9% and 48.0 mo,respectively,compared with 58.9% and 30.0 mo,respectively,after surgery in the nonanatomic resection group[9].Regardless,the factors responsible affecting long-term prognosis in HCC patients treated by anatomic hepatectomy are still lacking.Therefore,the present retrospective study aimed to evaluate the risk factors for recurrence-free survival among HCC patients after anatomic liver resection.
MATERIALS AND METHODS
Ethical approval
This study was approved by the ethics committee of Drum Tower Hospital Affiliatedwith the Nanjing University Medical School.
Patient selection and data collection
From January 2013 to December 2015,a total of 94 HCC patients who underwent precise anatomic hepatectomy at our institution were found,but ultimately only 74 included in this study.The Child-Pugh classification of these patients was not different prior to the surgery.Information,including patient age,sex,liver function grade,Barcelona clinic liver cancer(BCLC)stage,clinical stage,cancer grade on diagnostic biopsies,tumor size,surgical procedure,perioperative anesthesia management,and prognosis,was collected from the electronic charter system(Medisystem,Suzhou,China)in our hospital.The diagnosis of HCC was confirmed with image data and histopathological staining of the tumor specimen of the resected liver tissue.Patients who received any neoadjuvant treatments,such as transcatheter arterial chemoembolization or radiofrequency ablation,prior to surgery were excluded.Patients who had incomplete detailed clinical records or who did not have regular postoperative follow-up data were also excluded from this study.Anatomic hepatectomy was performed to achieve any type of complete excision of at least one segment based on Couinaud’s classification.After the precise dissection and control of the hepatic pedicle of the target part of the liver under the guidance of intraoperative ultrasound,the surgeons transected the liver parenchyma along the demarcation line.All surgical specimens were examined macroscopically and microscopically to determine surgical margins.All the operations were conducted by the same surgical team from the Department of Hepatobiliary Pancreatic Surgery at our institution.
Estimated blood loss(EBL)was estimated by the following formula:The weight difference of sterile gauze before and after surgery + the amount of fluid in the drainage bottle - the amount of saline flushed during the operation.Intraoperative hypotension(IOH)was defined as a decrease in the baseline mean arterial pressure over 20% for 5 min.
Follow-up
Follow-up examinations,which consisted of routine blood biochemistry,serum AFP measurements,and abdominal ultrasound or computed tomography(CT)if necessary,were performed once every 3 to 6 mo for the first 2 years and once every 6 to 12 mo thereafter.Once tumor recurrence was suspected,further examinations(CT or magnetic resonance imaging)were conducted to confirm or rule out.The diagnosis of HCC recurrence was based on the typical images of CT or magnetic resonance imaging scans,with or without elevated alpha-fetoprotein.The primary endpoint of this analysis was recurrence-free survival,defined as the interval from the date of surgery to that of diagnosis for the first recurrence,the date of death,or the deadline for follow-up.
Statistical analysis
The statistical methods of this study were reviewed by Professor Bi-Yun Xu at Department of Research,Drum Tower Hospital Affiliated with the Nanjing University Medical School,Nanjing,Jiangsu Province,China.
The statistical analyses were performed using Statistical Package for the Social Sciences version 22.Continuous variables are expressed as the mean ± SD or median with range.Categorical variables are expressed as proportions.Survival curves and the survival rate were calculated by the Kaplan-Meier method and analyzed using the log-rank test(P< 0.1).The prognostic value of each variable for affecting recurrencefree survival was assessedviamultivariate Cox proportional hazards regression analysis.The threshold for significance was established atP< 0.05.
RESULTS
Patient demographics and outcomes
A total of 94 patients definitively diagnosed with HCC undergoing precise anatomic hepatectomy were identified during this study period.Four patients receiving TACE/interventions prior to surgery,one patient who died of circulatory failure after surgery,and fifteen patients not completing the follow-up were excluded from this study.As a result,74 patients who underwent precise anatomic liver surgery were eligible for this study(Figure 1).The mean follow-up time was 27.82 mo(range,1.84 to 36 mo).Of the 74 patients,the mean age was 58 years(range,35 to 81 years).The proportion of hypertensive patients accounted for 30.7%.The mean 1-year and 3-year recurrence-free survival durations were 10.9 mo(range,1 to 12 mo)and 24.7 mo(range,1 to 36 mo),respectively.Their demographic and clinical data are summarized in Table 1.

