Pancreatic panniculitis and elevated serum lipase in metastasized acinar cell carcinoma of the pancreas: A case report and review of literature
Rainer Christoph Miksch, Tobias S Schiergens, Maximilian Weniger, Matthias Ilmer, Philipp M Kazmierczak,Markus O Guba, Martin K Angele, Jens Werner, Jan G D'Haese
Rainer Christoph Miksch, Matthias Ilmer, Department of General, Visceral, and Transplantation Surgery, Ludwig-Maximilians-University Munich, Munich 81377, Bavaria, Germany
Tobias S Schiergens, Department of General Visceral Transplantat Vasc & Thorac Surg,Campus Grosshadern, University of Munich, Munich 81377, Germany
Maximilian Weniger, Jan G D'Haese, Department of General, Ludwig Maximilians-University(LMU), Munich 81377, Germany
Philipp M Kazmierczak, Department of Radiology, Ludwig-Maximilians-University Munich,Munich 81377, Germany
Markus O Guba, Department of Surgery, University of Munich, Klinikum Grosshadern, Munich University Hospital, Munich 81377, Germany
Martin K Angele, Department of General, University of Munich, Klinikum Grosshadern,Hospital of the University of Munich, Munich 81377, Germany
Jens Werner, Department of General, Klinikum Univ Munchen, Klin Allgemeine Viszeral Transplantat Gefass & Th, Standort Grosshadern, Ludwig-Maximilians-University (LMU),Munich 81377, Germany
Abstract BACKGROUND Pancreatic panniculitis is an extremely rare condition associated with different underlying pancreatic disorders and characterized by subcutaneous fat necrosis induced by elevated serum lipase levels. These lesions usually affect the lower extremities and may precede abdominal symptoms of pancreatic disease. Acinar cell carcinoma (ACC) of the pancreas is a rare pancreatic neoplasm, accounting for only 1%-2% of pancreatic tumors in adults.CASE SUMMARY We present the case of a 72-year-old man with ACC of the pancreatic head and synchronous liver metastases. Both the primary tumor and liver metastases were resected. Serum lipase was elevated before surgery and decreased to normal postoperatively. Rising serum lipase levels at follow-up led to the diagnosis of hepatic recurrence. This disease progression was then accompanied by pancreatic panniculitis, with subcutaneous fat necrosis and acute arthritis. To the best of our knowledge, only 4 cases have been reported in the literature and each showed a similar association of serum lipase levels with pancreatic panniculitis and progression of ACC.CONCLUSION Clinical symptoms and progression of ACC may correlate with serum lipase levels, suggesting potential usefulness as a follow-up biomarker.
Key Words: Pancreatic panniculitis; Lipase; Acinar cell carcinoma; Pancreatic cancer; Case report
INTRODUCTION
Pancreatic panniculitis was first described in 1883 and appears in 0.3%-3% of patients with various pancreatic diseases[1-3]. Acinar cell carcinoma (ACC) of the pancreas is equally rare and reported in only 1%-2% of all exocrine pancreatic tumors in adults[4,5].Hyperlipasemia can occur in patients with ACC of the pancreas[6], since lipase production takes place in the acinar cells. Due to the acinar origin of this tumor,pancreatic panniculitis is observed more frequently in ACC than in any other pancreatic tumor types[7,8]. Lipase hypersecretion can cause fever, polyarthritis,eosinophilia, and progression of fat necrosis to pancreatic panniculitis[9,10], a condition described as “lipase hypersecretion syndrome” by Butturiniet al[11].
The combination of symptoms of pancreatitis, panniculitis, and polyarthritis has been summarized as “PPP syndrome” and is associated with a mortality rate of up to 24% in pancreatic cancer[12,13]. Additionally, in patients with PPP syndrome, necrosis may also affect subcutaneous tissue and skeletal structures as well[14]. The hypothesis of the underlying cause of these symptoms is secretion of pancreatic enzymes into the bloodstream[15].
