Supermicroscopy and arterio-venolization for digit replantation in young children after traumatic amputation: Two case reports
Yun Chen, Ze-Min Wang, Jing-Hui Yao
Yun Chen, Department of Pediatric Orthopedics, The Third Affiliated Hospital of Southern Medical University, Guangzhou 510000, Guangdong Province, China
Ze-Min Wang, Department of Pediatric Orthopedics, Loudi Central Hospital, Loudi 417000,Hunan Province, China
Jing-Hui Yao, Department of Pediatric Orthopedics, The Third Affiliated Hospital of Southern Medical University, Guangzhou 510630, Guangdong Province, China
Abstract BACKGROUND To report the application of supermicroscopy combined with arterio-venolization without venous anastomosis for replantation of digits following traumatic amputation in young children.CASE SUMMARY In March 2016, we treated two children aged 2 years and 7 years with traumatic digit amputation, no venous anastomosis, and bilateral digital inherent arteries on the palmar side. Supermicroscopy combined with an arteriovenous technique was adopted to improve the replantation surgery. Postoperative management involved auxiliary treatments such as anticoagulation, composure, antiinflammatory drugs, and insulation. After treatment, the amputated fingers survived completely without major complications, with good recovery.CONCLUSION Supermicroscopy combined with arterio-venolization is a safe and effective approach to treat traumatic digit amputation in young children without venous anastomosis.
Key Words: Digit replantation; Traumatic digit amputation; Children; Supermicroscopy;Arterio-venolization; Case report
INTRODUCTION
Replantation of traumatically amputated digits in infants and young children is one of the most difficult operations in hand microsurgery, especially in conditions without venous anastomosis. Even for experienced orthopedic surgeons and hand microsurgeons, this type of surgery is extremely challenging. In microsurgical treatment, if anastomosis is performed on the blood vessels with diameters < 0.8 mm,it is known as a super-microsurgical operation, which is more delicate and highly demanding for the surgeon. In super-microsurgical operations, special surgical instruments are needed for anastomosis of 0.3-0.8-mm diameter blood vessels,including microscopes with 20-50 times magnification, microforceps with 0.06 mm tips, 12-0 non-damage blood vessel wires, and needles with 0.05 mm direct meridian[1].
With the super-microsurgical technique, there is still an important issue for infants and young children who do not have venous anastomoses[2,3]. If the terminal segment of the finger is severed, the closed loop of blood vessels cannot be formed after arterial anastomosis, which can lead to arterial occlusion as well as fingertip ischemia and necrosis. Faced with such cases, some hospitals choose to abandon replantation of amputated digits, resulting in loss of the finger and functional and aesthetic defects.Hospitals with superior microscope technology often use arterial anastomosis and fingertip bloodletting, which have a low success rate and are technically demanding and labor intensive. There have been a few reports on the use of arterio-venolization technique for treatment of replantation of distal digits in infants and young children[4,5]. We present a retrospective summary of two successful cases of digit replantation in young children using an arteriovenous technique in blood vessels < 0.5 mm in diameter, which could be of instructive value for clinical practice.
CASE PRESENTATION
Chief complaints
Case 1:A 7-year-old boy accidentally cut off his left distal index finger with a broken glass while playing at home an hour ago.
Case 2:A 2-year-old boy was admitted to the hospital 3 h after his left thumb was crushed when closing the door, resulting in rupture of the ventral soft tissues in the distal phalanx of the thumb.
History of present illness
Case 1:In March 2016, a 7-year-old boy accidentally cut off his left distal index finger with a broken glass while playing at home. The dorsal cut of the middle index finger reached the bone surface in another wound, and all the dorsal veins were broken.
Case 2:In March 2016, a 2-year-old boy was admitted to the hospital 3 h after his left thumb was crushed when closing the door, resulting in rupture of the ventral soft tissues in the distal phalanx of the thumb. The left thumb was squeezed apart and fractured.
History of past illness
No special circumstances.
Personal and family history
No special circumstances.
Physical examination
Case 1:The dorsal cut of the middle index finger reached the bone surface in another wound, and all the dorsal veins were broken. The left index finger was cut and severed, and the dorsal side of the middle finger was cut.
Case 2:The scope of the rupture involved three quarters of the soft tissue on the volar and ventral distal phalanx of the left thumb, starting from the fingernail root on the dorsal side, leaving no dorsal vein, intact bilateral digit arteries on the palm side observed under microscope, presence of the accompanying digit nerves, and no serious crushing damage on the ventral thumb, indicating no venous anastomosis and bilateral digital artery integrity.
