Large and unusual presentation of gallbladder adenoma: A case report
Lin-Li Cao, Hua Shan
Lin-Li Cao, Hua Shan, Department of Medical Imaging, Jiangsu Second Hospital of Traditional Chinese Medicine, Nanjing 210017, Jiangsu Province, China
Abstract BACKGROUND Gallbladder adenoma is a relatively rare benign tumor with a potential for malignant transformation if found to be greater than 1 cm in size.CASE SUMMARY Herein, we report a case of a 51-year-old female with large 3 cm × 3 cm mass of gallbladder adenoma that was misdiagnosed as adenocarcinoma due to its clinical presentation. Computed tomography and magnetic resonance imaging scans showed an irregularly shaped cauliflower-like lump in the gallbladder measuring 38 mm × 32 mm corresponding to a malignant tumor and several gallbladder stones with low diffusion-weighted imaging and equisignal of T1-weighted imaging and T2-weighted imaging; moreover, the CA 19-9 levels were very high(184.1 U/mL). Pathology reports after tumor resection showed adenoma with moderate epithelial atypia and moderate atypia in the focal area with fine pedicle and no clear infiltration.CONCLUSION Computed tomography and magnetic resonance imaging scans need to be carefully scrutinized in certain rare cases of adenomas with abnormal imaging features.
Key Words: Gallbladder adenoma; Computed tomography; Magnetic resonance imaging;Case report; Imaging; Misdiagnose
INTRODUCTION
Gallbladder adenomas (GBA) are primary neoplasms of the gallbladder that are not very common and are estimated to be found in about 0.1%-10% of cholecystectomy cases. These benign tumors that usually present as single polypoid masses are classified as tubulary, papillary and tubulopapillary based on histological morphology. GBA are categorized as pyloric gland, intestinal and biliary type adenomas depending on their origin. GBA occur in mostly in females and middleaged individuals[1,2]. Gallbladder adenocarcinoma (GBC), a malignant tumor of the biliary tract, is known to be the fifth common neoplasm of the digestive tract[3]; it varies in its geographical distribution and ethnicity[4]. Presence of cholelithiasis, polyps bigger than 1 cm in diameter, female gender, advancing age, increased body mass index and chronic gallbladder inflammation are some of the risk factors for GBC[5].GBA are usually smaller than 20 mm in size[6], and those that are more than 1cm in size have a risk of developing into adenocarcinomas[2]. In the current report, we present the clinical data, images and pathological results of a case of gallbladder adenoma of size 3 cm × 3 cm that was misdiagnosed as adenocarcinoma due to its unusual clinical presentation.
CASE PRESENTATION
Chief complaints
A 51-year-old female of Han Chinese ethnicity from Nanjing, Jiangsu province of China, presented at the Emergency Department of our institution (Jiangsu Second Hospital of Traditional Chinese Medicine) with an acute pain in the right upper quadrant of her abdomen on August 2, 2017.
History of present illness
The pain was colic and radiated to the back. Concomitant symptoms included nausea,vomiting and diarrhea but no fever or chills. Neither weight loss nor anorexia was observed. She was prescribed omeprazole once a day for 2 d and sent home. Although the medication gave her temporary relief from the pain, she continued to experience severe abdominal spasms.
History of past illness
There was no previous medical history of hypertension, diabetes, coronary heart disease, hepatitis, tuberculosis, typhoid fever and other infectious diseases. There was also no history of trauma, surgery, blood transfusion or recent vaccination.
Physical examination
Physical examination revealed no abdominal lumps, jaundice or itchy skin.Tenderness was observed in the right upper quadrant with a positive Murphy’s sign.There was no rebound tenderness.
Laboratory examinations
Results of routine blood and urine tests were normal. Liver function test results showed higher than normal values (alanine transaminase: 164 U/L, aspartate transaminase: 179 U/L, gamma-glutamyltransferase: 371 U/L). Levels of CA19-9 were found to be elevated at 184.1 U/mL. Levels of other tumor markers were as follows:alpha-fetoprotein: 7.53 ng/mL, carcinoembryonic antigen: 1.87 ng/mL, CA125: 12.56 U/mL, CA153: 18.54 U/mL and CA724: 1.18 U/mL.
