Analysis of 234 cases of colorectal polyps treated by endoscopic mucosal resection
Lu Yu, Na Li, Xiao-Mei Zhang, Tao Wang, Wei Chen
Lu Yu, Xiao-Mei Zhang, Tao Wang, Wei Chen, Department of Gastroenterology, Maanshan Central Hospital, Maanshan 243000, Anhui Province, China
Na Li, Department of Gastroenterology, Affiliated Hospital of Southeast University, Nanjing 210009, Jiangsu Province, China
Abstract BACKGROUND Colorectal polyps refer to all neoplasms that protrude into the intestinal cavity.Researchers believe that 50%-70% of colorectal cancers originate from adenomatous polyps.AIM To investigate the endoscopic morphologic features, pathologic types, and clinical situation; evaluate the efficacy and safety of endoscopic mucosal resection (EMR);and guide clinicians in their daily practice.METHODS Two hundred thirty-four patients who underwent EMR in our hospital from January 1, 2018 to December 31, 2019 were recruited. Data including sex, age,endoscopic morphology of the polyps, and pathological characteristics were analyzed among groups.RESULTS A total of 295 polyps were resected from the 234 subjects enrolled in the study, of which 4 (1.36%) were Yamada type I. There were 75 (25.42%) type II, 101 (34.24%)type III, and 115 (38.98%) type IV adenomas. Among them, 41 were nonadenomas, 110 were low-risk adenomas, 139 were high-risk adenomas, and 5 were carcinomas. The differences in distribution were not statistically significant,with P values greater than 0.05. The risk of cancer significantly increased for polyps ≥ 1 cm in diameter (c2 = 199.825, P = 0.00). Regarding the endoscopic morphological features, congestion, erosion, and lobulation were more common on the surface morphology of high-risk adenomas and cancerous polyps (c2=75.257, P = 0.00), and most of them were Yamada types III and IV. In all, 6 of the 295 polyps could not be removed completely, with a one-time resection rate of 97.97%. There were two cases of postoperative bleeding and no cases of perforation, with an overall complication rate of 0.09%.CONCLUSION Colorectal polyps ranging from non-adenomatous polyps, low-risk adenomas,and high-risk adenomas to adenocarcinomas each has their own endoscopic features, while EMR, as a mature intervention, has good safety and operability and should be promoted clinically, especially at the primary care level.
Key Words: Colorectal polyp; Endoscopic mucosal resection; High-risk adenoma; Risk factors; Adenocarcinomas; 1,4-bis (diphenylphosphino) butane
INTRODUCTION
Colorectal polyps refer to all neoplasms that protrude into the intestinal cavity.Researchers believe that 50%-70% of colorectal cancers originate from adenomatous polyps[1]. The development process of colorectal cancer is normal mucosa, to epithelial cell hyperplasia, to tubular adenoma, to villous adenoma, to early cancer and finally to invasive carcinoma, and this evolution process takes approximately 8-15 years[2].
The early detection and treatment of colorectal polyps, especially endoscopic treatment of high-risk adenoma, can effectively reduce the incidence of colorectal cancer. Endoscopic mucosal resection (EMR) refers to the operation for complete removal of the diseased mucosa under endoscopy. It is a treatment method developed by combining endoscopic polypectomy and endoscopic submucosal injection[3].Endoscopy is an optional diagnostic tool. Radical surgery can also be considered.Surgery aims to diagnose and treat mucosal lesions through mass excision of part of the mucosa (up to the depth of the submucosal tissue). Since its introduction in 1973,EMR has been developed for decades and is currently a safe and effective method for treating polyps in the large intestine[4,5].
This article will retrospectively analyze the sex, age, endoscopic morphological characteristics, pathological types, and clinical conditions of 234 patients treated with EMR admitted to the hospital from January 2018 to December 2019, to understand the clinical characteristics of different types of colorectal polyps and the safety and efficacy of EMR treatment.
MATERIALS AND METHODS
Basic information
We selected 234 patients undergoing EMR treatment from January 2018 to December 2019 in our hospital. Of the 234 subjects enrolled in the study, 171 were male, with a mean age of 62.2 ± 11.9 years, and 63 were female, with a mean age of 60.9 ± 10.6 years.A total of 295 polyps were removed. Clinical data such as sex, age, polyp size, location,morphology, and pathological type were collected for retrospective analysis.
