Endoscopic fenestration in the diagnosis and treatment of delayed anastomotic submucosal abscess: A case report and review of literature
Bao-Zhen Zhang, Yi-Dan Wang, Ye Liao, Jing-Jing Zhang, Yu-Fan Wu, Xiao-Lin Sun, Si-Yu Sun, Jin-Tao Guo
Bao-Zhen Zhang, Yi-Dan Wang, Ye Liao, Jing-Jing Zhang, Yu-Fan Wu, Si-Yu Sun, Jin-Tao Guo,Department of Gastroenterology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China
Xiao-Lin Sun, Department of Endoscopy Center, Liaoyang Liaohua Hospital, Liaoyang 111000,Liaoning Province, China
Abstract BACKGROUND Abscess formation is one of the complications after radical resection of rectal cancer; cases with delayed postoperative anastomotic abscess are rare. Here, we report a rare case of postoperative anastomotic abscess with a submucosal neoplasm appearing after rectal surgery. Ultimately, the patient was diagnosed and treated by endoscopic fenestration. In addition, we review the literature on the appearance of an abscess as a complication after rectal cancer surgery.CASE SUMMARY A 57-year-old man with a history of rectal malignancy resection complained of a smooth protuberance near the anastomotic stoma. Endoscopic ultrasonography revealed a hypoechoic structure originating from the muscularis propria, and a submucosal tumor was suspected. The patient was subsequently referred to our hospital and underwent pelvic contrast-enhanced computed tomography, which revealed no thickening or strengthening of the anastomotic wall. In order to clarify the origin of the lesion and obtain the pathology, endoscopic fenestration was performed. After endoscopic procedure, a definitive diagnosis of delayed anastomotic submucosal abscess was established. The patient achieved good recovery and prognosis after the complete clearance of abscess.CONCLUSION Endoscopic fenestration may be safe and effective for the diagnosis/treatment of delayed intestinal smooth protuberance after rectal cancer surgery.
Key Words: Anastomotic stoma; Rectal cancer; Submucosal tumor; Endoscopic fenestration; Delayed postoperative abscess; Case report
INTRODUCTION
Currently, laparoscopic radical resection is the standard and mainstay surgical treatment for rectal cancer[1-3]. Abscess formation is one of the complications after rectal cancer resection and is usually found within a few weeks post-surgery[4-6]. However,delayed postoperative anastomotic abscess is extremely rare, especially that presenting several years after surgery. Here, we report a rare case of delayed anastomotic submucosal abscess in a patient after rectal surgery who was diagnosed and treated by endoscopic fenestration. Furthermore, we performed a literature review on abscess complication following rectal cancer surgery.
CASE PRESENTATION
Chief complaints
A 57-year-old male patient was referred to our hospital for definite diagnosis and treatment of an intestinal smooth protuberance that appeared more than 3 years after rectal cancer surgery.
History of present illness
Initially, a smooth protuberance was found following a colonoscopy examination during a regular medical examination at a local hospital 3.5 years after rectal cancer surgery. The patient did not complain of any symptoms.
History of past illness
The patient presented with irregular stool and bloody stool since September 2015. He was admitted to a local hospital complaining of lower abdominal pain in February 2016. Colonoscopy revealed a large protuberant lesion located 15-18 cm from the anus,and a biopsy was taken. Endoscopic diagnosis was advanced rectal cancer, and pathological diagnosis was rectal adenocarcinoma (moderately differentiated).Laparoscopic radical resection of rectal cancer was performed in March 2016. Intraand post-operative pathology confirmed rectal adenocarcinoma (moderately differentiated). Colonoscopy performed during postoperative follow-up at 6 mo, 1 year, 2 years, and 3 years after the operation showed good anastomotic healing(Figure 1A).
Personal and family history
The patient had no specific personal and family history.
Physical examination
The patient did not have positive signs on physical examination.
Laboratory examinations
Laboratory testing including C-reactive protein level and leukocyte count, showed no abnormalities.
