From infections to autoimmunity:Diagnostic challenges in common variable immunodeficiency
Ewa Więsik-Szewczyk,Karina Jahnz-Różyk
Ewa Więsik-Szewczyk,Karina Jahnz-Różyk,Department of Internal Medicine,Pulmonology,Allergy and Clinical Immunology,Central Clinical Hospital of the Ministry of National Defense,Military Institute of Medicine,Warsaw 04-141,Poland
Abstract Common variable immunodeficiency(CVID)is the most common clinically significant primary antibody deficiency diagnosed in adults.The early symptoms are not specific.They include common infections,mainly of the respiratory tract,caused by typical microorganisms,so cases can be missed in primary care.In the majority of patients increased susceptibility to infections coexists with signs or symptoms of autoimmunity,inflammation or polyclonal lymphoproliferation,which can divert diagnosis from immune deficiency.The overall incidence of malignancy is increased in CVID and certain cancers are significantly more common.Lymphomas and gastric carcinoma are the most frequently reported malignancies in CVID,so a high index of suspicion is recommended.Diagnostic delay in CVID is seen worldwide.The main goal of this paper is to increase the awareness about CVID among health care professionals.We aim to present features which can be helpful in CVID diagnosis in order to shorten the “latency”of proper management of CVID patients.We review clinical symptoms,complications and laboratory abnormalities of CVID.Immunoglobulin replacement therapy is regarded as the cornerstone of pharmacological intervention.New modes of Ig application,mainly subcutaneously and via the hyaluronidase-facilitated subcutaneous route,help to adjust therapy to patients’needs and preferences.Still there remain unmet needs.It remains to be seen whether CVID complications can be avoided by earlier diagnosis,treatment and thorough monitoring in the context of increased risk of malignancy.Development of patient tailored protocols depending on the clinical phenotype and risk factors might be more appropriate.The most important consideration is to diagnose suspected cases and stratify patients in a precise and timely way.Work is needed to define features predictive of unfavorable prognosis.
Key Words:Primary antibody deficiency;Recurrent respiratory tract infections;Complications;Immunoglobulin replacement;Adults;Early diagnosis
INTRODUCTION
Primary immunodeficiencies(PID)are rare diseases.More than half of PID cases are associated with a defect in antibody production or function[1].In this group,the most common clinically significant deficiency is common variable immunodeficiency(CVID).Although CVID is innate condition,the peak of disease onset occurs at the age of 20-40,and the condition can be diagnosed even in elderly patients[2].Early symptoms are not specific.They include common infections,mainly of the respiratory tract,caused by typical microorganisms,so cases can be missed in primary care.In a significant percentage of patients increased susceptibility to infections coexists with signs or symptoms of autoimmunity or polyclonal lymphoproliferation,which seems to be a paradox.Patients with CVID are consulted by doctors specializing in various areas - hematology,rheumatology,gastroenterology for specific symptoms while the common denominator,immunodeficiency and hypogammaglobulinemia,is overlooked.Indeed,diagnostic delay is seen worldwide[3].The delay in diagnosis can lead to organ damage,in particular bronchiectases.In long term follow-up malignancy is also more common among patients with CVID in comparison with healthy population.Unrecognized CVID generates high economical cost[4].
The main goal of this paper is to increase the awareness about CVID among health care professionals.We aim to present features which can be helpful in CVID diagnosis in order to shorten the “latency” of proper management of CVID patients.
EPIDEMIOLOGY AND DEMOGRAPHY
CVID prevalence ranges from 2/100000 to the highest reported prevalence for Finland- 6.9/100000[5].The median age at which the first symptoms occurred in a case series of Polish patients is 24 years[6],in Italy and Denmark 32 and 29 years[7],respectively,while in the 2018 European Society of Immune Deficiencies(ESID)registry the figure is 18 years[3].A recent study from the United States reported 24 and 28 years as the median age of onset for females and males,respectively[8].Some studies report bimodal age distribution[6,9]where others,reported linear distribution,with decline after the age of 80[10].In Germany,the highest percentage of patients experience the first symptoms of CVID between 1 and 5 years,followed by a markedly lower peak incidence at the age of 16-20 years[11].Current data indicate that the majority of patients are diagnosed in adulthood(age ≥ 18)comprising between 65% and nearly 90% in reported cohorts.The significant variations in epidemiology and demographic data are related to differences between cohorts surveyed,especially with regard to the proportion of adult to pediatric patients,as well as diagnostic criteria used,which are discussed below.From 2012,when new PID ESID criteria were proposed,professionals tend to identify more cases of late-onset combined immune deficiencies in adults[12].