Laboratory examinations
No special circumstances.
Imaging examinations
Case 1:Fracture of distal phalanx.
Case 2:No special circumstances.
FINAL DIAGNOSIS
Case 1
The left index finger was cut and severed, and the dorsal side of the middle finger was cut.
Case 2
Left thumb squeezed apart and fractured.
TREATMENT
Case 1
One hour after injury, the patient went to our hospital for treatment, was informed of the surgical risk and method, and was scheduled to undergo limb salvage replantation. After the wound was cleaned, the broken bones were fixed. For the dorsal part of the broken distal forefinger, we could not find an anastomosis of the digital vein with suitable diameter. Bilateral digital arteries on the palmar side of finger were completely broken without defect. The fracture of the finger nerve was neat. The extensor tendon and flexor digitorum profundus tendon were anastomosed.During the operation, the proximal and distal ulnar digital arteries were anastomosed using a super-microsurgical technique. The distal radial arteries were anastomosed to dorsal radial veins to form a closed loop of blood flow (Figure 1). The ulnar digital nerves were anastomosed. The patient was kept at a constant temperature with continuous irradiation of a baking lamp and given intravenous infusion of papaverine as well as anti-tetanus and anti-infective treatment.
Case 2

Figure 1 Treatment for case 1. A: Preoperative appearance; B: Postoperative appearance.
Debridement and suture are recommended in many hospitals, but the patient’s parents could not accept repair of finger stump. They came to our hospital for treatment and were informed of the surgical risk and method, and we planned to perform limb salvage replantation. The scope of the rupture involved three quarters of the soft tissue on the volar and ventral distal phalanx of the left thumb, starting from the fingernail root on the dorsal side, leaving no dorsal vein, intact bilateral digit arteries on the palm side observed under microscope, presence of the accompanying digit nerves, and no serious crushing damage on the ventral thumb, indicating no venous anastomosis and bilateral digital artery integrity. During the operation, the ulnar digital arterial anastomosis was performed using a supermicroscopic technique.The distal radial digital artery was connected to the proximal dorsal digital vein, and the ulnar digital nerve was anastomosed (Figure 2). Postoperative plaster fixation of the elbow joint to the affected finger was adopted to prevent the child’s involuntary hand movements from affecting the blood circulation. The patient was kept at a constant temperature under the continuous irradiation of a baking lamp and given intravenous infusion of papaverine as well as anti-tetanus and anti-infective treatment.After the operation, the fingertip survival was complete and full.
OUTCOME AND FOLLOW-UP
Case 1
No major complications occurred during treatment and follow-up. Three years after the operation, the palmar skin of the distal phalanx of the finger was examined, and the two-point discrimination sensation reached 6 mm and the distal interphalangeal joint could not move, while the proximal interphalangeal joint and metacarpoparacular joint had normal activity, demonstrating good appearance and prognosis(Figure 3).
Case 2
In the course of treatment and follow-up, no major complications occurred. Two years after the operation, the palmar skin of the distal phalanx of the finger was examined,and the two-point discrimination sensation reached 5 mm, with normal knuckle activities and excellent prognosis (Figure 4).
DISCUSSION
Replantation of an amputated digit in infants or young children is technically challenging because vascular conditions are difficult to control, especially when it is difficult to find veins of suitable size for anastomosis[2,3]. If no saturation is undertaken or only the artery is sutured, insufficient blood supply or reocclusion of blood vessels can occur after reperfusion due to the absence of a reflux channel, resulting in loss of blood supply at the distal end and eventually leading to a high probability of ischemia and necrosis of the replantation finger. The veins in the ventral center of the finger are already in an extremely vulnerable state at the distal end of the finger and cannot fit well. Arterial anastomosis and bloodletting therapy can lead to a large amount of blood loss, seriously increased workload, heavy psychological burden on the parents,and low success rate[6,7]. In the present report (Table 1), two blood vessels and one nerve were anastomosed at one time (Figure 5),the wound was closed normally, the operation time was 3.5 h and 4 h, and the intraoperative blood loss was 20 mL and 50 mL, respectively. No vasospasm or insufficient blood supply occurred in the two casesduring the anastomosis[5].
