Fourty-nine years old woman co-infected with SARS-CoV-2 and Mycoplasma: A case report
Zi-Ang Gao, Ling-Bao Gao, Xin-Jie Chen, Yu Xu
Zi-Ang Gao, Yu Xu, Department of Otolaryngology-Head and Neck Surgery, Renmin Hospital of Wuhan University, Wuhan 430060, Hubei Province, China
Ling-Bao Gao, Department of Transfusion, Taizhou People's Hospital, Taizhou 225300, Jiangsu Province, China
Xin-Jie Chen, Department of Neurology, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510006, Guangdong Province, China
Abstract BACKGROUND Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new virus responsible for the outbreak of respiratory illness known as coronavirus disease 2019 (CoVID-19). Mycoplasma is an uncommon co-infected pathogen with SARSCoV-2 and has not yet been reported. Computed tomography (CT), used as an accessory examination, may play a more significant role in this co-infection.CASE SUMMARY A 49-year-old female presented with a cough, expectoration and chest congestion followed by elevated C-reactive protein and erythrocyte sedimentation rate. CT images showed ground-glass opacities in bilateral lower lobes and a patchy and striate shadow in the right upper lobe. Immunoglobulin M antibody of Mycoplasma pneumoniae was positive and real-time fluorescence polymerase chain reaction of sputum was positive for SARS-CoV-2 nucleic acid. The diagnosis of CoVID-19 was made based on laboratory results, chest CT images, clinical manifestations and epidemiologic characteristics. She was treated with combination therapy for 17 d and showed a marked reCoVery.CONCLUSION Co-infection with SARS-CoV-2 and Mycoplasma in CoVID-19 patients appears to be uncommon. CT is an acceptable method for the primary diagnosis and treatment should be initiated as soon as possible. Combination therapy with antiviral, anti-inflammatory, traditional Chinese herbal medicine and interferon inhalation may be a reference for further progress in treating this co-infection.
Key Words: CoVID-19; SARS-CoV-2; Mycoplasma; Co-infection; Computed tomography; Infectious disease; Case report
INTRODUCTION
Coronavirus disease 2019 (CoVID-19) is a respiratory illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which has already infected over 70000 and killed more than 2000, especially in Wuhan, China. A study of 8274 samples showed that 5.8% of CoVID-19 infected and 18.4% of non-CoVID-19-infected patients had other infections[1]. However, co-infection with SARS-CoV-2 and Mycoplasma has not been reported previously. We report the case of a 49-year-old female co-infected with SARS-CoV-2 and Mycoplasma.
CASE PRESENTATION
Chief complaints
A 49-year-old woman came to the Outpatient Service of our hospital complaining of a cough, chest discomfort and fatigue on January 20, 2020.
History of present illness
The patient's symptoms started 5 d ago with a cough, expectoration and chest congestion.
History of past illness
She mentioned a travel history to Wuhan one week ago, the center of this CoVID-19 outbreak.
Physical examination
On admission, symptoms of cough, expectoration of white sputum, chest congestion and fatigue were observed, but her body temperature was normal 37.0°C (98.6°F).Coarse breath sounds in both lungs with wet rales distributed at the base of both lungs were heard on auscultation.
Laboratory examinations
Laboratory studies showed a normal leukocyte count (white blood cell count, 5.58 ×109/L) and normal lymphocyte count (lymphocyte count, 1.47 × 109/L). The leukocyte differential count indicated 64.9% neutrophils, 26.3% lymphocytes, and 5.9%monocytes. There were elevated blood levels of C-reactive protein (12.50 mg/L) and erythrocyte sedimentation rate (37 mm/h). Albumin (32.1 g/L) and serum calcium(3.26 mmoL/L) were lower. Immunoglobulin M (IgM) antibody ofMycoplasma pneumoniaewas positive (Table 1).
Imaging examinations
Unenhanced chest computed tomography (CT) showed ground-glass opacities in bilateral lower lobes and a patchy and striate shadow in the right upper lobe.According to these findings and due to her travel history to Wuhan, we speculated that she had Mycoplasma infection and suspected SARS-CoV-2 infection; therefore, we sent a throat swab for analysis and the results were expected to take several days.Considering her CT images and the rapid development of CoVID-19, we treated the patient with anti-inflammatory and empirical antiviral drugs in the first three days. CT images showed progressive manifestations.
Further diagnostic work-up
Three days later, real-time fluorescence polymerase chain reaction (RT-PCR) of sputum was positive for SARS-CoV-2 nucleic acid and her diagnosis of CoVID-19 was finally made based on laboratory results, chest CT images, clinical manifestations and epidemiologic characteristics. We were glad that we performed early intervention with antiviral therapy based on the previous CT manifestations.
CT showed multiple patchy ground-glass opacities and consolidated opacities in bilateral lower lobes (Figure 1) and a patchy and striate shadow of slightly high density in the upper right lung (Figure 2). This asymmetrical lesion in the upper right lobe was quite rare in the cases reported so far.