The literature informs of a long delay in diagnosing CVID.In a recent report,the overall delay was 5 years in Europe and remained constant over the last 20 years[3].A Danish cohort had a mean diagnostic delay of 7 years[7]and in an Italian one,the figure was 8.9 years[13].The longest diagnostic delay of 10.13 years was reported for adult patients with CVID in Poland[14].However it was significantly shorter in patients diagnosed before age 18:5.22 years compared to 11.63 years for patients diagnosed in adulthood(age ≥ 18),despite similar clinical phenotypes in children and adults[14].At present,in Poland,CVID diagnosis is more rapid than that before 2000[6].However,there remains a low percentage of patients whose diagnosis was established within a year of occurrence of the first symptoms[6].According to the 2014 ESID registry,a significant shortening of the median delay was achieved only in Spain(9.0vs4.6 years)[2].There is a need for further research on the relationship between delayed diagnosis and occurrence of complications.It is difficult to compare data coming from different countries and studies,due to different methodology applied for analysis.In our experience,a significant increase in number of diagnosed CVID cases occurred when reimbursement of subcutaneous immunoglobulin treatment for adult patients with primary immunodeficiency was provided and specialized immunology centers established[6,14].
Taken together,these data suggest that the level of awareness and suspicion of CVID as a differential diagnosis remains poor.
CLINICAL FEATURES
Infections
The hallmark of CVID is susceptibility to infections which affect 99 to 70 per cent of patients.Infections are the leading cause of mortality among patients with primary antibody deficiencies in the United States of America[15].The reported etiologies of recurrent respiratory tract infections include common bacteria:Streptococcus pneumoniae,Hemophilus influenzae,Moraxella catarrhalis,Mycoplasma pneumoniae,Chlamydophila pneumoniae and Staphylococcus aureus[16].Common sites of infection include paranasal sinuses,middle ear,bronchi and lungs.Gastritis and enterocolitis are less common.The typical causative agents in the alimentary tract are:Giardia lamblia,Campylobacter jejuni,Salmonella enteritidis but some atypical pathogens can be identified,for example:Campylobacter pylori and Aeromonas hydrophila.The differential work-up of enterocolitis must also include viral etiology,including norovirus,which is spontaneously eliminated by immunocompetent persons[17].Cytomegalovirus(CMV)has been found in gut biopsies of CVID patients[18].CMV enteritis in CVID can lead to severe malabsorption and irreversible chronic damage of the gastro-intestinal tract,which can require parenteral nutritional support[19].
In contrast to high risk of common bacterial infections patients with CVID do not present an increased susceptibility to influenza infection.Moreover most of them have preserved antigen specific T cell responses after influenza vaccination[20].Data about the clinical course of coronavirus disease 2019(COVID-19)in patients with primary immunodeficiency remains limited.The first,published case series included 5 patients with CVID and 2 patients with agammaglobulinemia[21].Patients with CVID presented with a severe form of COVID-19 infection.They required multiple drug treatment,including antiretroviral agents,IL-6 blocking drugs,and mechanical ventilation.In contrast two patients with agammaglobulinemia and absent B cells,had mild symptoms.Authors speculate that strikingly different clinical course of COVID 19 might be explained by a possible role of B lymphocytes in the severe acute respiratory syndrome coronavirus 2 induced inflammation,assuming that patients with agammaglobulinemia lack B lymphocytes whereas patients with CVID have dysfunctional B lymphocytes[21].
If patients remain untreated,they suffer an increase of frequency and severity of infections with increasing duration of CVID.Patients often require hospitalization and intravenous antibiotics.Bronchiectases are a long-term sequel of recurrent lung infections in CVID[22].Still a significant percentage of patients are diagnosed when bronchiectases are already present[23].
Sepsis is a relatively rare complication of CVID[14].Opportunistic infections are more characteristic for combined B and T cell immunodeficiencies than for CVID[12].Cumulative incidence of opportunistic infections in CVID is reported between 5.4%and 9.2%,and Pneumocystis jirovecii,varicella zoster virus,Mycobacterium species(spp.),Aspergillusspp.,Toxoplasma gondii,andCandidaspp.are the most common pathogens[24].In our CVID cohort we found 1 opportunistic infection and 1 infection caused by an unusual pathogen[14].The former case was a severe pneumonia caused by Aspergillus spp.and the latter,a sepsis due to an atypical pathogen:Achromobacter denitrificans.Both patients initially were missed as CVID cases and underwent immunosuppressive treatment for their presenting conditions.The first patient received biological and conventional diseases modifying anti-rheumatic drugs due to psoriatic arthritis[25].The second patient was treated with mycophenolate mofetil due to retinitis with granulomas[26].It has been found that the risk of opportunistic infections in CVID patients increases with secondary comorbidities and their management[24].