Table 1 Baseline characteristics of study participants(n = 74)
At the endpoint of the follow-up,the overall 1-year survival rate and the recurrence-free survival rate were 78.38% and 68.92%,respectively;the 3-year overall survival rate and the recurrence-free survival rate were 62.16% and 55.41%,respectively,after undergoing precise anatomic hepatectomy,as shown in Figure 2.
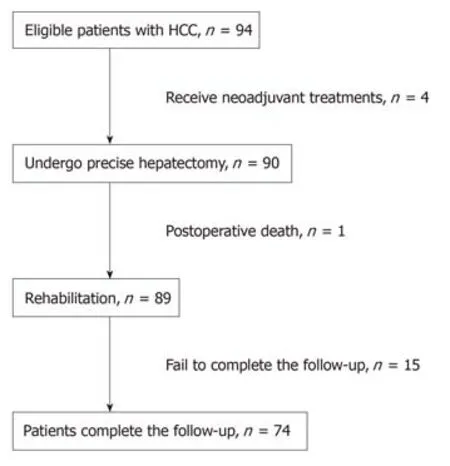
Figure 1 Flow diagram of patients enrolled in this study.
Prognostic factors for 3-year recurrence-free survival
Twenty-three(31.1%)patients died within 1 year after the presence of tumor recurrence-related complications after precise hepatectomy.The mean 1-year recurrence-free survival duration was 10.9 mo(range,1-12 mo).The analysis of diverse variables was conducted and is summarized in Table 2.
Thirty-one(41.9%)patients died within 3 years after the presence recurrencerelated major complications after hepatectomy.The mean survival duration of these patients after the operation was 24.7 mo(range,1-36 mo).The analysis of diverse perioperative variables was conducted,and the results are summarized in Tables 1 and 2.The 3-year recurrence-free survival rate was significantly correlated with preoperative cirrhosis,jaundice(bilirubin level),diabetes,tumor stage,tumor size,IOH,frequency of hypotensive episodes,EBL,blood transfusion,intraoperative fluid volume,and postoperative infection(P< 0.1,Table 2).The significant risk factors were subjected to multivariate Cox proportional hazards regression analysis,which identified hepatic cirrhosis,tumor stage,and the incidence of IOH and EBL as independent risk factors for 3-year recurrence-free survival(P< 0.05,Table 3).
DISCUSSION
Although much progress has been made in the past few decades in terms of surgical techniques,perioperative management,and the understanding of liver anatomy,hepatectomy remains a high-risk interventional procedure for HCC patients with a high 5-year mortality rate of approximately 33.3%-70%[10].A recent study from Zhaoet al[9]indicated that the application of precise anatomic hepatectomy rendered the beneficial effect in decreasing the recurrence of HCC.Patients who underwent nonanatomic liver resection were prone to early and marginal recurrence.The results from our retrospective study similarly showed that the long-term prognosis(1-year and 3-year recurrence-free survival)was better compared with that of patients undergoing the non-anatomic procedure from the previous data.Anatomic liver resection ensures that the tumor is resecteden blocin normal liver tissues out of the tumor mass with no tumor infiltration to improve the radical resection rate,which is thought to be one of the important determinants for reduced tumor metastasis and recurrence.Although prognostic factors or oncologic outcomes have been analyzed in patients after hepatectomy in multitudes of previous retrospective studies[11,12],the predictors of long-term outcomes in patients following precise anatomic hepatectomy are still lacking.Notably,in addition to several risk factors comprising tumor stage,preoperative cirrhosis,and intraoperative blood loss,which have also been identified to be relevant to the prognosis of HCC patients by other investigators[13,14],we found that the hypotension events during the surgery were highly associated with the poor outcome of HCC patients after precise anatomic hepatectomy in the present study.