Imaging examinations
Abdominal computed tomography (CT) scan showed pathological conditions corresponding to a large cauliflower-like mass in the gallbladder. CT (Figure 1) and magnetic resonance imaging (MRI, Figure 2) scans performed on August 4, 2017 revealed an irregularly shaped cauliflower-like lump in the gallbladder measuring 38 mm × 32 mm corresponding to malignant tumor (GBC) and multiple stones in the gallbladder. T1-weighted imaging and T2-weighted imaging (T2WI) were equisignal with low diffusion-weighted imaging (DWI) signal. There was no detectable extension through the gallbladder wall or invasion of adjacent structures. The biliary system was normal with no associated hepatic lesions and no apparent liver damage or abnormalities in the cystic duct, common hepatic duct or intrahepatic ducts.
FINAL DIAGNOSIS
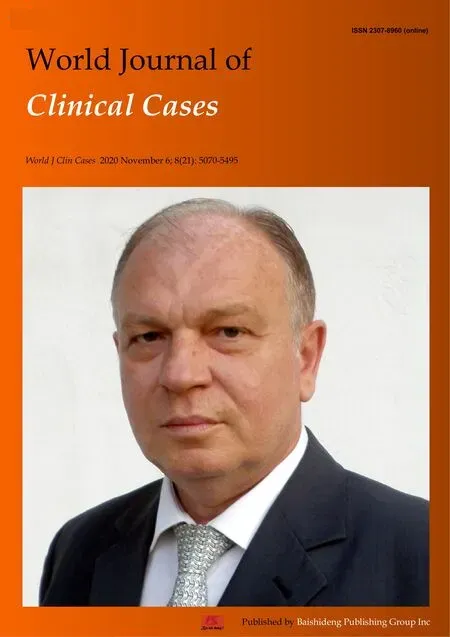
Pathology reports after tumor resection showed adenoma with moderate epithelial atypia and moderate atypia in the focal area with fine pedicle and no clear infiltration.
TREATMENT
As per the patient’s wishes, laparoscopic cholecystectomy was performed under general anesthesia. Intraoperative probe revealed no obvious abnormality in the liver,common bile duct dilation with mild adhesion of the omentum to the gallbladder,gallbladder bile duct expansion, gallbladder size about 10 cm × 5 cm and no invasion of the serosal layer. Irregular masses measuring 3 cm × 3 cm and several stones of different sizes in the gallbladder were found at surgery. The resected samples were sent for histopathological examination. After the surgery, the patient was treated with medications that included anti-inflammatory, acid inhibition, gastric protection, fluid supplementation, water and electrolyte balance and anticoagulation. The patient was discharged without any complications. Pathological assessment of the tumors showed adenoma with moderate epithelial atypia and moderate atypia in the focal area with fine pedicle and no clear infiltration (Figure 3).
OUTCOME AND FOLLOW-UP
A follow-up was conducted on September 18, 2017. Ultrasound examination showed no evidence of any abnormality in the gallbladder area.
DISCUSSION
The incidence of GBA, which are benign and highly vascularized tumors, is low[1].They are generally asymptomatic unless there are multiple large adenomas or the tumor tissues are detached resulting in floating fragments in the bile duct or attached to the gallstones[7]. They usually appear as sessile polypoid isoechoic or hyperechoic lesions on imaging. Differentiating GBA from GBC might be difficult because polypoid lesion with arterial enhancement may be seen in early-stage adenocarcinoma[8]. On CT imaging, GBC appears as a mass completely occupying or replacing the gallbladder lumen, focal or diffuse asymmetric gallbladder wall thickening or an intraluminal polypoid lesion. GBA and GBC can sometimes coexist making diagnosis a challenge because wall thickening patterns or polypoid growth result in overlap of imaging findings leading to uncertainty in preoperative diagnosis[9].
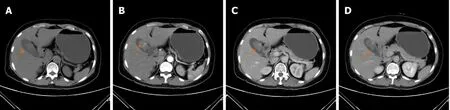
Figure 1 Contrast-enhanced computed tomography scan of the gallbladder. A: Nodular in low density shadow, about 31 mm × 23 mm size; B: Arterial enhancement scanning, computed tomography value of 47 HU; C: Venous phase computed tomography value of 51 HU; D: Delayed computed tomography value of 42 HU. Arrows in the figures indicate irregular cauliflower-shaped mass measuring 38 mm × 32 mm with its base connected to the gallbladder wall.