Research method
Patients confirmed with polyps under endoscopic and successful EMR treatment with complete clinical data, such as endoscopic and pathological reports were included.Patients with intestinal obstruction, familial hereditary polyposis, intestinal tuberculosis, or inflammatory bowel disease and those with incomplete clinical data were excluded.
Grouping method
The selected research subjects were divided into non-adenomatous polyps, low-risk adenoma, high-risk adenoma, and adenoma canceration groups according to the Chinese colorectal cancer screening, early diagnosis and treatment, and comprehensive prevention consensus[6]. Those with one of the following three items were considered to have high-risk adenoma: Polyps or lesions ≥ 1.0 cm in diameter;Villous adenoma or mixed adenoma with villous structures exceeding 25.00%, and high-grade epithelium. Statistical analysis was conducted for variables such as sex,age, and endoscopic and pathological features of polyps.
Devices and medicines
Equipment: OLYMPUS CV-290 electronic colonoscope, OLYMPUS ESG-100 highfrequency electric transmitter, COOK ASM-1-S snare, Nanjing minimally invasive disposable endoscope injection needle, Nanjing minimally invasive ROCC-D-26-195 Titanium clip. Intestinal medicine: Compound polyethylene glycol electrolyte powder(Sutaiqing).
Treatment method
The patients were asked to discontinue anticoagulant and antiplatelet medications 1 wk before surgery, start a low residue or no residue diet 3 d before surgery, and take one box of Sutex the night before surgery and 750 mL warm water. Three packs of Sutaiqing and 2250 mL warm water were taken orally on the morning of the examination, followed by water fasting. Signed informed consent was obtained. The lends were smoothly inserted to reach the ileocecal region, and then the lens was withdrawn to observe the ileocecal region, ascending colon, transverse colon, sigmoid colon, and rectum to determine the endoscopic features of the polyps treated with EMR and to administer 1:10000 epinephrine submucosal injections at the base of the polyps. A sodium chloride solution was administered, good lifting was observed, a loop device was used to encircle the polyp, and then high-frequency electricity was used to completely remove the polyp. The wound was closed as appropriate with titanium clips. Clamping or high-frequency electrocautery were applied.Postoperatively, the patients were instructed to stay in bed, initiate a liquid diet, eat a residue-free diet for 1 wk after surgery, and abstain from strenuous exercise.
RESULTS
Clinical and endoscopic characteristics of the study subjects
A total of 295 polyps were resected, of which 219 (74.24%) were from males and 76(25.76%) polyps were from females. The lesions were classified as follows: Type I: 4(1.36%); Type II: 75 (25.42%); Type III: 101 (34.24%); Type IV: 115 (38.98%). Under endoscopy, Yamada classified the raised lesions in the stomach into four types according to their morphology, regardless of their nature: Type I: Mound-shaped, and the raised part is smooth without a clear boundary; Type II: Hemispherical shape, with a definite boundary in the uplifting part; Type III: The uplift is slightly smaller,forming Yati; and Type IV: The uplift has an obvious pedicle[7,8]. All 295 polyps were divided into four groups according to Yamada type for analysis: The age differences and distributions of polyps were not statistically significant among groups (P> 0.05).Type I and type II polyps more commonly had a diameter of 0.5-0.9 cm, while the number of type III and type IV polyps with diameter > 1.0 cm increased gradually (χ2=463.381,P= 0.000). Type III and Type IV polyps had significantly more congestion,erosion, roughness, and lobulation on the surface morphology than type I and II lesions (χ2= 46.935,P= 0.000, Table 1).