Microbiological assessment is a crucial element of the diagnostic work-up of patients with CVID.It should be emphasized that in patients with hypogammaglobulinemia and those treated with polyclonal immunoglobulin G(IgG)products,serological tests based on determination of antibodies in IgG class are unreliable.It is therefore obligatory to collect appropriate cultures or perform polymerase chain reaction assays in search of the infectious agent.
Non-infectious complications
The clinical picture of CVID is typically composed of multiple non-infectious pathologies.A non-complicated phenotype,limited to infections,is reported in only up to 30% of patients[8,14].Non-infectious pathologies involve autoimmune complications,both organ-specific and general,lymphoid hyperplasia,granulomas and malignancy.In long term follow-up,68% of patients had at least 2 complications[8].These non-infectious complications can precede recurrent infections and be the first presentation of immune dysregulation in CVID[27,28].They can also appear simultaneously with infections or later,during follow up.According to published studies,disease complications had a negative impact on patient survival[10,29,30].Resnicket al[29]estimated the risk of death to be 11 times higher in complicatedvsnon-complicated CVID.
Autoimmunity:According to reports,autoimmune diseases occur in up to 30% of CVID cohorts.In a recent study focused on noninfectious CVID complications,among 632 patients followed since 1974,autoimmune thrombocytopenic purpura(AITP)was the most common(16.2%),followed by autoimmune hemolytic anemia(AIH 7.7%).Other associated autoimmune conditions include rheumatoid arthritis(2.7%)and uveitis(1%).Rarer autoimmune complications are psoriasis,psoriatic arthritis,vitiligo,alopecia,autoimmune thyroiditis,antiphospholipid syndrome,Sjogren syndrome,vasculitis,type 1 diabetes,myasthenia gravis,autoimmune pancreatitis,severe oral ulcers[8,10,14].In one,although small,series of CVID patients the median age of AITP diagnosis was 23 years,while of CVID was 27 years.CVID was diagnosed before AITP in only 19% of patients[28].It is recommended to assess IgG level in patients with autoimmune cytopenia.
Gastrointestinal involvement:Gastrointestinal(GI)pathologies in CVID may involve any part of the gastrointestinal tract.They affect from 5% to 20% of patients in published cohort studies[8,14].Gastrointestinal symptoms are difficult to differentiate from signs of inflammation due to infectious or non-infectious etiology(colitis-like or celiac-like disease),all the more so since both conditions can coexist.
Non-infectious background of GI symptoms should be searched for after infectious etiology is excluded.The main symptoms are bloating,pain,chronic diarrhea(lasting more than 2 wk)and malabsorption.Comprehensive biopsies revealed lymphocytosis,villous atrophy/blunting,nodular lymphoid hyperplasia,granulomas and nonspecific inflammation.If CVID presents with gastrointestinal symptoms,the case is commonly misdiagnosed as celiac disease.The features,which support differential CVID diagnosis,are absence of plasma cells in the histological assessment,negative celiac genetic testing and lack of response to gluten-free diet[31].Another diagnostic pitfall is inflammatory bowel disease.Current data highlights the relevance of the endoscopic and histological assessment in CVID patients presenting with chronic diarrhea.The vigilance towards CVID in patients with enterocolitis and recurrent infections is recommended[32]and immunology centers should agree on a protocol with the local gastroenterology team to guide observations and indicate the pathological samples to be taken at endoscopy in adults with CVID[33].
Polyclonal lymphoid infiltration:Polyclonal lymphadenopathy occurred in 20% to 40% of patients[8].Clinically,this often presents as generalized lymphadenopathy and splenomegaly.The challenge is to differentiate it from lymphoma.Diagnostic excision of a whole lymph node is recommended.Lymph nodes show atypical lymphoid hyperplasia,reactive lymphoid hyperplasia or granulomatous inflammation[16].In our experience,we have to repeat histologic evaluation serially in one patient.
Granulomas are less common,but can be located in any organ and may lead to irreversible damage.Granulomas in lungs,liver,skin or eyes can be diagnosed as sarcoidosis[34].This highlights the need to include serum main immunoglobulin assessment in a work-up of patients with sarcoidosis.In a subset of patients,lung granulomas can also be accompanied by an intense lymphocytic infiltration;a condition described as granulomatous lymphocytic interstitial lung disease(GLILD)[35,36].According to the definition proposed by British Lung Foundation/United Kingdom Primary Immunodeficiency Network,GLILD is a distinct clinicoradio-pathological interstitial lung disease(ILD)occurring in patients with CVID,associated with lymphocytic infiltration and/or granuloma of the lung,and in whom other conditions had been considered and,where possible,excluded[37].