Imaging examinations
In November 2019 (3.5 years after operation), a smooth protuberance measuring approximately 15 mm × 15 mm (Figure 1B) was found near the anastomotic site by colonoscopy at the local hospital. The diagnosis was a protuberant lesion near the anastomotic stoma. Subsequent endoscopic ultrasonography (EUS) at the local hospital revealed a hypoechoic structure (Figure 1C) of approximately 1.12 cm × 0.91 cm in the rectal wall. A submucosal tumor (SMT) originating from the muscularis propria was suspected. The patient was referred to our hospital for definitive diagnosis and further treatment. We analyzed the patient's past history and examination and suspected that the protuberance was local recurrence of rectal cancer,postoperative abscess, or SMT. Subsequently, pelvic contrast-enhanced computed tomography (CT) was performed, which revealed no thickening or strengthening of the anastomotic wall (Figure 1D).
Further diagnostic work-up/endoscopic examination
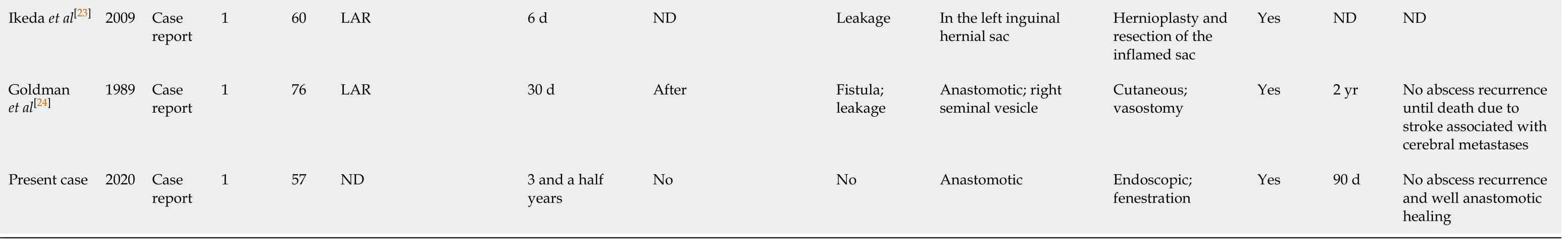
To clarify the origin of the lesion and obtain the pathology, endoscopic resection was performed. After dissecting the mucosal layer by using a dual knife, a soft cystic structure was observed. After opening the sac wall, a yellow viscous liquid can be seen flowing out (Figure 2A). Generally speaking, pus needs bacterial culture for further diagnosis; however, the lesion was at the rectum and highly susceptible to contamination by intestinal faeces and flora. Therefore, we did not culture the pus. We subsequently repeated the suction and irrigation procedures during endoscopic procedure to clean the area of the purulent exudate. The wound was closed using five metal clips finally (Figure 2B).
FINAL DIAGNOSIS
Based on the clinical, imaging, and endoscopic findings, we finally made a definitive diagnosis of delayed anastomotic submucosal abscess following rectal surgery.
TREATMENT
Diagnostic endoscopic fenestration that the patient underwent was also performed as a treatment for the intestinal protrusion lesion. In the process, the purulent exudate was cleaned completely, and the wound was entirely closed using clips.
OUTCOME AND FOLLOW-UP
After the endoscopic fenestration, the patient had no adverse effects and was treated with cephalosporin and glucose for anti-infection and nutrition therapy, respectively.The patient was discharged without complications 2 d after the procedure.Postoperative follow-up examination was performed, showing no evidence of recurrence in both white light endoscopy and narrow-band imaging (Figure 2C and D).
DISCUSSION
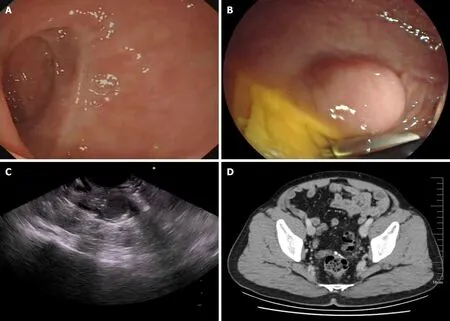
Figure 1 Anastomotic site findings. A: Previous colonoscopy showing no abnormalities near the anastomotic site; B: Last colonoscopy performed at the local hospital showing a smooth protuberance near the anastomotic site; C: Endoscopic ultrasound image showing a hypoechoic structure in the rectum; D: No obvious thickening or strengthening of the anastomotic wall was visible in the contrast-enhanced computed tomography scan of the pelvic cavity.
