Streptococcus agalactiae:Identification methods,antimicrobial susceptibility,and resistance genes in pregnant women
Fabrícia Almeida Fernandes Santana,Tais Viana Ledo de Oliveira,Marcelo Barreto de Souza Filho,Lucas Santana Coelho da Silva,Breno Bittencourt de Brito,Fabrício Freire de Melo,Cláudio Lima Souza,Lucas Miranda Marques,Márcio Vasconcelos Oliveira
Fabrícia Almeida Fernandes Santana,Tais Viana Ledo de Oliveira,Breno Bittencourt de Brito,Fabrício Freire de Melo,Cláudio Lima Souza,Lucas Miranda Marques,Márcio Vasconcelos Oliveira,Instituto Multidisciplinar em Saúde,Universidade Federal da Bahia,Vitória da Conquista 45029-094,Bahia,Brazil
Marcelo Barreto de Souza Filho,Laboratório Oliveira Ltda,LABO,Vitória da Conquista 45020740,Bahia,Brazil
Lucas Santana Coelho da Silva,Lucas Miranda Marques,Campus Soane Nazaré de Andrade,Universidade Estadual de Santa Cruz,Ilhéus 45662900,Bahia,Brazil
Abstract BACKGROUND Group B Streptococcus(GBS)is a normal component of the gastrointestinal and genital microbiota in humans and can lead to important infections in newborns.AIM To compare GBS isolation and identification methods as well as to assess the antibiotic susceptibility and to identify resistance genes in GBS strains from pregnant women attended in healthcare services from the city of Vitória da Conquista,in Bahia State,Brazil.METHODS From January 2017 to February 2018,vaginorectal swabs were obtained from 186 participants and the samples were seeded onto chromogenic agar for GBS before and after inoculation in selective broth.Confirmatory identification using 3 CAMP and latex tests was performed in samples with GBS-suggestive colonies.Then,disk diffusion antibiograms were performed in GBS-positive samples,and the detection of the resistance genes ermB,ermTR,mefA,and linB in the clindamycin and/or erythromycin-resistant samples was carried out.RESULTS Thirty-two samples(17.2%)were GBS-positive.The culture in chromogenic agar after sample incubation in selective broth was the most sensitive method(96.9%)for GBS detection.All isolates were susceptible to penicillin,ampicillin,cefotaxime,and vancomycin.Clindamycin resistance was observed in 6 samples(18.8%),while 8 samples(25%)were erythromycin-resistant.All erythromycin and/or clindamycin-resistant GBS strains had negative D-tests.Two strains(25%)presented an M phenotype and 6 isolates(75%)presented a cMLSB phenotype.The ermB gene was identified in 4 samples(44.4%),the mefA gene was also found in 4 samples(44.4%),the ermTR gene was identified in 1 isolate(11.1%),and the linB gene was not found in any isolate.CONCLUSION This study evidenced that the screening for SGB can be performed by means of various methods,including chromogenic media,and that the chemoprophylaxis for pregnant women who cannot use penicillin must be susceptibility-guided.
Key Words:Streptococcus agalactiae;Pregnancy;Antimicrobial susceptibility
INTRODUCTION
Streptococcus agalactiae(Group B Streptococcus GBS)is a bacterium that inhabits the gastrointestinal and genital tracts as a component of the normal human microbiota.Its clinical relevance is mainly due to infection in neonates.However,a growing number of GBS infections among non-pregnant adults has been reported[1,2].The presence of GBS colonization in pregnant women during childbirth represents the main risk for the development of infections(pneumonia,meningitis,and/or sepsis)in the newborn through vertical transmission from the colonized mother[3,4].
The estimated prevalence of GBS colonization in pregnant women is 10%-35% in various countries,including Brazil[1-3].In a recent systematic review,the average estimated prevalence was 20%,with the highest prevalence being reported in African countries.Nonetheless,there was a significant variation in the prevalence of maternal colonization that may be associated with factors that need to be further studied[5].
GBS vertical transmission occurs in approximately half of the newborns from colonized mothers,and,when antibiotic prophylaxis is not instituted,it is estimated that 1%-4% of neonates develop an early or a late GBS infection[6,7].The prevention of GBS infection includes identifying the colonized pregnant women by means of vaginorectal swab culture between 35thand 37thgestational weeks[3,8,9].