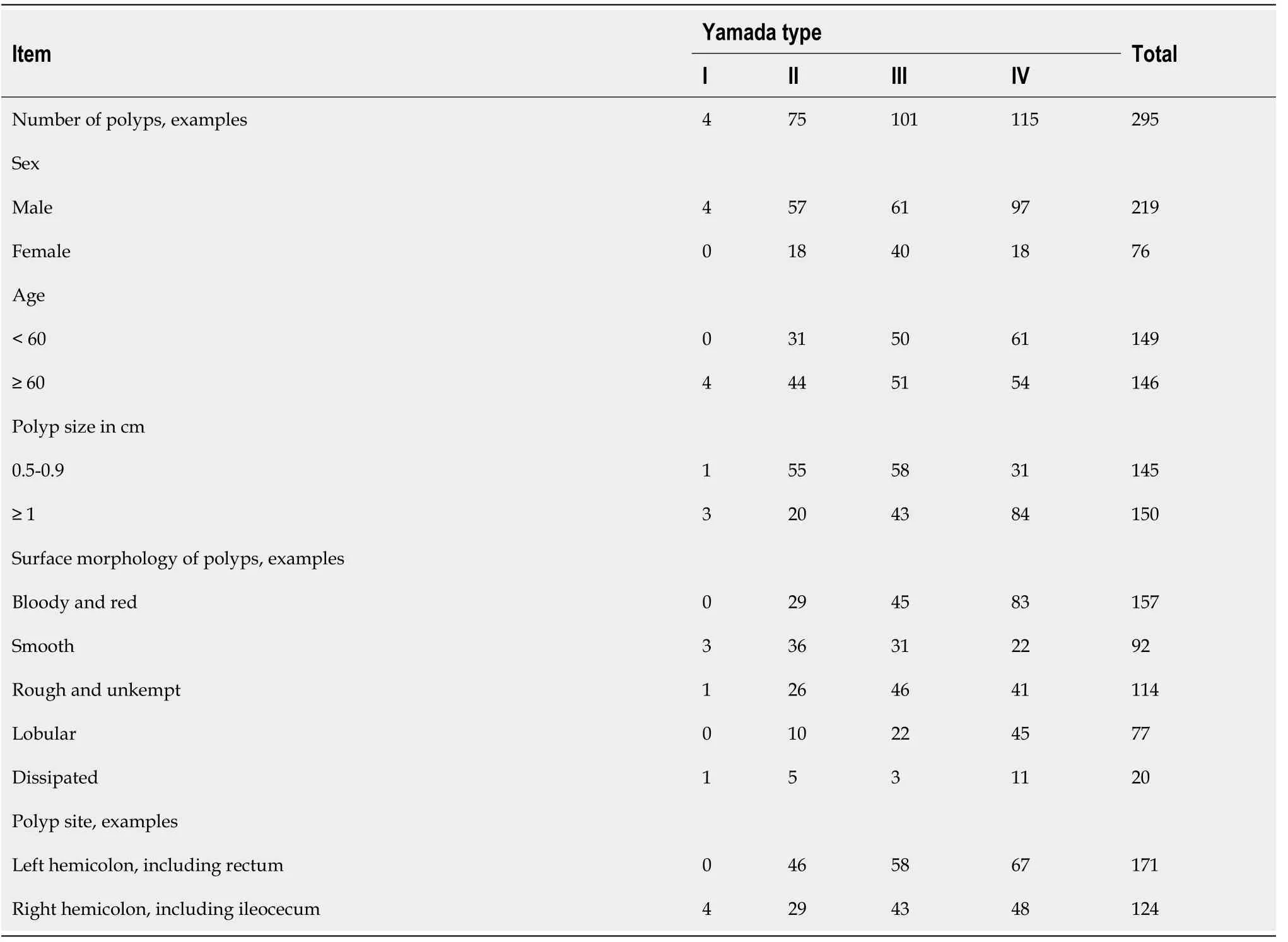
Table 1 Comparison of clinical characteristics and endoscopic features
Risk factor analysis for colorectal polyps
A total of 295 polyps comprising 41 non-adenomas, 110 low-risk adenomas, 139 highrisk adenomas, and 5 carcinomas were classified by sex, age, polyp size, and distribution in the large intestine. There were no statistically significant differences in gender, age and distribution in the large intestine, and thePvalues were greater than 0.05. The risk of polyps ≥ 1 cm in diameter was significantly elevated (c2= 199.825). All five cancerous polyps in the study subjects were polyps ≥ 1 cm in diameter, the largest being approximately 3 cm in diameter. The smallest one was approximately 1 cm in diameter. A total of 128 polyps ≥ 1 cm were found among the high-risk adenomas,accounting for 92.09% of all high-risk adenomas, while the smallest polyp was approximately 1 cm in diameter. There were only 5 polyps ≥ 1 cm among the low-risk adenomas, accounting for 4.55% of all low-risk adenomas (Table 2).
Comparing endoscopic morphological features, congestion, erosion, and lobulation were more common on the surface morphology of high-risk adenomas and cancerous polyps (χ2= 75.257,P= 0.00) and mostly Yamada types III and IV than on other polyps(Table 3).