Clinically,patients with GLILD experience new or worsening,often productive cough,exertional dyspnea and fatigue.On physical examination,inspiratory crackles are present in 50% of patients[34].There is universal agreement for full lung function assessment(spirometry,lung volumes,gas exchange)[37].In one study including 20 patients with confirmed histopathological GLILD,a restrictive ventilatory defect(total lung capacity < 80% predicted)was found in 33.3% patients and an obstructive defect(forced expiratory volume in 1 s/vital capacity < 70%)in 10 % of patients while an impairment of carbon monoxide diffusing capacity(DLCO <80%)was observed in 70% patients[34].
Chest computerized tomography(CT)is an essential diagnostic step,where discovery of new abnormalities,which closely correlate with clinical signs and symptoms,is very suggestive.If conventional CT images are stable,but the patient’s condition deteriorates,positron emission tomography(PET)can add value[38].The most common CT finding in GLILD was nodules,often multiple with air bronchograms and smooth margins possibly surrounded by ground-glass opacities(halo sign).In one study,micronodules were present in 60% of patients,had a random distribution in 64% cases and were perilymphatic in 36% cases.Neither the hallmarks nor their constellation seems to be sufficiently specific to establish diagnosis[38-40].
A recommended approach is to confirm the diagnosis of GLILD at surgical lung biopsy[41],but this is not always available[23].Diagnosis has to be established by a histopathologist experienced in PID in cooperation with a clinician.The presence of granulomatous inflammation,peribronchiolar lymphoid proliferation,interstitial lymphoid proliferation,and CD4-cell predominance are described,but this is not a universal phenomenon[41].Flexible bronchoscopy helps to exclude infection[37].The extent of microbiological work-up differs among centers.Recommended essential tests are microscopy and culture,Mycobacterial culture,fungal culture.There is some debate about PCR forMycobacteria,atypical bacteria,respiratory viruses,Pneumocystis jirovecii and these should be assessed in selected cases[37].Some studies indicate that bronchoalveolar lavage can be helpful in assessing GLILD activity and selecting possible treatment.There is some evidence that lymphocytes exceeding 20% of cell counts in BAL material correlate with GLILD diagnosis.There is also growing evidence that GLILD,lymphadenopathy,splenomegaly,hepatomegaly and chronic diarrhea are seen together and that they share common pathology[42,43].
Up to now the cause and exact significance of this interstitial lung disease is poorly understood and its management is a challenge in clinical practice.Center experiences vary and even the natural history of GLILD is not well described.Patients are often put on corticosteroids with other immunosuppressive therapies and rituximab as a second line treatment[35,44].The STILPAD study is a multi-center observational study looking at the effect of various treatments on interstitial lung disease(ILD)in patients with CVID and ILD that had been diagnosed by a chest CT scan[45].In selected patients,there may be a role for FDG PET-CT imaging in view of the sensitivity of combined anatomical and functional information obtained,but more data are needed to endorse this modality.
Malignancy:The overall incidence of malignancy is increased in CVID and certain cancers are significantly more common.Lymphomas are the most frequently reported malignancies in CVID[46,47].The majority of lymphomas are of the B cell non-Hodgkin’s type(90%)[8].Childhood onset and previous polyclonal lymphoproliferation are predictors identified for lymphomas[10].Gastric carcinoma is common as well.In a Scandinavian study,the observed to expected ratio for stomach cancer was 10:3[48].In an Australian study a standardized incidence ratio for gastric carcinoma was 7.3[49].Standardized mortality ratio indicated a 10.1-fold excess mortality among CVID patients with gastric cancer[50].A gastric screening protocol was proposed[51].This is to include a gastroscopy in individuals with CVID with any of the following risk factors:Age greater than 50,CVID diagnosis since more than 10 years,significant smoking history,family history of gastric carcinoma,persistent diarrhea or upper gastrointestinal symptoms,previous gastroscopy with inadequate biopsies,positiveHelicobacter pyloribreath test,iron deficiency,and low serum vitamin B12.As CVID patients also have an increased risk of gastrointestinal lymphoma,it seems reasonable to perform multiple biopsies from the gastric antrum and body and additionally from the second part of the duodenum.It is reported that fewer biopsies decreased the probability of detecting early premalignant lesions[51].Dhallaet al[52]suggested to perform upper endoscopy with an interval between the subsequent endoscopic assessment based on histological findings:Every 1-3 years in patients with metaplasia,every 3 years in patients with atrophic gastritis,and every 6-12 mo in those with dysplasia.However,some CVID patients developed a high-grade gastric cancer 12-14 mo after an endoscopy that had shown no histologic signs of dysplasia.Based on this data a yearly evaluation for stomach cancer in all CVID patients might be beneficial[50,53].Development of further guideline/consensus on screening and monitoring for gastric cancer and lymphomas is required.