The vaginal/rectal secretions are inoculated in an antibiotic-supplemented,enriched,selective,Todd Hewitt broth and,then,cultivated in a 5% sheep blood agar[3,10].Other GBS isolation and identification methods include CAMP test,serogrouping,chromogenic media,and molecular tests[3].Each of them presents different sensitivity and specificity levels for GBS detection as well as distinct costs.
Penicillin is the drug of choice for prevention and treatment of GBS infection,and no bacterial resistance to that drug has been reported in this scenario[11,12].However,reduced penicillin susceptibility associated with penicillin-binding protein mutation was observed in some cases[13-15].Moreover,using erythromycin and clindamycin is indicated for penicillin-allergic pregnant women and,if bacterial resistance to these drugs occurs or there is a lack of information,vancomycin is chosen[12].In the last decades,a growing prevalence of erythromycin and clindamycin-resistant GBS strains has been observed(25%-32% and 13%-20%,respectively)[3,16-21].Such resistance is associated with the acquirement and expression of theermgenes,resulting in a MLSB phenotype that is related to the occurrence of erythromycin and clindamycin resistance.Furthermore,mefandmsrA genes confer erythromycin resistance and clindamycin susceptibility,characterizing an M phenotype(resistance to macrolides only).In its turn,linB gene,which is only linked to the clindamycin resistance,leads to an L phenotype(resistance to lincosamides only)[21,22].Moreover,the transfer of these genes between bacteria occurs by means of plasmids or transposons[12,16,18].
The clinical and epidemiological impacts of the GBS neonatal infections are significant and there is a tendency to an antimicrobial resistance rising that has already been shown in other Brazilian studies[23-28].Expanding the investigation of the antimicrobial resistance profile in more Brazilian cities can contribute for the better characterization of the prevalence and the susceptibility profile of the GBS as well as for the development of suitable guidelines in both national and regional scenarios.
Even though the local data do not directly influence the antibiotics choice since the international standards are taken into account for prevention and treatment of the GBS infection,such information may justify the implementation of GBS screening protocols in order to replace the risk-based chemoprophylaxis already adopted in some countries.That measure would reduce not only the local infant mortality,but also the costs related to the prolonged hospitalizations of GBS-infected newborns.
This study aimed to compare identification methods,to verify the susceptibility profile,and to determine the resistance genes of the GBS strains isolated from pregnant women in prenatal care in the basic health units from the county of Vitória da Conquista,in Bahia State,Brazil.
MATERIALS AND METHODS
Study design,period,region,and population
This cross-sectional study analyzed 186 vaginal and rectal secretion samples from pregnant women attended in nine Family Basic Health Unit of the county of Vitória da Conquista,in Bahia State,Brazil.The sampling was based on 5170 child-births occurred in the above-mentioned county in the year 2015 and on the GBS colonization prevalence(17%)described by the pilot study conducted by Oliveiraet al[29],with a 5%margin of error and a 95% confidence level.The sample collection was performed from January 2017 to February 2018.
Inclusion and exclusion criteria
Pregnant women with a 32-to-40 gestational age who lives in the urban area of the county were eligible,but the participants were excluded if they had used antibiotics in the last 7 d before collection.
Samples collection
The biologic samples were collected by means of the use of single vaginorectalswabswithout using speculum.The material was collected from the lower middle third region of the vagina and from perianal region,mandatorily.The samples were packaged inStuarttransport media and carried in specific boxes to the Clinical Analysis Laboratory of the Multidisciplinary institute of Health of the Federal University of Bahia within 8 h after the collection to perform the experiments.
Bacterial isolation and identification
The samples were seeded by depletion technique ontoStreptococcus chromIDTMStreptoB chromogenic medium,inoculated in Todd Hewitt broth(BIOMERIÉUX),and placed at a 35°C-37°C bacteriological incubator for 24 h.After,the samples were subcultured in chromogenic agar and kept in the incubator under the same above-mentioned conditions for 24 h.