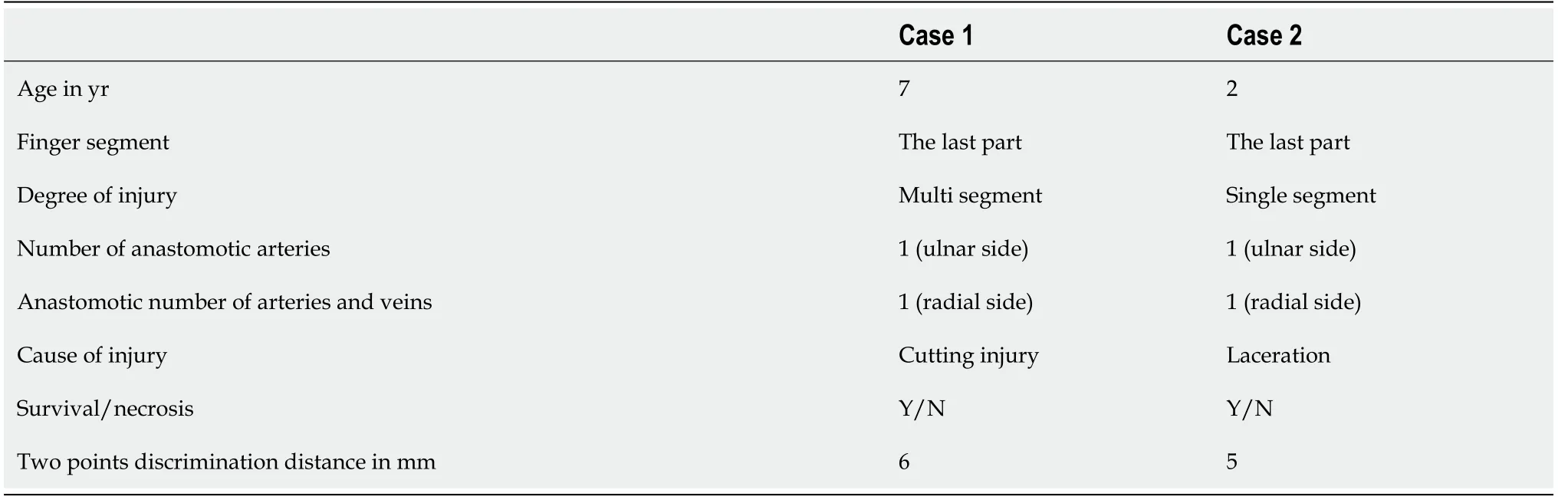
Table 1 Summary of the two patients’ cases
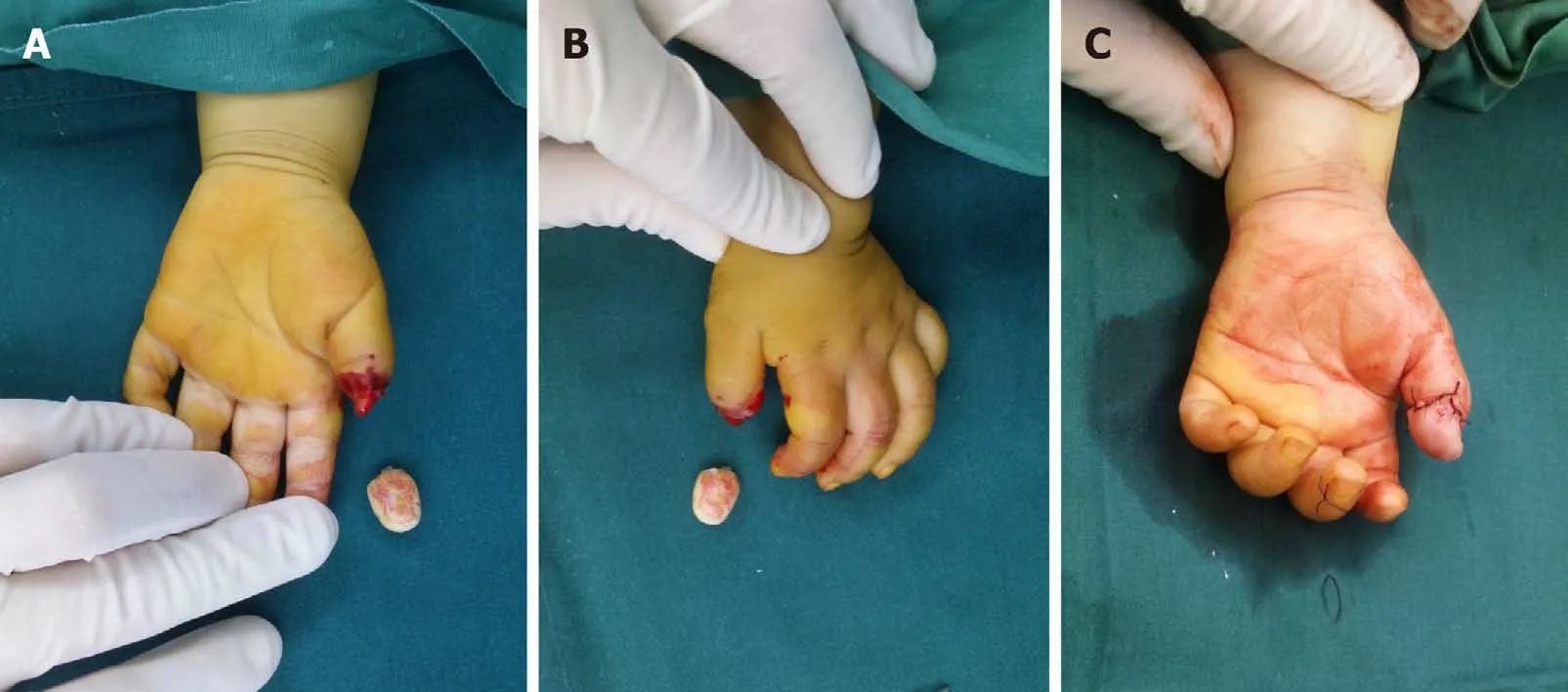
Figure 2 Treatment for case 2. A and B: Preoperative appearance; C: Postoperative appearance.