Other malignancies occurred in patients diagnosed in adulthood and according to published data are more likely to develop in the fifth and sixth decade[54].Examples are pituitary gland adenoma,colon tubular adenocarcinoma,squamous cell carcinoma(lungs),basal cell carcinoma,intestinal tubular adenoma(low grade),breast adenocarcinoma,metaplasia of the cervix[14].
CLINICAL PHENOTYPES
The literature defines five clinical phenotypic categories:Autoimmunity(including organ-specific autoimmune conditions and cytopenia);polyclonal lymphocytic infiltration(including unexplained granuloma,unexplained hepatomegaly,persistent lymphadenopathy,and lymphoid interstitial pneumonia);lymphoid malignancy(proven and treated);unexplained enteropathy(biopsy-proven and gluteninsensitive);and no disease-related complications[10].
LABORATORY MANIFESTATIONS
Despite the heterogeneity of CVID,low IgG levels are found in most patients.At diagnosis,only a minority of patients had IgG ≥ 500 mg/dL,a significant percentage had less than 100 mg/dL and up to 20% had undetectable IgG,IgA and IgM[14,55].As normal IgG and IgA levels exclude CVID,quantification of serum Ig levels is a useful initial laboratory test[14,55].Protein electrophoresis can draw attention to a low gamma fraction.
Immunoglobulin levels are not always available for primary care.Calculated globulin(CG)can be an alternative option.CG is the difference between total protein and albumin levels.If a CG result is ≤ 17 g/L,the probability of hypogammaglobulinemia increases[56-58]and the patient is suitable for further immunologic evaluation.
Specific antibody production and isohemaglutinins
Specific antibody production reveals a function of adaptive immunology.It is impaired in the majority of CVID patients.
Currently,the measurement of specific antibody responses varies across countries.It should include evaluation of both T-dependent responses(to protein or glycoprotein antigens)and T-independent responses(to polysaccharide antigens).The procedure involves two steps.First,an initial protective antibody assay is done.If the titer is low,immunization is performed,and a second measurement of protective antibody titer made after 3-6 wk(optimal at 4 wk).Diphtheria and tetanus toxoid vaccines are the most commonly used vaccines to evaluate T-cell dependent responses.Specific antibody T independent responses are mostly measured after vaccination of PPV23(referred to as test immunization).The vaccination response in adults is satisfactory if at least 70% of the measured serotype-specific antibody titers are above 1.3 μg/mL or a four-fold increase of the pre-vaccination titers for more than 17 of 23 serotypes is observed at week 4 after immunization[59].An alternative to PPV is the measurement of response after immunization against Salmonella typhi[60,61].Isohemagglutinins are naturally occurring antibodies of IgM and IgG isotypes to polysaccharide blood group antigens.Isohemagglutinins may be an alternative,clinically relevant,and easily accessible analysis to assess T-independent antibody function in patients with a group other than AB[55].
Lymphocyte subsets
CVID is a primary antibody defect,so naturally attention is focused on B lymphocyte analysis.Immunophenotyping of the B cell compartment is a routine evaluation of patients with CVID.Low Ig switched memory B-cell(smB)(CD19+CD27+IgM-IgD-)is an abnormality present in 80% of patients,however it is not specific for CVID[57].Other B lymphocyte subsets are highly variable.Findings can be classified according several systems,of which two are the most popular:Freiburg[62]and EUROclass[63].Both strategies apply characterization of CD19+ B cell subsets.Low Ig sm B-cell(smB)proportions and abnormally high proportions of B cells with reduced CD21 expression(CD21lowB cells)help to distinguish subsets.In addition to these two cell subsets,the EUROclass classification also uses abnormal expansion of transitional B cells(CD19+CD27-CD38+)for further subgrouping.