IOH is actually not uncommon,and the incidence ranges from 5% to 99%depending on the threshold used to define hypotension.The deleterious effects ofhypotension during surgery have been underestimated previously until a prospective observational study from Monket al[15]indicated that the 1-year mortality of patients was most strongly correlated not only with preexisting comorbidity but also with the incidence of IOH(defined as systolic hypotension less than 80 mmHg),depending on the duration of hypotension.The association of IOH with 1-year mortality in noncardiac surgery has been identified in several studies[16].However,the retrospective study conducted by Bijkeret al[17]did not elicit the causative association between IOH and 1-year mortality despite using 48 distinct definitions for hypotension in noncardiac surgery.These conflicting results can be attributed to the nonunified threshold of IOH for a wide spectrum of surgeries and different populations because each individual is different in terms of the varying comorbid factors,baseline conditions,and thresholds of tolerance to hemodynamic insults.Therefore,we designated a decrease in the baseline mean arterial pressure over 20%for 5 min as IOH in the anatomic liver resection procedure in the present study.An intriguing finding was that the incidence of IOH could cause a detrimental effect on the 3-year survival of HCC patients,regardless notably of the time or duration of IOH during the operation.This suggests that IOH might render an unfavorable impact on the long-term outcome for carcinoma patients.Hypoperfusion status and hypoxic environment are favorable for tumor cell mitosis and angiogenesis,accounting for neoplasm recurrence.The adverse relationship between intraoperative hypotension and long-term survival in HCC patients needs to be validated in prospective randomized control trials.

Figure 2 Kaplan-Meier survival curves of 1-year and 3-year survival rates.
Intraoperative blood loss is associated with immediate outcomes and mortality in patients undergoing noncardiac surgery.Several lines of evidence from multiple studies have suggested that massive bleeding(>1000 mL)can independently predict postoperative survival and recurrence after hepatectomy[18-20].In accordance with these previous results,the multivariate analysis in this study identified estimated blood loss(>800 mL)as an independent risk factor responsible for decreased 3-year recurrence-free survival in HCC patients undergoing anatomic hepatectomy.It has generally been accepted that blood loss during hepatectomy is relevant to the extension of liver resection and the complexity of the procedure(vascularreconstruction),which,to some extent,represents the advanced stage of the tumor with a poor prognosisper se.Although blood loss did not correlate with tumor stage(P= 0.235,odds ratio [OR] = 1.378)or size(P= 0.729,OR = 1.250),EBL was confirmed to be one of the factors related to patient survival after hepatectomy.However,some reports have suggested that the impact of bleeding on prognosis is mainly caused by the event of blood transfusion,not the blood lossper se[21].Therefore,whether perioperative blood transfusion will adversely affect the prognosis of cancer patients remains a controversial issue in humans[22,23].Multivariate analysis in this study implicated that blood transfusion did not affect the recurrence-free survival ofpatients undergoing precise hepatectomy.We speculate that the composite effect of blood transfusion could be precisely delineated once considering the values of prompt rectification of anemia and maintenance of hemodynamic stability,not the blood transfusion-associated immunity repression effect alone[24].
系统基于地理信息大数据技术,将土地利用现状、规划、基本农田、水系等国土数据进行了整理,并充分利用地理国情数据提取周边工矿企业、开发区、旅游区、大型经济作物集中连片区、地质灾害点等专题信息,进行地理空间大数据分析,辅助异地搬迁安置点分析等业务决策。如图5、6所示。

Table 2 Univariate analyses of intraoperative and postoperative factors associated with 1-year and 3-year recurrence-free survival of hepatocellular carcinoma patients

Table 3 Multivariate analyses of the intraoperative and postoperative factors associated with 3-year recurrence-free survival of hepatocellular carcinoma patients
Our results,which are in line with those of previous studies,also suggest that preoperative cirrhosis is a predictor of long-term recurrence-free survival in HCC patients.The 3-year recurrence-free survival rate and the average recurrence-free time in the cirrhotic group were lower than those in the noncirrhotic group.This might be due to the hepatic decompensation caused by ongoing cirrhosis itself in cirrhotic patients[25].