Figure 2 Magnetic resonance imaging scan of the gallbladder. Signals of T1-weighted imaging (A) and T2-weighted imaging (B) are equal. Diffusionweighted imaging signal (C) was low. Arrows in the figures indicate irregular cauliflower-shaped mass with its wide base connected to the gallbladder wall. T1WI: T1-weighted imaging; T2WI: T2-weighted imaging; DWI: Diffusion-weighted imaging.
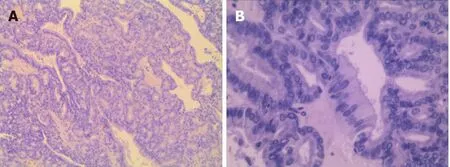
Figure 3 Hematoxylin and eosin staining of surgically resected gallbladder tumor. A: Magnification (10 ×); B: Magnification (40 ×). Image shows adenoma with moderate epithelial atypia, and moderate atypia in the focal area with fine pedicle and no clear infiltration.
In our patient, the misdiagnosis of GBA as GBC was due to: (1) The appearance of the lesion being irregular and cauliflower-shaped; (2) The lesion had a wide base; (3)Contrast-enhanced CT showed obvious and significantly enlarged masses consistent with the features of malignant tumors; and (4) CA19-9 levels of our patient were very high, which coincided with the fact that the patient presented the highest incidence of cholecystic carcinoma and that CA19-9 is considered a prognostic marker for GBC[9]. In this case, both T1WI and T2WI signals during MRI were equal, whereas for adenomas,T1WI signal is low and T2WI signal is high. Moreover, the diameter of the lesion that was more than 3 cm was confined to the gallbladder, and there was no distant metastasis. Hence, it was not easy to differentiate GBA from GBC. Interestingly in this case, the DWI signal was low, whereas the DWI signal is expected to be high in malignant tumor. Therefore, the diagnosis was not easy in this case. From this case, it is important to note that misdiagnosis can be prevalent due to large size of polypoid lesions with DWI signals being low and elevated levels of tumor markers; but physicians could check for T1WI and T2WI signals to be equal, which can give an estimation whether the tumor is GBA.
Recently, techniques such as multidetector CT, high-resolution ultrasound and use of apparent diffusion coefficient and lesion to spinal cord ratio DWI have been proposed to increase the diagnosis and differentiation between malignant and benign tumors[10,11]. In spite of these technical advancements, the detection of gallbladder cancer from clinical and imaging data at curative stages still remains tricky and challenging. GBA are reported to be benign lesions of cauliflower shape, narrow base,with mulberry shape and uniform reinforcement. DWI can help to differentiate GBC from adenoma and well-differentiated from higher-grade adenocarcinoma[12]. GBC is highly suspected when a large gallbladder mass that nearly fills or replaces the lumen and often directly invades the surrounding liver parenchyma. GBA is often confined to the gallbladder and it will not infiltrate the surrounding structure. Generally, in gallbladder adenoma, the CA19-9 level is not high[13]; in our patient, this tumor index increased significantly. Therefore, careful examination of MRI along with other clinical and laboratory examination could improve the diagnostic accuracy.
CONCLUSION
In conclusion, our case report highlights the importance for oncologists to carefully evaluate characteristic imaging appearances and values of CT/MRI scans of primary gallbladder tumors to determine the stage of cancer for appropriate treatment regimen. The incidence of gallbladder adenoma is relatively low and is predisposed to malignancy. Hence, carefully distinguishing between GBA and GBC is necessary for optimizing the treatment strategy for the patients.
 World Journal of Clinical Cases2020年21期
World Journal of Clinical Cases2020年21期
- World Journal of Clinical Cases的其它文章
- Strategies and challenges in the treatment of chronic venous leg ulcers
- Peripheral nerve tumors of the hand: Clinical features, diagnosis,and treatment
- Treatment strategies for gastric cancer during the COVID-19 pandemic
- Oncological impact of different distal ureter managements during radical nephroureterectomy for primary upper urinary tract urothelial carcinoma
- Clinical characteristics and survival of patients with normal-sized ovarian carcinoma syndrome: Retrospective analysis of a single institution 10-year experiment
- Assessment of load-sharing thoracolumbar injury: A modified scoring system