We report a case of delayed anastomotic submucosal abscess in a patient after rectal cancer surgery with a review of the literature. To the best of our knowledge, only 15 cases of abscess formation following rectal cancer surgery have been reported in the literature, including our case (Table 1), and this is the first report of delayed intestinal anastomotic abscess diagnosed and treated by endoscopic fenestration.
Currently, laparoscopic radical resection of rectal cancer has the advantages of less trauma, less bleeding, and rapid recovery of the intestinal function, and remains the most significant treatment for rectal cancer[2,3]. However, in any invasive procedures,complications cannot be completely avoided. These complications have an important impact on the postoperative recovery of patients. Postoperative complications of rectal cancer resection include postoperative hemorrhage, infection-related complications,and anastomosis-related complications (anastomotic fistula and stricture)[4-6].Postoperative abscess is one of the severe complications after rectal cancer surgery.Patients with postoperative abscess are usually symptomatic. Indicators of infection in laboratory tests will also increase accordingly, including C-reactive protein level and white blood cell count[7-9]. Postoperative abscess is related to the following factors: (1)After anti-infective therapy, viable bacteria are stored in the deep rectal wall,stimulating the rectal wall to form an abscess for a long time; (2) Local hematomas resulting from intra-incisional bleeding are not fully absorbed and develop into abscesses in the event of infection; and (3) Anastomotic fistulas are caused by poor blood supply and excessive tension, which lead to infection and abscess formation around the anastomotic site[10,11].
In the 15 cases reviewed herein, the patient ages ranged from 32-76 years, with an average age of 56.7 years[12-24]. The retrieved literature indicated that when patients were diagnosed with postoperative abscess after rectal cancer surgery, they usually presented with abdominal pain, obvious mass, and fever, accompanied by fistula or leakage formation (66.67%). Among the 15 patients (including this case), nine achieved the ideal treatment effect by drainage (60%), and the remaining patients underwent colostomy and cutaneous vasostomy for excretion of the purulent secretions to relieve symptoms in a timely manner. Five (33.33%) of the 15 patients had pelvic abscess afterrectal cancer surgery; in four (80%) of these patients, drainage was performed,whereas one (20%) was treated by colostomy. All five patients underwent successful abscess treatment (100%); four of these patients were followed (> 45 d), and the results showed improvement in three patients. In the fourth patient, Kollmorgenet al[15]reported an abscess recurrence after drainage of a small pelvic abscess, which improved after anti-infective treatment with ciprofloxacin. This suggests that conservative anti-infective treatment is a feasible option for limited abscess without increased risk of spreading. Presacral abscess was found in four (26.67%) cases, and three (75%) of these cases were treated by drainage. D'Hondtet al[19]reported intermittent fever, massive mucopurulent discharge from a perineal wound, and severe pain during radiotherapy after rectal cancer resection. After admission, CT showed a presacral abscess. Endo-sponge therapy was performed on the presacral abscess after biopsy confirmed no recurrent tumor. The prognosis was good after 5 mo of follow-up. A case reported by Mandaiet al[20]showed abscess formation in the paraanastomotic and subphrenic areas after low anterior resection of rectal cancer. The patient was treated by EUS-guided transgastric drainage and naso-cystic drainage innovatively and had no abscess recurrence at the 3-year follow-up. EUS-guided drainage is suggested as a safe and effective method for the treatment of postoperative abdominal abscess.