Our study has several limitations.First,this was a single-center retrospective study concerning the long-term outcome of patients undergoing anatomic hepatectomy by the same surgical team.The sample size was small,and selective bias may thus be inevitable.Second,inconsistent with the previous study,several tumor biological features,including tumor size with/without satellite foci,portal vein cancer thrombus,and preoperative AFP level,did not show a close correlation with 3-year recurrence-free survival in the present study.We cannot exclude the possibility that the aforementioned factors might have a relatively negligible impact on the prognosis of HCC patients undergoing anatomic hepatectomy.Third,the IOH criteria used in the present study were based on the definition of a decrease in the baseline mean arterial pressure over 20%,according to the majority of previous studies.However,it is uncertain whether a different definition would have served as a better predictor of disease recurrence for these HCC patients.Therefore,a multicenter and large-sample,randomized,controlled trial is warranted to validate the findings of our study.
In conclusion,tumor stage and preoperative cirrhosis adversely affect the postoperative recurrence-free survival rate in patients with hepatocellular carcinoma following anatomic hepatectomy.Furthermore,intraoperative hypotension and blood loss are the key determinants of long-term outcomes for HCC patients.Therefore,strict blood pressure control and reducing blood loss during surgery may improve the long-term prognosis of HCC patients following anatomic hepatectomy.
ARTICLE HIGHLIGHTS
Research background
The risk factors for patients with major postoperative complications immediately after liver resection have been identified;however,the intermediate and long-term prognoses for these patients have yet to be determined.
Research motivation
The aim of the study was to evaluate the factors responsible for the long-term recurrence-free survival rate in patients with hepatocellular carcinoma(HCC)following anatomic hepatectomy.
Research methods
We performed a retrospective analysis of 74 patients with HCC who underwent precise anatomic hepatectomy at our institution from January 2013 to December 2015.The observational endpoints for this study were the tumor recurrence or death of the HCC patients.The overall follow-up duration was 3 years.The recurrence-free survival curves were plotted by the Kaplan-Meier method and were analyzed by the log-rank test.The value of each variable for predicting prognosis was assessedviamultivariate Cox proportional hazards regression analysis.
Research results
The 1-year and 3-year recurrence-free survival rates of HCC patients were 68.92% and 55.41%,respectively,following anatomic liver resection.The results showed that the 3-year recurrencefree survival rate in HCC patients was closely related to preoperative cirrhosis,jaundice level,tumor stage,maximal tumor diameter,complications of diabetes mellitus,frequency of intraoperative hypotensive episodes,estimated blood loss,blood transfusion,fluid infusion,and postoperative infection(P< 0.1).Based on multivariate analysis,preoperative cirrhosis,tumor stage,intraoperative hypotension,and estimated blood loss were identified to be predictors of 3-year recurrence-free survival in HCC patients undergoing anatomic hepatectomy(P< 0.05).
Research conclusions
Tumor stage and preoperative cirrhosis adversely affect the postoperative recurrence-free survival rate in patients with hepatocellular carcinoma following anatomic hepatectomy.Furthermore,intraoperative hypotension and blood loss are the key determinants of long-term outcomes for HCC patients.Therefore,strict blood pressure control and reducing blood loss during surgery may improve the long-term prognosis of HCC patients following anatomic hepatectomy.
Research perspectives
It is uncertain whether a different definition would have served as a better predictor of disease recurrence for these HCC patients.Therefore,a multicenter and large-sample,randomized,controlled trial is warranted to validate the findings of our study.
ACKNOWLEDGEMENTS
The authors would like to thank Professor Bi-Yun Xu for her kind assistance in data collection and statistical analysis.
World Journal of Clinical Cases2020年4期
- World Journal of Clinical Cases的其它文章
- Must pilots permanently quit flying career after treatment for colorectal cancer? - Medical waiver for Air Force pilots with colorectal cancer:Three case reports
- Prevalence and associated factors of suicide among hospitalized schizophrenic patients
- Lymphoepithelioma-like carcinoma of the upper urinary tract:A systematic review of case reports
- Extrapleural solitary fibrous tumor of the thyroid gland:A case report and review of literature
- Delayed right coronary ostial obstruction after J-valve deployment in transcatheter aortic valve implantation:A case report
- Diverticulum of the buccal mucosa:A case report