Microscopically, pancreatic panniculitis shows necrosis, neutrophil infiltration, and necrotic adipocytes called “ghost cells”[16]. With regard to treatment options, early resection of the primary AAC tumor is recommended, whenever feasible. This approach may also include resection of synchronous and/or metachronous metastases[17]. Indeed, almost 50% of the patients have evidence of synchronous metastases at the time of diagnosis, and surgical resection is the treatment of choice[18,19].
Evidence for the administration of chemotherapy in ACC is scarce and thus, it is not clear whether patients with ACC might benefit from systemic adjuvant or neoadjuvant regimens.Only small case series have been published on adjuvant chemotherapy[20,21].Oxaliplatin-based and 5-fluorouracil (5-FU)-based therapeutic protocols seem to show better antitumor activity compared to gemcitabine-based protocols[22]. Yooet al[19]described oxaliplatin-based regimens in locally advanced and metastatic disease of ACC with significantly improved progression-free survival compared to a gemcitabine-based regimen. Furthermore, Jimboet al[23]showed 5-FU-based neoadjuvant chemotherapy to be a promising option for locally unresectable ACC.
High recurrence rates have been reported even after curative surgery in ACC[11,18,19].Overall survival rates for localized disease after curative surgery were reported to be 38 mo[18]and 14 mo[24]in patients with synchronous metastases after surgery. The median survival after resection has been reported to be around almost 2 years[7,20,25].
Collective findings reported in the literature indicate that ACC has a better prognosis than pancreatic ductal adenocarcinoma[17]; however, development of effective treatment strategies with surgery and systemic chemotherapy is a critical aspect for improvement of survival rates. Furthermore, tumor markers may improve early diagnosis and detection of disease recurrence. Krugeret al[22]were the first to describe serum lipase as a marker for prognosis and treatment efficacy in ACC; they showed repeated lipase measurements to monitor the dynamics in 5 patients.
Here, we report the case of a patient with metastatic ACC and pancreatic panniculitis that highlights the dynamics of serum lipase in the individual course of the disease and its value for diagnosis and detection of relapse.
CASE PRESENTATION
Chief complaints
A 72-year-old man was referred to the hospital of the Ludwig-Maximilians-University(Munich, Germany) to address an isolated complaint of abdominal pain.
History of present illness
The patient reported that the abdominal pain had appeared that day and denied chronicity or any other symptoms.
History of past illness
There was no history of past illness.
Physical examination
The physical examination revealed a biologically unremarkable patient in good condition, with only diffuse abdominal pain during palpation.
Laboratory examinations
Routine laboratory tests were unremarkable, except for serum lipase, which was elevated (5580 U/L) and prompted suspicion of ACC.
Imaging examinations
Initial imaging examination with computed tomography (CT) detected tumoral growth of the pancreatic head (Figure 1A) and synchronous liver metastases(Figure 1B).
FINAL DIAGNOSIS
We presented the case in multidisciplinary expert consultation, which resulted in a diagnosis of pancreatic ACC with synchronous liver metastases. The consensus recommendation was an up-front surgical treatment.
TREATMENT
Two-stage surgery was performed, consisting of a pylorus-preserving pancreatoduodenectomy first and right hemihepatectomy 9 d later. After the second surgery, the patient’s serum lipase showed a decrease to 432 U/L. The diagnosis of ACC in the pancreas and the liver was confirmed by pathology. There were no histopathological findings of pancreatitis in the corresponding pancreas tissue.
OUTCOME AND FOLLOW-UP
After complete resection of the primary and liver lesions, adjuvant chemotherapy(fluoropyrimidine S-1) was initiated. At 9 mo after the surgery, however, an increase of the serum lipase (to 2384 U/L) was detected. Subsequently, staging diagnostics were performed and hepatic recurrence was found by CT scan (Figure 2). There were no typical signs of pancreatitis as pancreatic inflammation, peripancreatic fluid collection, fluid collections, retroperitoneal air or necrosis. Consequently, a modified FOLFOX6 chemotherapy protocol was recommended.