Multiple studies have demonstrated disturbances in T and natural killer(NK)cell homeostasis.Decreased circulating NK cell numbers in CVID patients were found to be associated with severe bacterial infections and granulomas[64,65].T cells play a central role in B cell activation and differentiation into memory and IgG producing B cells.Various reports have associated CVID with other findings,such as CD4 T-cell lymphopenia with reduced counts of naive CD4 T cells[66]and naive CD8mT-cell[67].Regulatory T cells(Treg),Th17,and follicular T helper(Tfh17)cells were specifically reduced in patients with complicated CVID phenotypes[68].T cells in CVID have lower proliferative capacities[69]and abnormal cytokine production[70].Low(naïve)CD4 T cells are associated with complications and a poor prognosis in CVID[71].Recent publications show an involvement of follicular T cells in CVID pathogenesis[72].An increase of circulating memory CXCR5+CD4 T cells in CVID patients with noninfectious complications has been reported[73].Follicular T helper cells could participate in autoimmune manifestations through their role as B cell inducers.As a consequence patients with CVID and autoimmune phenomena exhibit hyperplastic however insufficient germinal center(GC)response.An enrichment of T cells in lymph nodes of patients with CVID with lymphadenopathy and preserved ability to form GCs has been found[74].Taken together these data suggest that some distinct pathophysiological alterations are present in a defined subgroup of CVID patients.Work has also been done to better understand correlations between B cell and T cell abnormalities with unique clinical profiles and to use them as a prognostic marker[68,75].
Real life data revealed that full diagnostic work-up is not always performed.Gaps in laboratory testing were identified.A minority of CVID patients(20%)had been assessed for response to vaccination[7,14].Problems that need to be solved include test standardization,lack of polysaccharide pneumococcal vaccine on the market,and lack of reimbursement of vaccines for adult patients,challenges in the interpretation of results.Of all reported patients in a Danish cohort 21% had isohemagglutinin titers measured and only 17.9% were characterized by flow cytometric B cell phenotyping[7].
Genetics
CVID is a sporadic disease,polygenic in nature.A genome-wide association study identified multiple loci with potential susceptibility for CVID,however their significance in clinical practice is unclear.Currently molecular genetic analysis of patients is not a requirement for the diagnosis[55].However,pathogenic monogenic variants are found in 2%-30% of screened CVID populations,depending of applied clinical criteria,frequency of parents consanguinity,proportion of familial cases and genetics methods used.Whole exome sequencing(WES)is an effective tool for the discovery of genetic defects in patients with primary immunodeficiencies(PIDs).In 2016 WES was performed on 50 subjects diagnosed with CVID[76].Subjects selected for analysis had at least one of the following:Early-onset of manifestations(under age 10)(36%),autoimmune/inflammatory manifestations(76%),low B lymphocyte counts(58%),and/or familial history of hypogammaglobulinemia(16%).With this approach 17 probable disease-causing mutations in 15 patients(30%)were identified.There were mutations inNFKB1,STAT3,CTLA4,PIK3CD,andIKZF1,and biallelic mutations inLRBAandSTXBP2.This suggests that WES may be useful in selected CVID phenotypes.It remains to be seen whether this approach generates change is management and will be beneficial in daily practice[77].
DIAGNOSIS
There is an ongoing debate about criteria for diagnosis of CVID[78].First were proposed by European Society of Immune Deficiencies(ESID)/ Pan-American Group for Immune Deficiency in 1999[79].Ameratunga in 2013[80],ESID in 2014[12]and International Consensus Document in 2016[55]proposed new criteria(Table 1).They include features and laboratory parameters which illustrates progress of knowledge and understanding in the pathogenesis of CVID.All criteria may be applied only if secondary causes of hypogammaglobulinemia have been excluded[81].Particular domains,features or parameters of diagnostic criteria must be applied sequentially as none is specific individually.Each definition has limitations which are analyzed in a review paper by Ameratungaet al[78].In our center we use ESID criteria[12].We believe that they are helpful for early diagnosis.In our practice they have a good discriminative value for exclusion of subjects with undifferentiated hypogammaglobulinemia.However ESID criteria are not recommended as an unique criterion for decision of initiation an Ig replacement therapy[12,80,82].
CONCLUSION
CVID is heterogenous disease.An early and proper diagnosis of CVID is a challenge in everyday practice.It is recognized that early correct diagnosis avoids unnecessary diagnostic procedures and wrong treatments.In the last decade data from published registries and national cohorts of CVID patients increased our knowledge about CVID’s natural history and the complexity of its clinical picture,beyond increased susceptibility to infections.Majority of patients have at least one non-infectious manifestation,such as autoimmunization,granulomatous lesions,unexplained polyclonal lymphoproliferation,enteropathy,or malignancy.Immunoglobulin replacement therapy is regarded as the cornerstone of pharmacological intervention.New modes of Ig application,mainly subcutaneously andviathe hyaluronidasefacilitated subcutaneous route,help to adjust therapy to patients’ need and preferences[83,84].Still there remain unmet needs.It remains to be seen whether CVID complications can be avoided by earlier diagnosis,treatment and thorough monitoring in context of increased risk of malignancy.Development of patient tailored protocols depending on the clinical phenotype and risk factors might be more appropriate.In our opinion,from a practical point of view,the most important consideration is to diagnose and stratify patients as precisely as possible from the moment of diagnosis.Predictive features which help identifying a subgroup of patients with unfavorable prognosis are needed.