All pink or red colonies(characteristic for GBS identification)underwent legitimized identification tests by means of CAMP test using the kit composed by Todd Hewitt agar and Hemolisinabac(PROBAC)and serogrouping using the SLIDEX®Strepto Plus B kit(BIOMERIÉUX)for species confirmation.
All serogrouping-confirmed isolates(gold standard method for GBS identification)were forwarded for antibiogram and an aliquot of each of them was cryopreserved at -20°C in a Brain Heart Infusion(BHI)broth with 15% glycerol.
Antimicrobial susceptibility testin g
All serogrouping-confirmed specimens underwent the disk diffusion antimicrobial susceptibility test(Kirby e Bauer)as recommended by theClinical and Laboratory Standards Institute[30].The tested antibiotics were penicillin(10 units),ampicillin(10 μg),cefotaxime(30 μg),erythromycin(15 μg),clindamycin(2 μg),and vancomycin(30 μg).They were chosen according the Clinical and Laboratory Standards Institute[30]and considering the drugs availability in the public health network of the studied county.
Determination of erythromycin resistance phenotypes
A D-test was performed for each erythromycin and/or claritromycin-resistant sample.Comercial Erythromycin(15 μg)and Clindamycin(2 μg)discs were placed 12 mm apart on Mueller Hinton agar plates supplemented with 5% blood and kept at a 35-37°C,5% CO2,incubator for 24 h with subsequent observation of the bacterial growth inhibition halo.The clindamycin and erythromycin resistances were considered indicators of constitutive MLSB phenotype(cMLSB).The reduction of the bacterial growth inhibition halo around the clindamycin disc in the region close to the erythromycin disc defined the inductive MLSB phenotype(iMLSB).Isolated sensitivity to clindamycin indicated the M phenotype and the sensitivity to erythromycin alone defined the L phenotype[21,22].
Determination of the resistance genetic profile
The presence of resistance genes in erythromycin and/or clindamycin resistant strains according to the phenotypic test was assessed by multiplex Polymerase Chain Reaction(PCR)technique.
The evaluated resistance genes wereermB,ermTR,andmefA,for erythromycin,andlinB for clindamycin,using specific primers(Table 1).The primers were synthesized and the reaction conditions were performed according described by Bolukaotoet al[21].The bacterial DNA for the PCR performing was extracted by boiling method[31].
The PCR results were analyzed according the presence or absence of bands in 2%agarose gel in 1x TAE buffer solution,stained with ethidium bromide and visualized on UV transilluminator after electrophoretic run.OneStreptococcus agalactiaereference strain was used as negative control.
Statistical analysis
The research database was made in Microsoft Office Exc el 2007 spreadsheets and the descriptive statistical tests were done with the EPI-INFO 3.5.1 version statistical package.In order to perform frequency comparisons,chi-square tests were performed with a 5% significance level.
Aiming the evaluation of the microbial identification tests,sensitivity,specificity,positive predictive value(PPV),and negative predictive value(NPV)were calculated,considering serogrouping as the gold standard[32].
Ethical considerations
The study was approved by the Ethical Committee of Research in Human Beings of the Multidisciplinary institute of Health - Campus Anísio Teixeira from the Federal University of Bahia(IMS-CAT/UFBA)under the protocol number 58104116.8.000.5556.
RESULTS
From the 186 analyzed samples,32 presented GBS strains according serogrouping,what represents a 17.2% colonization prevalence among the studied pregnant women.
Using the chromogenic medium(CRO1)without previously passing the sample through the Todd Hewitt medium,26 samples were positive for GBS colonies and one of them was not confirmed by serogrouping or CAMP test.When a previous sample passage through the Todd Hewitt medium was performed(CRO2),32 samples were GBS-positive and one of them was not confirmed by serogrouping.