At 10 mo after the initial operation, a further increase of the serum lipase (to 8414 U/L) was detected when tests were prompted by erythema suspicious for panniculitis occurred in both legs (Figure 3). Shortly thereafter, the patient developed necrosis in the lower extremities, which was accompanied by a sharp increase in the serum lipase level (to 10949 U/L). At 1 year after the surgery, arthritis presented in the patient’s left elbow and another increase in serum lipase (of 13340 U/L) was detected (Figure 4). At this time, panniculitis also appeared on the patient’s facial skin and serum lipase reached its highest level (of 19940 U/L) (Figure 5). Meanwhile, there was no relation between the serum lipase levels and the tumor marker levels of carcinoembryonic antigen (CEA) and CA19-9 during follow-up (Figure 5). The patient has passed away 12 mo after first presentation.
DISCUSSION
A systematic search of PubMed and the Cochrane Library was performed according to the PRISMA guidelines[26]. Medical Subject Headings (commonly known as MeSH)were used as search terms and included “Panniculitis” (MeSH) and “Acinar Cell Carcinoma” (MeSH). A Boolean operator (“AND”) was used to combine the mentioned search terms. Additionally, reference lists were searched for relevant literature. Publications in any language other than English, published before 1995 or without ACC of the pancreas were excluded from further analysis.

Figure 2 Computed tomography at 9 mo after surgery showing hepatic progression of the disease. The patient’s bloodwork showed lipase of 2384 U/L, amylase of 61 U/L, C-reactive protein of 13.1 mg/dL, and leukocytes of 4.98 G/L. A and B: Multifocal filiae of the liver with hypovascular metastases(arrows), and tumor infiltration of the abdominal wall dorsally of the liver. Of note, compared with pancreatic ductal adenocarcinoma[48], the tumor density of the acinar cell carcinoma in the non-contrast phase and time attenuation curve pattern are different but both tumor entities tend to be hypodense in the contrast-enhanced phases; C: Portal venous phase of recurrent metastasis with solid and cystic properties (liver segment VII).

Figure 3 Progressive panniculitis with fat necrosis in the lower extremities at 10 mo after surgery. The patient’s bloodwork showed lipase of 8414 U/L, amylase of 82 U/L, C-reactive protein of 5.2 mg/dL, and leukocytes of 5.41 G/L. A-C: Erythema suspicious for panniculitis occurred in both legs.
The literature search revealed a total of 23 publications, out of which 4 written in non-English language and 3 not reporting data on pancreatic manifestations were excluded. In three[24,27,28]of the sixteen publications[2,3,24,27-39], lipase values corresponding to the clinical course of the patients were described (Table 1). Eight publications showed no correlation between the level of serum lipase and the clinical course[24,27-30,33,37]; these papers described high levels of serum lipase at the stage of diagnosis or surgery but without further assessment of laboratory values.
The current knowledge on ACC of the pancreas is based on publications of small case series[19]. If feasible, up-front surgery is recommended[40]. For our case, we performed a two-stage resection of the primary tumor of the pancreas and its hepatic metastases[17,41]. Al-Haderet al[42]endorse resection of the sites of metastasis, to provide better overall survival than that seen in patients without resection.
Evidence for adjuvant chemotherapy is scarce and can only be deduced from small case series[18-23,43]. Yooet al[19]proposed oxaliplatin-based regimens which may offer a higher efficacy than gemcitabine monotherapy. They showed improved progressionfree survival in patients treated with the common FOLFOX- and FOLFIRINOX regimen, respectively[19]. Among the literature, oxaliplatin-based regimens are most commonly used in cases of metastatic ACC of the pancreas[19,22]. Richardet al[44]have described a case of response of pancreatic ACC to anti-endothelial growth factor receptor (EGFR) therapy related to EGFR amplification.