EMR efficacy and complications
In all, 6 of the 295 polyps were incompletely excised, with remnants of adenomatous or cancerous tissue in the incision, and margin 2.03% of the total. Five of them were Yamada type II, one was Yamada type III, two were less than 1 cm in diameter, four were ≥ 1 cm in diameter, and the largest one was 2 cm in diameter. If the pathology was adenoma, the patient underwent secondary endoscopic argonplasmacoagulation or high-frequency electrotherapy; if the cancerous tissue remained, additional surgical treatment was provided after surgery. During follow-up, there were two cases of postoperative hemorrhage. Both of these cases occurred in males with high-risk adenomas, one with a Yamada type II polyp and one with a Yamada type IV polyp,with diameters of 2 cm and 4 cm, respectively. Endoscopic hemostasis was successfully performed. There were no cases of perforation or infection in any of the enrolled subjects.
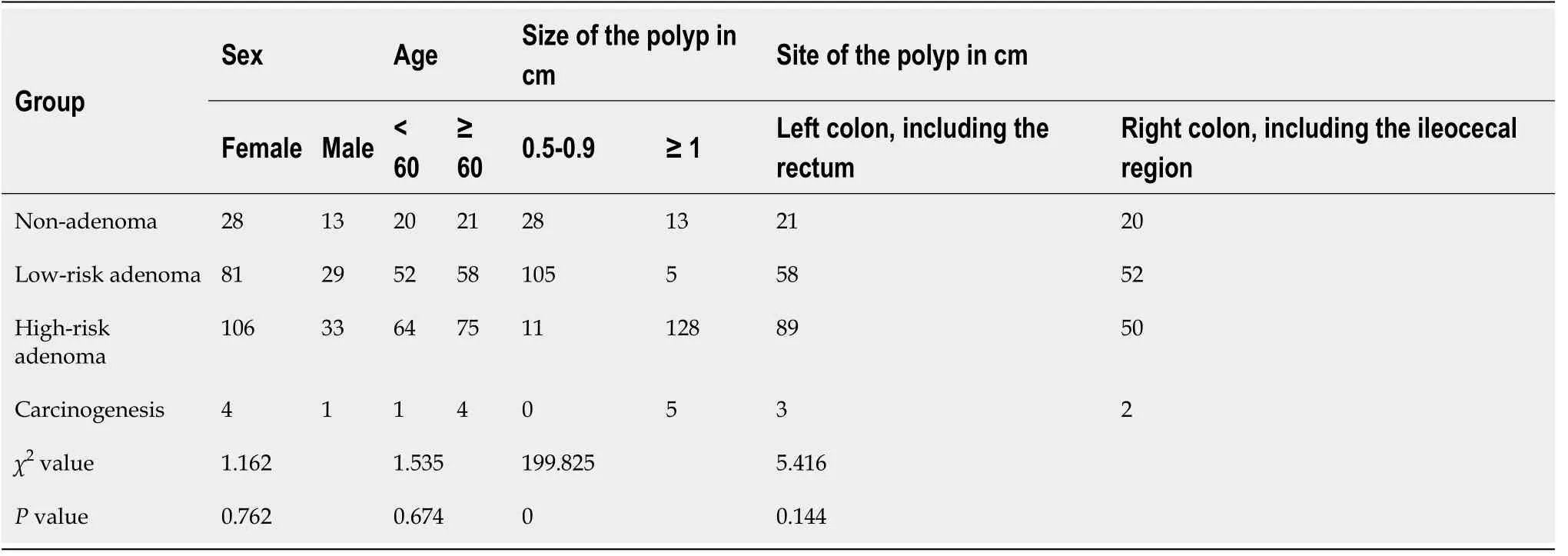
Table 2 Comparison of general clinical conditions of each group

Table 3 Comparison of morphological characteristics of each group under endoscopy
DISCUSSION
Colorectal polyp is a generic term for all superfluous growths, both tumorous and non-tumorous, that protrude into the intestinal cavity. The former are closely related to carcinogenesis and are precancerous lesions, accounting for 70%-80% of colorectal polyps, with a cancer rate of 1.4%-9.2%[9]. The timely resection of colorectal polyps,especially high-risk adenomas, can effectively halt the polyp carcinogenesis process.