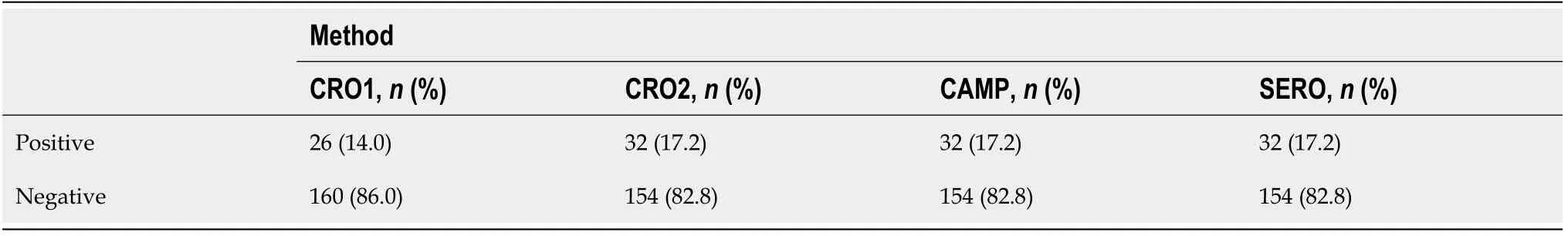
Table 1 Comparison between the isolation and identification methods used in vaginorectal secretions from pregnant women(n = 186)
Regarding the cross analysis between CRO1 and CRO2,one sample was GBSpositive only in CRO1,24 were positive in both,and 7 were positive only in CRO2.The sensitivity,specificity,positive predictive value(PPV),and negative predictive value(NPV)were calculated by means of the analysis of the CRO1,CRO2 and serogrouping results(CRO1 X CRO2/CRO1 X serogrouping/CRO2 X serogrouping).The GBS detection through CRO2 was the method that presented the best performance,with sensitivity(96.9%),PPV(96.9%),and NPV(99.3%)very close to those observed in serogrouping.
All the samples that were identified as positive for SBG after serogrouping underwent the antibiogram test.The susceptibility profile showed that all the GBS strains were susceptible to penicillin,ampicillin,cefotaxime,and vancomycin.Six(18.8%)GBS-positive strains were resistant to clindamycin and eight(25.0%)were resistant to erythromycin.
The erythromycin and/or clindamycin-resistant isolates(8)presented negative Dtests.Only 2 strains(25%)presented the M phenotype and 6 isolates(75%)presented the cMLSB phenotype.The Figure 1 shows the results of the 2% agarose gel electrophoresis performed from the GBS isolates that presented resistance to erythromycin and/or clindamycin in the phenotypic test,aiming genotypic evaluation by PCR.
In 4 isolates(44.4%),the resistance was associated withermB genes.ThemefA gene was present in 4 isolates(44.4%)and theermTR gene was detected in only one isolate(11.1%).In 7 isolates(87.5%),it was detected only one resistance gene(ermB,ermTR,ormefA).In one sample(12.5%),the presence of two resistance genes was verified(mefA+ermB).No strain carried thelinB gene.
In 4 isolates(44.4%),the resistance was associated withermB genes.Similarly,mefA gene was observed in 4 isolates(44.4%),while theermTR gene was found in a single isolate(11.1%).The detection of a single resistance gene(ermB orermTR ormefA)occurred in 7 isolates(87.5%).In a sample(12.5%),it was observed the presence of two resistance genes(mefA andermB).None of the strains hadlinB gene.
DISCUSSION
The GBS colonization prevalence of 17.2% found in this study is similar with those described by Oliveiraet al[29]and Borgeret al[33].That percentage is also befitting with the data from theCenter for Disease Control and Prevention(CDC)[3]that point towards a colonization prevalence from 10% to 30%.Moreover,the prevalence described in this study corroborates to the data observed in Taiwan[4](21.8%),Italy[16](25.5%),Ethiopia[17](19.0%),and Pakistan[34](17.0%).A recent systematic review estimated a world maternal colonization by GBS of 18% with regional variations from 11% to 35%[35].
Unfortunately,GBS screening of the pregnant women during prenatal evaluation is not performed in the studied county.In that context,the significant GBS prevalence observed in this study may contribute to the development of invasive infections by GBS in newborns,since CDC estimates that it occurs in about 1%-2% of newborns from colonized women[3].These data justify the adoption of a screening protocol for GBS by the health system from that county.