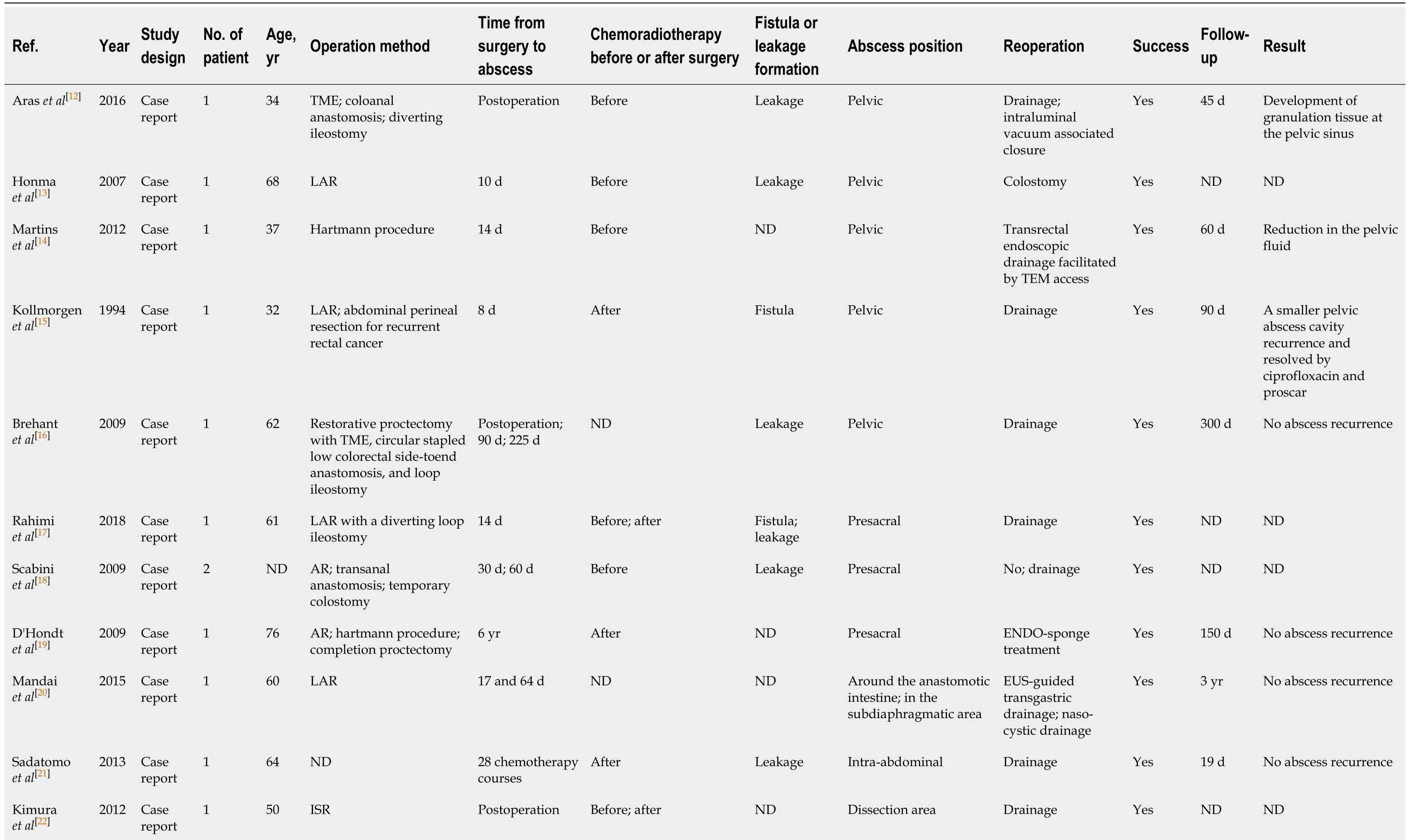
Table 1 Description of cases with abscess appearing as a complication after rectal cancer surgery
ND: Not described; TME: Total mesorectal excision; LAR: Low anterior resection; TEM: Transanal endoscopic microsurgery; AR: Anterior resection; ISR: Intersphincteric resection; EUS: Endoscopic ultrasonography.