Figure 3 Case 1, appearance and function 3 years after operation.
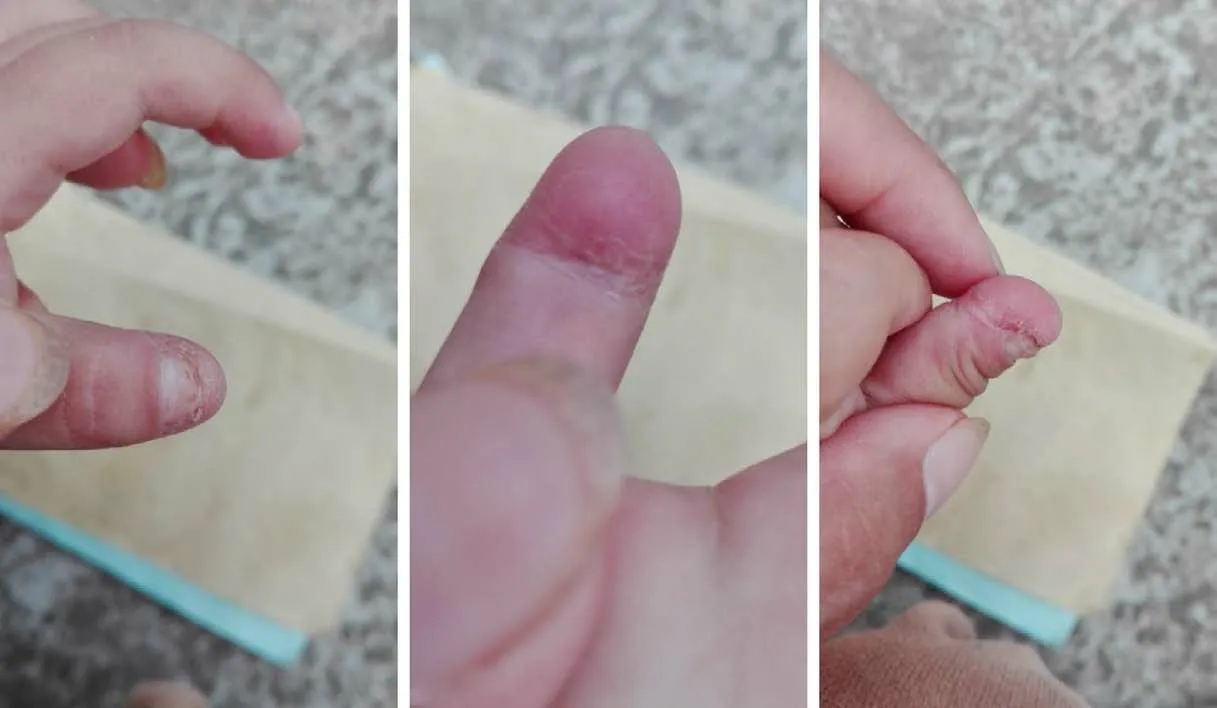
Figure 4 Case 2, appearance and function 2 years after operation.