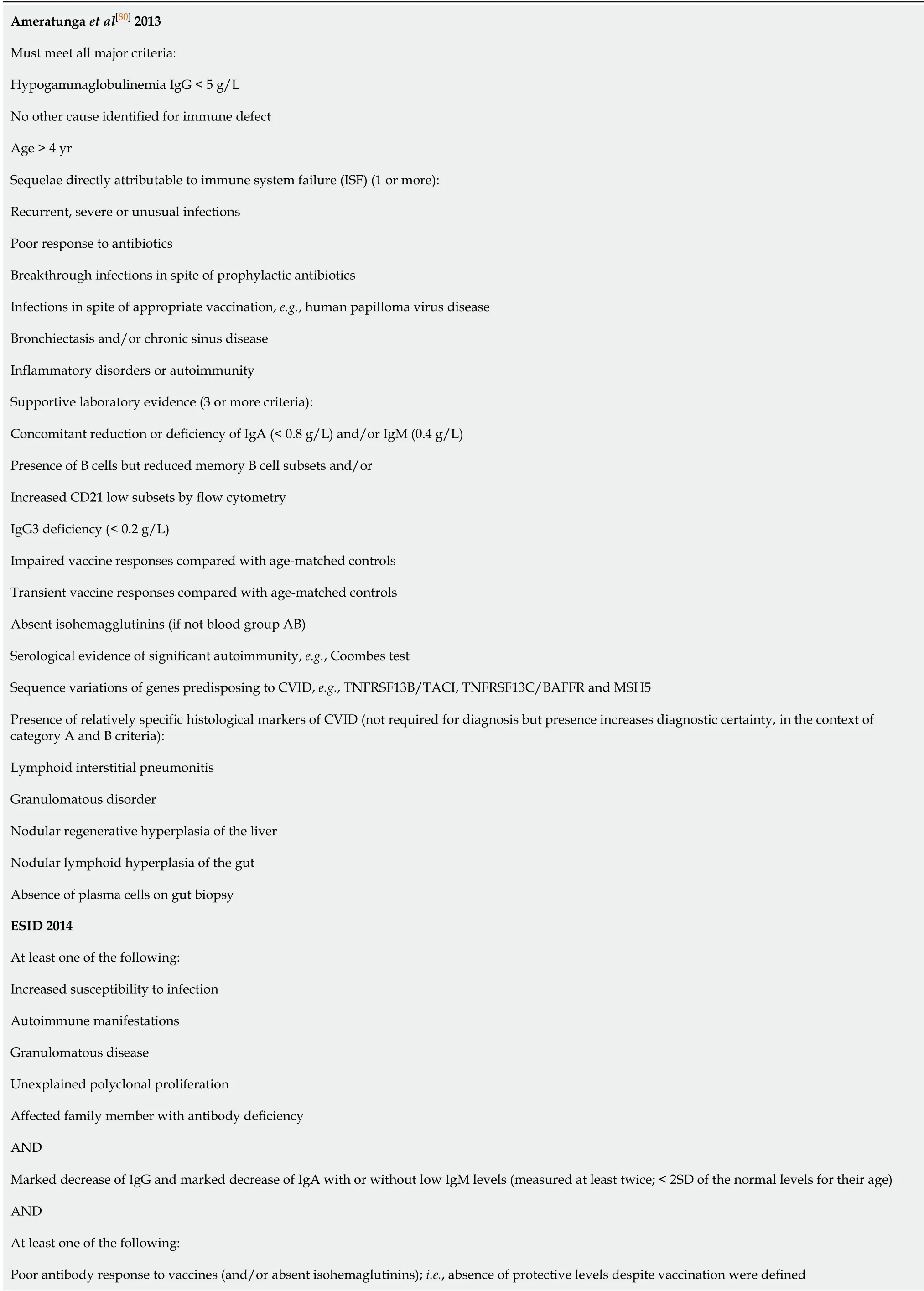
Table 1 Definitions of common variable immunodeficiency proposed by Ameratunga et al[80],European Society of Immune Deficiencies[12] and International Consensus Document[55]
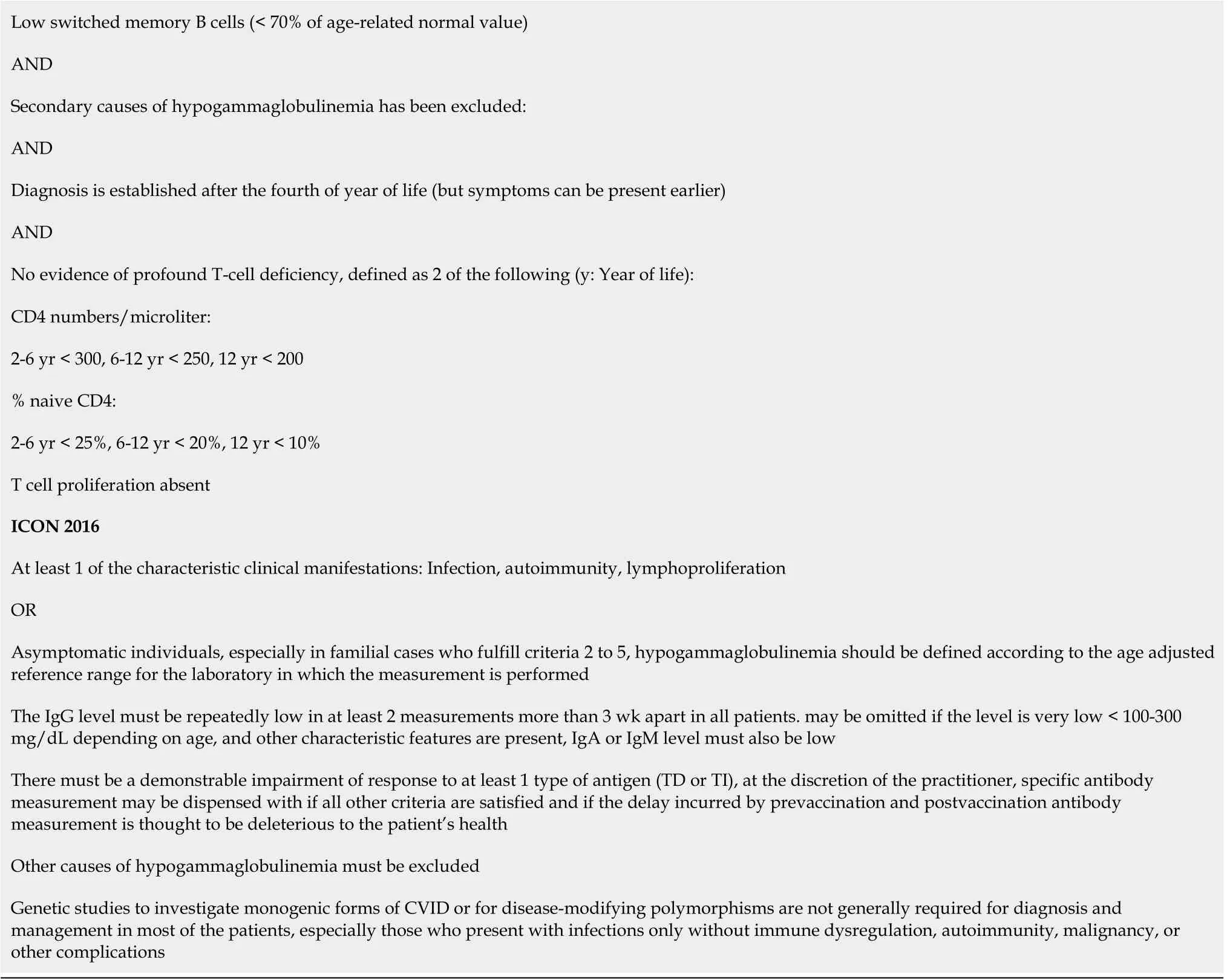
CVID:Common variable immunodeficiency;ESID:European Society of Immune Deficiencies;ICON:International consensus document.
 World Journal of Clinical Cases2020年18期
World Journal of Clinical Cases2020年18期
- World Journal of Clinical Cases的其它文章
- Special features of SARS-CoV-2 in daily practice
- Gastrointestinal insights during the COVID-19 epidemic
- One disease,many faces-typical and atypical presentations of SARS-CoV-2 infection-related COVID-19 disease
- Application of artificial neural networks in detection and diagnosis of gastrointestinal and liver tumors
- Hepatic epithelioid hemangioendothelioma:Update on diagnosis and therapy
- Streptococcus agalactiae:Identification methods,antimicrobial susceptibility,and resistance genes in pregnant women