Patients with postoperative abscess in the abdominal and pelvic cavity are usually symptomatic, whereas those with SMT are asymptomatic[25-27]. In the present case, the patient had no discomfort until colonoscopic examination detected the abnormality near the anastomotic site. Combined with the history of past illness, the patient was easily misdiagnosed with rectal cancer recurrence or rectal submucosal lesions. At this point, differential diagnosis was difficult, especially with SMT. The clinical features and EUS imaging were strongly suggestive of SMT after local tumor recurrence was disregarded based on pelvic CT findings. Endoscopic fenestration, however,ultimately indicated a rare delayed submucosal abscess rather than SMT.
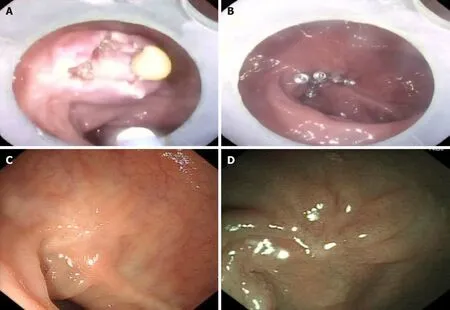
Figure 2 Endoscopic images. A: After opening the sac wall, a yellow viscous liquid can be seen flowing out; B: Colonoscopy image showing the five metal clips clipping the wound after complete clearance of the abscess; C and D: There was no evidence of abscess recurrence in both white light endoscopy and narrow-band imaging after a follow-up period of 11 mo.
To date, there is little information on delayed postoperative anastomotic abscess,especially that appearing several years after an operation. The later an abscess develops, the more complicated the causal relationship between the abscess and previous surgery is, making differential diagnosis more difficult. Patients with postoperative abscess usually present with fervescence, abdominal pain, and abdominal mass. Inflammatory indicator levels on blood tests usually increase and imaging examination may also suggest inflammatory exudation. However, these conditions may not occur when the abscess is wrapped around the cyst wall and does not spread. Therefore, abscess can mistakenly and easily be ruled out as a diagnosis,thereby delaying the patient's treatment. Currently, there are no guidelines for the treatment of postoperative abscess of rectal cancer. In general and based on the reviewed literature, large abscesses with complex anatomical locations are more commonly treated by drainage. If an abscess is associated with peritonitis, emergency surgical treatment can be performed. However, endoscopic fenestration is a better minimally invasive procedure for enveloping an abscess in the intestinal tract.
Endoscopic fenestration is an intuitive, safe, and reliable diagnostic method when clinical features and imaging findings are uncertain. Endoscopic fenestration has been widely used for intracranial cysts[28,29]; in recent years, it has also emerged as an effective method for the diagnosis and treatment of gastrointestinal protuberance[30,31].Endoscopic fenestration can safely and effectively diagnose abscess, reduce severe complications such as peritonitis, and reduce the use of invasive procedures such as abdominal drainage.
CONCLUSION
Although extremely rare, delayed submucosal abscess should be considered in the differential diagnosis in cases of suspected SMTs based on imaging during the late postoperative period in rectal cancer patients presenting with intestinal smooth swelling. When the protuberance is wrapped around the cyst wall without definite evidence of tumor recurrence or metastasis, endoscopic fenestration can be considered as a safe, effective, and feasible strategy for the definitive diagnosis and treatment of delayed intestinal smooth protuberance in patients after rectal surgery.
ACKNOWLEDGEMENTS
We thank Professor Sun SY, the co-corresponding author of this article, for his support and guidance to this study, as well as all other doctors who participated in this study.
 World Journal of Clinical Cases2020年23期
World Journal of Clinical Cases2020年23期
- World Journal of Clinical Cases的其它文章
- Understanding the immunopathogenesis of COVID-19: Its implication for therapeutic strategy
- What is the gut feeling telling us about physical activity in colorectal carcinogenesis?
- Latest developments in chronic intestinal pseudo-obstruction
- Correlation between ductus venosus spectrum and right ventricular diastolic function in isolated single-umbilical-artery foetus and normal foetus in third trimester
- Clinical efficacy of integral theory–guided laparoscopic integral pelvic floor/ligament repair in the treatment of internal rectal prolapse in females
- Treatment of Kümmell’s disease with sequential infusion of bone cement: A retrospective study