Figure 1 Electrophoresis in 2% agarose gel for erythromycin and clindamycin-resistant GBS isolates.Lines 1,2,3,and 6(samples 32,79,98,and 174,respectively):mefA gene presence(348 pb);Line 5(sample 136):ermTR gene presence(400 pb);Lines 1,4,7,and 8(samples 32,128,177,and 209,respectively):ermB gene presence(640 pb);Line 9:Negative control;Line 10:Molecular weight marker(100 kb).
According CDC recommendations,the GBS isolation and identification of GBS biologic samples should be performed in selective enrichment broths such as Todd Hewitt broth,followed by microbial cultivation in 5% sheep blood agar,presumptive identification by CAMP test,and confirmatory identification by serogrouping[3].Such recommendations are based on the assumption that the direct seeding of the vaginorectal sample onto any culture medium,without a previous passage in a selective enrichment broth,increases the chance of false-negative results.In addition,although the use of chromogenic media for GBS identification is mentioned by CDC,such an organization highlights that the available media were not able to identify nonhemolytic strains,which represent up to 4% of the GBS strains[3].Furthermore,it was demonstrated that non-hemolytic strains are associated with severe infections in newborns[36,37].However,the last CDC guidelines for the isolation and identification of GBS date back from 2010.Since then,chromogenic media that are able to detect hemolytic and non-hemolytic strains have emerged,including the ChromIDStrepto B(BIOMÉRIEUX)medium,which was used in this study.
Some studies had already demonstrated that the direct inoculation of vaginorectal samples onto chromogenic culture media is as sensitive as the method recommended by CDC[36-40].In our study,it was observed an important sensitivity difference between the GBS isolation and identification using direct seeding in chromogenic medium(78.1%)when compared to when that procedure is preceded by sample inoculation in selective media for GBS(96.9%).Regarding specificity,there was no difference,being that 96.3% for each of these methods.
In this study,32 samples were isolated/identified through CRO2 and,among them,only 1 was not confirmed by serogrouping.These data reveal that CRO2 presented a 96.9% sensitivity and a 99.3% specificity.Moreover,seven samples that were positive in serogrouping were not isolated/identified by CRO1,but only by CRO2.It shows that,besides a high sensitivity(96.9%),the high negative predictive value(99.3%)presented by CRO2 makes it stand out in this study as the best method for GBS colonization screening,since the minimization of false-negative results,which potentially lead to an increased risk of newborn infection by GBS,is one or the most important requirements for a screening protocol.
A previous research reported a 100% sensitivity for GBS detection through chromIDTMStrepto B(BIOMERIÉUX)media and a 79% sensitivity when blood agar was used,even after the enrichment in selective media[39].In our study,when the isolation/identification of GBS colonies in chromogenic media after the passage in Todd Hewitt broth is compared with the serogrouping results,a 96.9% agreement is observed.Although the chromogenic agar media manufacturers and CDC recommend the confirmation of the detection of GBS-suggestive colonies in chromogenic media by means of biochemical or immunological tests,the findings from this study as well as results obtained by previous researches,such as the one carried out by Moritaet al[39],suggest that the chromogenic media could be used without performing confirmatory tests.Furthermore,such method is considered an easy and fast diagnostic option that does not demand further technological sources,reducing test-related costs.Nowadays,besides the high detection rates,the chromogenic media provide other advantages such as the easy visualization of the colonies by means of colors,the detection of hemolytic and non-hemolytic strains,and the incubation in anaerobic environment[39].
In our investigation,the CAMP test showed 100% sensitivity in relation to serogrouping.However,that test should not be used as a confirmatory method for GBS identification,but only as a presumptive method,since the CAMP factor is not only found in GBS but also in other bacteria such as some streptococci of serogroups A,C,F,and G as well asListeria monocytogenesstrains[41].In addition,our study revealed that CAMP test should be performed in an extremely thorough way,using a standardStaphylococcus aureusstrain that has not been frozen for a long time,and the blood agar plates should be obtained commercially in order to reach a high accuracy.The use of commercial kits also does not seem to be advantageous because they present a short shelf life and,after the opening of the kit label,the hemolysin strips dry out quickly.
Besides the comparative study of the diagnostic methods,we evaluated the susceptibility profile of the GBS strains that are circulating in the county where this study was carried out.Such investigation is crucial to institute proper antimicrobial prophylaxis and to reduce the incidence of neonatal group B streptococcal disease.