FINAL DIAGNOSIS
CoVID-19 and Mycoplasma infection.
TREATMENT
According to Chinese newest treatment guidelines for SARS-CoV-2, the patient was treated with antiviral drugs (Aluvia, Peramivir, Interferon-α2b), anti-inflammatory drugs (Cefonicid Sodium, Azithromycin, Moxifloxacin) and traditional Chinese herbal medicine (Lianhuaqingwen), combined with supportive care and interferon inhalation from January 25, 2020 and she was discharged on February 10, 2020.
OUTCOME AND FOLLOW-UP
On the 7thday, her cough, expectoration, chest congestion and debilitation started to improve. Laboratory tests of SARS-CoV-2 nucleic acid, lymphocyte count, erythrocyte sedimentation rate, potassium, total calcium, lactate dehydrogenase, blood oxygen saturation and IgM antibody ofMycoplasma pneumoniaeall showed that the patient had improved. A marked reCoVery was noted in this patient at the 2 wk follow-up.
DISCUSSION
The outbreak of CoVID-19 caused by SARS-CoV-2 has resulted in significant harm to human health globally, and has been declared a public health emergency of international concern by the WHO[2].
CoVID-19 has spread in 43 countries, including South Korea, Japan, Italy, and the United States.Person-to-person transmission in hospital and family settings has been identified and more than 2600 lives have been lost. From up-to-date data, it can seen that fever and cough are the most common symptoms, and both diarrhea and vomiting are rare. Most patients have lymphopenia and elevated levels of C-reactive protein on admission[3]. Among 2745 CoVID-19 patients, 104 were positive for multiple respiratory pathogens and 6/104 had co-infection with coronavirus (3/104), influenza A virus (2/104), rhinovirus (2/104), and influenza A H3N2 (1/104)[1]. Co-infection with SARS-CoV-2 and Mycoplasma is unusual and has not been reported previously.Treatment protocols and prognosis are new with few references.
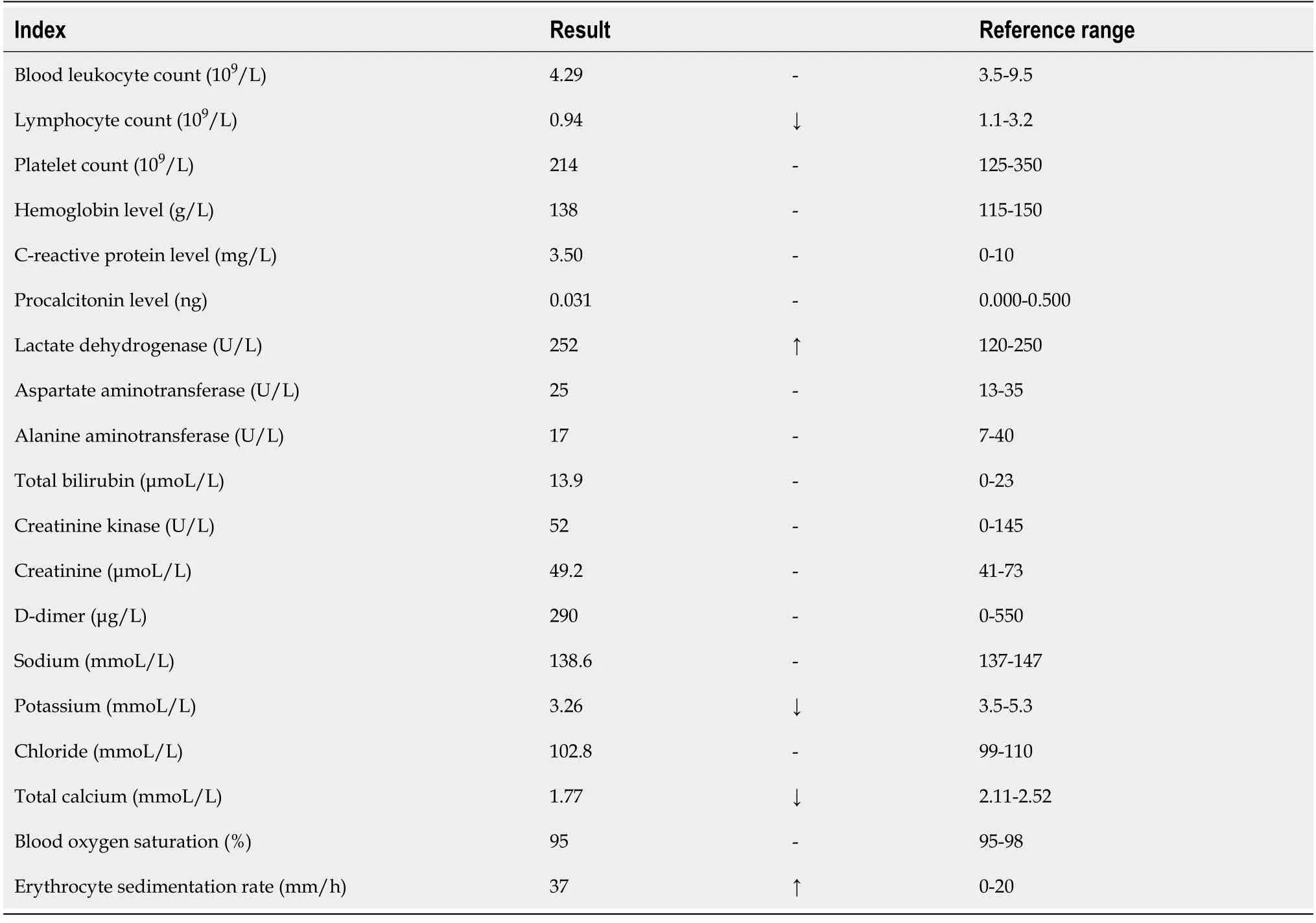
Table 1 Laboratory findings of the patient co-infected with severe acute respiratory syndrome coronavirus 2 and Mycoplasma
Imaging studies have shown that ground-glass opacity and bilateral patchy shadowing are the most common features on chest CT[3-5]. In our patient, progressive changes in typical CT manifestations were seen in bilateral lower lobes which were thought to be caused by CoVID-19, but an untypical isolated shadow in the upper right lung was also seen. This was thought to be caused by Mycoplasma infection.