Almost 50% of ACC patients present with synchronous metastases at the stage of diagnosis. Nevertheless, there are recurrence rates of up to 72% after curative surgeryof non-metastasized ACC[23]. Thus, up-front surgery remains the recommended treatment option for patients with either metastasized or non-metastasized ACC.Subsequent therapies must also be considered.
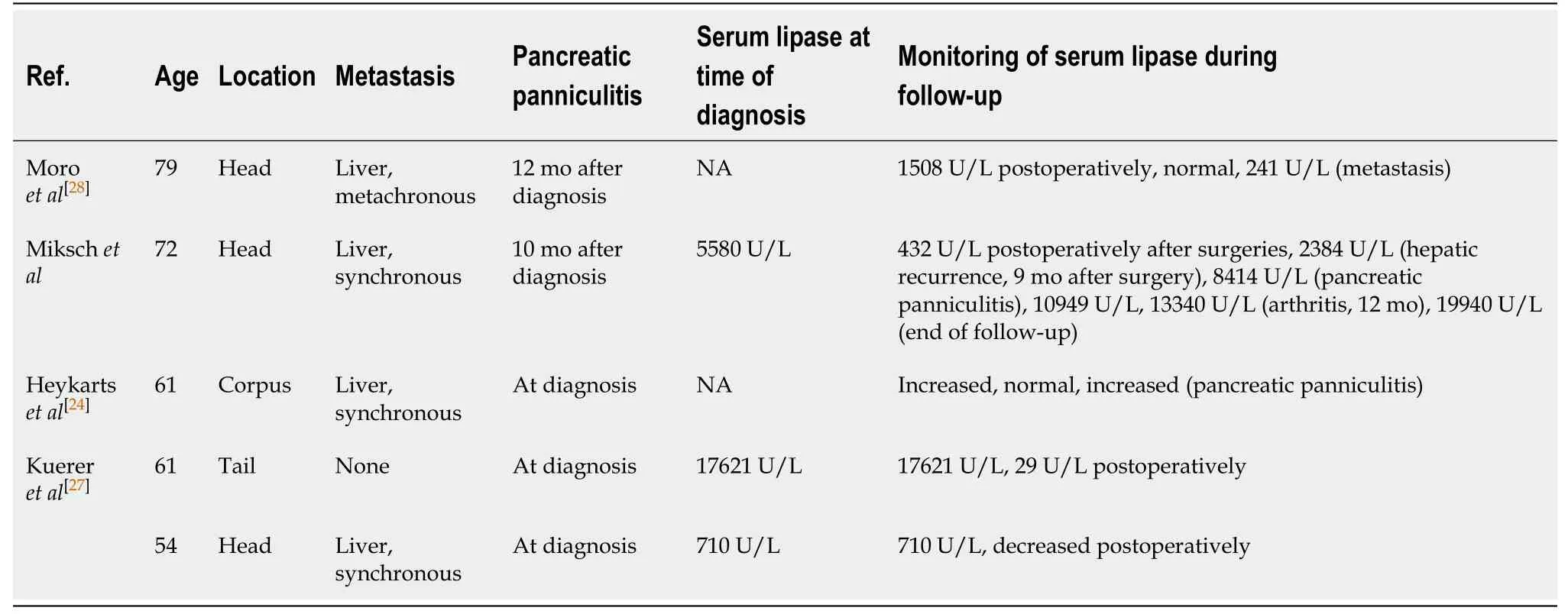
Table 1 Four cases of acinar cell carcinoma of the pancreas associated with pancreatic panniculitis and elevated serum lipase values

Figure 4 X-ray at 12 mo after surgery showing acute arthritis of the left elbow with epicondylitis (arrow). The patient’s bloodwork showed lipase of 13410 U/L, amylase of 22 U/L, C-reactive protein of 22.3 mg/dL, and leukocytes of 10.2 G/L.