The erythromycin(25%)and clindamycin(18.8%)resistance rates found in this study were lower than in some previous Brazilian studies but higher than in others such as those carried out by Meloet al[12],Dutraet al[25]and Borgeret al[33].The resistance rates for erythromycin and clindamycin in these studies were,respectively,8.1% and 5.9% in the first,4.1% and 3.0% in the second,and 9.4% and 6.2% in the third.When compared to the erythromycin and clindamycin resistance prevalence found by studies carried out in other countries,the prevalence showed by our results is also higher.In South Africa,Bolukaotoet al[21]found that erythromycin and clarithromycin resistance rates were 21.1% and 17.2%,respectively,while Mengistet al[17],in Ethiopia,found resistance rates of 6.5% for erythromycin and of 3.2% for clindamycin.Moreover,Frohlicheret al[20]observed resistance prevalence of 14.5% for erythromycin and of 8.2% for clindamycin in Switzerland,and Pinheiroet al[18]found resistance rates of 15% and 9.6% for erythromycin and clindamycin,respectively.These data suggest that the use of erythromycin and clindamycin as an alternative for penicillin-allergic pregnant women with high anaphylaxis risk should be accompanied by susceptibility tests for the choice of the proper therapy for each case.However,it is important to highlight that the cases of penicillin allergy are not frequent.
The rates of phenotypic and genotypic resistances found in this study influence the clinical management of the patients regarding the choice of the therapeutic scheme.Our results confirm that GBS isolates from the study population present macrolides resistance genes and,considering that these genes can be transferred from one bacterium to another,the monitoring of the GBS antimicrobial resistance should be performed regularly in penicillin-allergic patients.The high prevalence of antimicrobial-resistant GBS strains limit the therapeutic options for the antimicrobial prophylaxis and,increasingly,the use of broad-spectrum antibiotics have been necessary,which leads to a selective pressure over other microorganisms,contributing to the antimicrobial resistance growth[3,12,16,18,19,42].
Although most studies show that the GBS susceptibility to penicillin is uniform,its reduction had already been reported by some authors[14,15,43].In this study,we did not observe any GBS isolate that presented resistance or even a reduced sensitivity to penicillin.
The D-test results were negative in 100% of the isolated GBS strains that showed to be resistant to erythromycin.In other words,none of those strains presented an erythromycin-induced reduction of sensitivity to clindamycin.The resistance phenotypes observed in our study were cMLSB(75%)and M(25%).Similar studies carried out in Brazil by Dutraet al[25]and in Portugal by Pinheiroet al[18]also observed the iMLSB phenotype,besides cMLSB and M phenotypes.In its turn,the study by Bolukaotoet al[21]found four resistance phenotypes(cMLSB,iMLSB,M,and L).
ThemefA gene was detected by means of molecular test in the two samples that presented the M phenotype,corroborating with the data from the available literature,which indicate that themefA gene confer resistance only to macrolides[21].Moreover,5 samples presented the cMLSB phenotype had only theermB gene or theermTR gene,also being examples of concordance between the phenotypic and genotypic tests,since it is known that genes fromermfamily are associated with bacterial resistance to macrolides,lincosamides,and streptogramins B[21].ThemefA andermB genes were detected in one isolate that presented a cMLSB phenotype,suggesting the participation of two different genes in the promotion of the antimicrobial resistance.The finding of a cMLSB phenotype sample whose genotypic test only detected themefA gene,which confers resistance only to macrolides,show that the clindamycin resistance could be related to another gene that was not tested.The study by Dutraet al[25],which identified resistance genes of GBS strains in different Brazilian regions did not detect themefA gene,contrasting with our results.
CONCLUSION
This is the first study that compared the identification methods and evaluated the antimicrobial susceptibility profile of GBS strains in Vitória da Conquista,providing valuable information to the development of public health policies,including the elaboration of screening and antibiotic prophylaxis protocols against that microorganism.Subsequently,it would be possible to minimize the GBS transmission to newborns during the deliveries,which may contribute not only to the decrease of the child mortality but also to the reduction of the costs with prolonged hospitalizations of infected newborns.