CONCLUSION
In conclusion, co-infection with SARS-CoV-2 and Mycoplasma should not be ignored in clinical diagnosis and treatment, especially in the early course as CoVID-19 is a rapidly developing disease. CT manifestations may be a better and quicker route to the diagnosis of CoVID-19 than nucleic acid testing using RT-PCR, and can result in timely treatment. Clinical improvement in CT images in our patient suggested that our novel combination therapy may be a reference for further progress in the treatment of this co-infection. As these pathogens are very infectious, doctors and nurses, particularly those on the first line, require personal protective equipment.
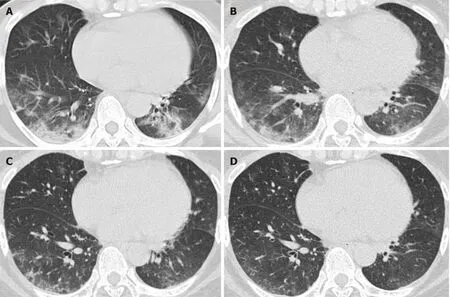
Figure 1 Unenhanced computed tomography images in a 49-year-old woman (axial imaging). Computed tomography (CT) radiographs show multiple patchy ground-glass opacities and consolidated opacities in bilateral lower lobes, the middle lobe of the right lung and the tongue segment of the upper left lung, as treatment progressed, CT manifestations showed improvement. A: Day 7 (2020.1.26) after the onset of symptoms; B: Day 12 (2020.1.31) after the onset of symptoms; C: Day 16 (2020.2.4) after the onset of symptoms; D: Day 21 (2020.2.9) after the onset of symptoms.
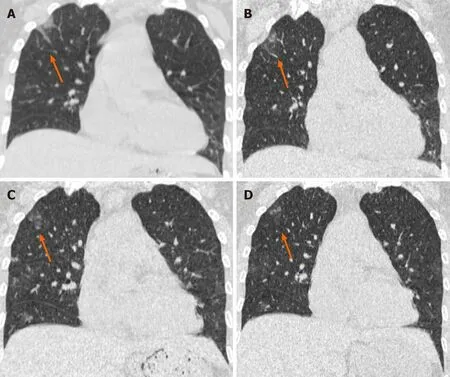
Figure 2 Unenhanced computed tomography images in a 49-year-old woman (coronal imaging). Computed tomography radiographs show a patchy and striate shadow of slightly high density in the upper right lung (arrows), as the treatment progressed, this asymmetrical lesion was gradually absorbed. A:Day 7 (2020.1.26) after the onset of symptoms; B: Day 12 (2020.1.31) after the onset of symptoms; C: Day 16 (2020.2.4) after the onset of symptoms; D: Day 21(2020.2.9) after the onset of symptoms.
 World Journal of Clinical Cases2020年23期
World Journal of Clinical Cases2020年23期
- World Journal of Clinical Cases的其它文章
- Understanding the immunopathogenesis of COVID-19: Its implication for therapeutic strategy
- What is the gut feeling telling us about physical activity in colorectal carcinogenesis?
- Latest developments in chronic intestinal pseudo-obstruction
- Correlation between ductus venosus spectrum and right ventricular diastolic function in isolated single-umbilical-artery foetus and normal foetus in third trimester
- Clinical efficacy of integral theory–guided laparoscopic integral pelvic floor/ligament repair in the treatment of internal rectal prolapse in females
- Treatment of Kümmell’s disease with sequential infusion of bone cement: A retrospective study