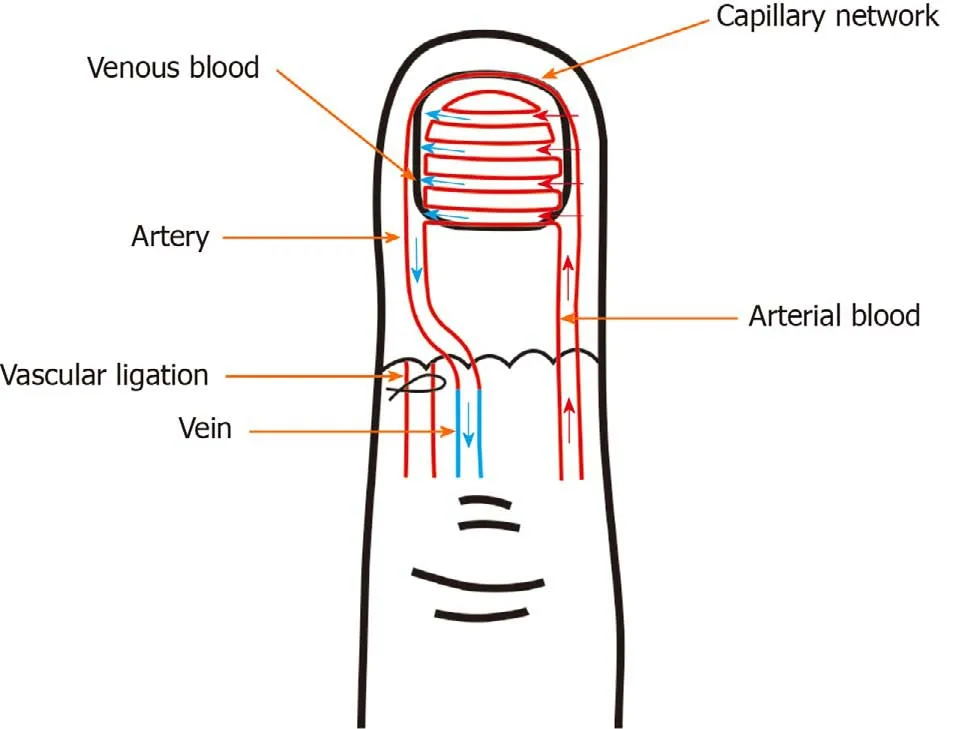
Figure 5 Surgical procedure demonstration.
The ulnar digital artery has good elasticity, with a thick blood vessel and unobstructed blood supply after anastomosis, so it is anastomosed as the arterial supply. We select the radial side of the distal arteries, dissect 1.5 mm of blood vessels,select a vein with a diameter of 0.3-0.5 mm on the lateral phalangeal groove of the proximal finger, hydraulically expand the diameter of the distal artery and proximal vein, anastomose with 12-0 noninvasive vascular wire under a 26 × microscope, and perform a postoperative strangulation test to determine the vascular patency.Immediately after the operation, whether the capillary filling of fingers is good,whether the finger pulp is full, and whether the bleeding of acupunctured fingertip is normal should be checked. A negative blood capillary filling test indicates a good finger blood supply. We believe that because of the widespread presence of the capillary network at the distal end of the artery, and after the reliable arterial vascular perfusion, the blood can flow into the contralateral digital artery reflux following the capillary network. Meanwhile, because of the pressure of the capillaries, blood can be effectively perfused to the distal limb to provide nutrition in the soft tissue. We used postoperative sedation and anti-infective and anti-tetanus treatment. During the treatment, the suture area of the broken end of the finger had little infiltration of blood, and dry closure was observed on the 2ndd after the operation. Postoperative nursing observation is particularly important, with close observation of the color change of the fingertip after the operation, and timely replacement of the dressing to avoid gauze compression and clotting in the anastomotic vessels, which may lead to vessel blockage.
CONCLUSION
Compared with the traditional surgical methods, supermicroscopy combined with arteriovenous therapy can effectively improve the success rate of finger preservation and demonstrates the advantages of one-stage closure to reduce blood loss, infection,and length of hospital stay and to restore the distal sensation of the finger. The method is an effective and safe option for treatment of childhood traumatic finger amputation.
 World Journal of Clinical Cases2020年21期
World Journal of Clinical Cases2020年21期
- World Journal of Clinical Cases的其它文章
- Strategies and challenges in the treatment of chronic venous leg ulcers
- Peripheral nerve tumors of the hand: Clinical features, diagnosis,and treatment
- Treatment strategies for gastric cancer during the COVID-19 pandemic
- Oncological impact of different distal ureter managements during radical nephroureterectomy for primary upper urinary tract urothelial carcinoma
- Clinical characteristics and survival of patients with normal-sized ovarian carcinoma syndrome: Retrospective analysis of a single institution 10-year experiment
- Assessment of load-sharing thoracolumbar injury: A modified scoring system