Pancreatic panniculitis as an extra-pancreatic manifestation and most frequently described in cases of ACC[7,8].It usually affects the lower extremities[31,45],where most subcutaneous tissue is located. The occurrence of pancreatic panniculitis varies from patient to patient. Herein, we have described a patient with pancreatic panniculitis at almost 1 year after primary surgery. This is similar to the findings of Ferriet al[46]and Zhanget al[47], who reported occurrence of pancreatic panniculitis with serum lipase values of 3885 U/L and 27575 U/L, respectively; neither of those case reports mentioned abdominal symptoms at that time of elevated serum lipase. The combination of subcutaneous panniculitis and elevated serum lipase may be an important clue to suspect recurrent ACC at follow-up[12].
Our patient presented a combination of clinical symptoms with panniculitis and polyarthritis without signs of pancreatitis in several CT scans. Whereas Ferriet al[46]showed that half of the reviewed 64 cases with PPP syndrome occurred in patients with pancreatic ductal adenocarcinoma, whereas 34 cases were reported for patients with pancreatitis.
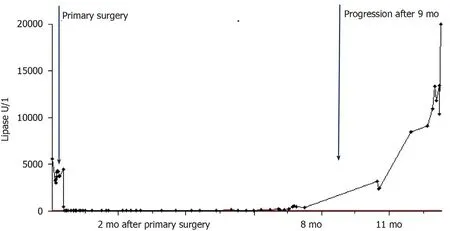
Figure 5 Dynamics of serum lipase levels starting before surgery and during follow-up. The maximal concentration of lipase was 19940 U/L, of Creactive protein was 22.9 mg/dL, and leukocytes was 11.2 G/L. The carcinoembryonic antigen (CEA) an CA19-9 tumor marker levels were collected during follow-up as well: CEA 1.5 ng/mL and CA19-9 13.3 U/mL (first surgery), CEA 1.7 ng/mL and CA19-9 10.2 U/mL (6 mo after primary surgery), CEA 1.7 ng/mL and CA19-9 9.9 U/mL (9 mo after primary surgery).
Impact of serum lipase on the pathogenesis of the PPP syndrome has been verified in mouse models[10]. The systemic pancreatic enzyme secretion causes systemic fat necrosis, especially in subcutaneous fat tissue[35].In all reported cases, an exceptionally high level of lipase was found. Other pancreatic enzymes, such as amylase,phosphorylase and trypsin, may play a role in the development of a hyperlipasemia syndrome, itself consisting of fever, arthralgia, rash, nodular panniculitis, and hypereosinophilia[9-11].The clinical symptoms of fever, arthritis, and pancreatic panniculitis were detected in our patient during disease progression of the ACC.
For the case presented herein, the serum lipase correlated closely with the clinical course of ACC and pancreatic panniculitis. In this respect, disease progression was detected postoperativelyviaincreasing levels of the serum lipase and subsequent radiological detection by CT scan. As demonstrated by our and other cases, serum lipase might indeed be a good tumor marker of disease progression in ACC[22,24,28].
CONCLUSION
In our case of synchronous metastasized ACC, serum lipase was a reliable marker for tumor diagnosis, recurrence, and progression. Therefore, measurement of serum lipase may help to predict prognosis and monitor the individual course of the disease in ACC patients.
 World Journal of Clinical Cases2020年21期
World Journal of Clinical Cases2020年21期
- World Journal of Clinical Cases的其它文章
- Strategies and challenges in the treatment of chronic venous leg ulcers
- Peripheral nerve tumors of the hand: Clinical features, diagnosis,and treatment
- Treatment strategies for gastric cancer during the COVID-19 pandemic
- Oncological impact of different distal ureter managements during radical nephroureterectomy for primary upper urinary tract urothelial carcinoma
- Clinical characteristics and survival of patients with normal-sized ovarian carcinoma syndrome: Retrospective analysis of a single institution 10-year experiment
- Assessment of load-sharing thoracolumbar injury: A modified scoring system