ARTICLE HIGHLIGHTS
Research background
Streptococcus agalactiae(Group BStreptococcus,SGB)is a bacterium that inhabits the gastrointestinal and genital tracts of men and women as a component of their normal microbiota.The colonization of pregnant women by GBS in childbirth represents the main risk factor for the development of infections(pneumonia,meningitis,and sepsis)in newborns through a vertical transmission that occurs in approximately a half of the newborns from colonized mothers and,when antibiotic prophylaxis is not performed,about 1%-4% of the neonates develops an early or a late GBS infection.
Research motivation
The great importance of Group B streptococcal disease for clinical practice and health systems demands the expansion of the knowledge on GBS colonization detection methods and eradication regimens in order to aid in the development of health policies against that infection.
Research objectives
To compare the identification methods,to verify the sensitivity profile,and to determine resistance genes in the GBS strains isolated from pregnant women in prenatal care in basic health units from the county of Vitória da Conquista,in Bahia State,Brazil.
Research methods
This is a quantitative transversal study that analyzed 186 samples of vaginal and rectal secretions from pregnant women attended in nine basic health units from the county of Vitória da Conquista,in Bahia State,Brazil.Pregnant women with gestational ages from 32 to 40 wk were eligible for this study.The biologic samples were collected with a single vaginorectal swab without speculum use,seeded by depletion ontoStreptococcus chromIDTMStrepto B chromogenic media,inoculated in Todd Hewitt broth(BIOMERIÉUX),and placed at a bacteriological incubator under a 35°C-37°C temperature during 24 h.Subsequently,the Todd Hewitt broth samples were subcultured in chromogenic agar plates and kept in the incubator for other 24 h in the above-mentioned conditions.
All pink or red colonies(characteristics for GBS identification)underwent legitimate identification tests:CAMP test using the KIT composed by Todd Hewitt agar and Hemolisinabac(PROBAC DO BRASIL)and serogrouping using the SLIDEX®Strepto Plus B KIT(BIOMERIÉUX)for species confirmation.
All serogrouping-confirmed isolates(gold standard method for GBS identification)were forwarded for antibiogram performing by means of the disk-diffusion technique(Kirby and Bauer),following the Clinical and Laboratory Standards Institute recommendations,and an aliquot was preserved at -20°C in a 15% glycerol brain-heart infusion broth for resistance genes investigation in erythromycin- and/or clindamycin-resistant strains through multiplex Polymerase Reaction Chain.
Research results
One hundred and eighty-six samples were analyzed by this study,and GBS strains were identified in 32 of them,representing a 17.2% prevalence among the included pregnant women.The GBS detection after subculturing in Todd Hewitt broth presented the higher sensitivity(96.9%).In six GBS isolates(18.8%),it was verified a clindamycin resistance,and eight isolates(25.0%)presented erythromycin resistance.The resistance was associated withermB genes in 4 isolates.ThemefA gene was detected in 4 strains and theermTR gene was found in a single strain.In seven isolates,it was detected only one resistance gene(ermB orermTR ormefA).One strain had two resistance genes(mefA+ermB).
Research conclusions
For the first time,we compared identification methods and analyzed the antimicrobial susceptibility profile of GBS strains in the above-mentioned county.The data from this study may be useful in the development of future screening and antibiotic prophylaxis protocols aiming the prevention of GBS neonatal infection.
Research perspectives
The information provided by this study is applicable for the elaboration of GBS colonization screening and eradication strategies.Therefore,this study potentially contributed to the reduction of children morbidity and mortality as well as to the decrease of health system costs with the hospitalization of neonates.
 World Journal of Clinical Cases2020年18期
World Journal of Clinical Cases2020年18期
- World Journal of Clinical Cases的其它文章
- Special features of SARS-CoV-2 in daily practice
- Gastrointestinal insights during the COVID-19 epidemic
- From infections to autoimmunity:Diagnostic challenges in common variable immunodeficiency
- One disease,many faces-typical and atypical presentations of SARS-CoV-2 infection-related COVID-19 disease
- Application of artificial neural networks in detection and diagnosis of gastrointestinal and liver tumors
- Hepatic epithelioid hemangioendothelioma:Update on diagnosis and therapy