A total of 295 polyps were removed from 234 patients in this study, of which 139 high-risk adenomas were removed, accounting for approximately 47.12% of all polyps.Among them, 128 polyps ≥ 1 cm were found, accounting for 92.09% of all high-risk adenomas, higher than similar reports in which high-risk adenomas accounted for 17.08% of the total samples[10,11], which is associated with the use of argon and highfrequency electrotherapy for polyps less than 1.0 cm in diameter in this center. There were no significant differences in gender, age, or polyp distribution among the four groups studied, but another study[12]showed that in the left half of the large intestine,the incidence of high-grade neoplasia and early cancer was higher than that in the right colon, and further studies and discussions are still needed. All five cancerous polyps in the study subjects were polyps ≥ 1 cm in diameter, with the largest being approximately 3 cm in diameter and the smallest being approximately 1 cm in diameter. The number of polyps ≥1 cm among high-risk adenomas was 128,accounting for 92.09% of all high-risk adenomas. There were only five polyps ≥ 1 cm among low-risk adenomas, accounting for 4.55% of the total number of low-risk adenomas. High-risk adenomas and cancerous polyps more commonly showed congestion, erosion, and lobulation on the superficial morphology (c2= 75.257,P=0.00), and most of them were Yamada types III and IV[13]. This is similar to the report from Fukamiet al[12]. Type III and type IV colorectal polyps with a diameter of ≥ 1 cm and superficial congestion, erosion, and lobulation can be considered to have a higher risk of cancer than other types of polyps. For polyps smaller than 1 cm, endoscopic white light + blue light imaging of the three basic areas (surface/pits/vessels) of each description and polyp grading showed good accuracy and confidence[14].
Perforation of the gastrointestinal tract, infection and bleeding are the three most common complications of colorectal polyp treatment[15]. Bleeding was divided into intraoperative and delayed postpolypectomy [bleeding during surgery and bleeding after surgery,1,4-bis(diphenylphosphino)butane]bleeding[16].There were no cases of perforation or infection in this study, and there were two cases of postoperative bleeding, with an overall complication rate of 0.09%, which is lower than that in similar reports[11]. The two patients who developed 1,4-bis (diphenylphosphino)butane were both male and had high-risk adenomas, and bleeding occurred on the 2ndpostoperative day. They had endoscopic Yamada classifications of type II. The polyps had diameters of 2 cm and 4 cm and endoscopic hemostasis was achieved. Some studies have shown that polyps with diameters > 10 mm[17], polyps with a clitoris,adenomatous polyps and intraoperative bleeding are the most common causes of bleeding after endoscopic resection of colorectal polyps and should be considered risk factors for delayed bleeding[18]. In contrast, other studies have shown that sex is an independent risk factor for bleeding from colorectal polyps, with men being more prone to bleeding than women[19]. Patients with a history of hypertension, polyps ≥ 10 mm in diameter, and polyps located in the right hemicolon are prone to delayed bleeding after endoscopic resection. Endoscopists should be more vigilant when treating such patients and should routinely use titanium clips to close the wound during surgery and observe the patient's stool after surgery. Changes in vital signs such as heart rate, abdominal signs and blood pressure should be noted in cases of postoperative bleeding. If abnormal, endoscopic titanium clip to stop bleeding or spray or inject to stop bleeding[20]. A total of 6 of the 295 polyps were incompletely excised, with residual adenomatous or carcinomatous tissue in the incision margin(2.03% of all polyps). The rate of single resection was 97.97%, which is similar to that in relevant reports[21]. Failed endoscopic resection of colorectal polyps is related to a number of factors, which can be summarized as follows: 1) operator skill—those who have a preliminary mastery of EMR fail to perform endoscopic resection proficiently;2) inadequate exposure of the endoscopic polyps—a variety of factors such as overly large polyps, inadequate intestinal preparation, and poor polyp location can lead to inadequate exposure of endoscopic polyps and a limited field of view; and 3)underestimation of the submucosal depth of the polyps, especially for polyps > 2 cm in diameter and Yamada type II and lateral growth polyps, whose histology can invade the muscle and even the plasma membrane layer, rendering EMR impossible[22]. Polyps should be evaluated by ultrasound endoscopy before surgery[23].
CONCLUSION
In summary, colorectal polyps range from non-adenomatous polyps, low-risk adenomas, high-risk adenomas to adenocarcinomas, and each type has its own endoscopic characteristics. EMR is a mature intervention that has good safety and operability and is worth promoting clinically, especially at the primary care level.
ARTICLE HIGHLIGHTS
Research background
The early detection and treatment of colorectal polyps, especially endoscopic treatment of high-risk adenoma, can effectively reduce the incidence of colorectal cancer. Endoscopic mucosal resection (EMR) refers to the operation for complete removal of the diseased mucosa under endoscopy.
Research motivation
Endoscopy is an optional diagnostic tool. Radical surgery can also be considered.Surgery aims to diagnose and treat mucosal lesions through mass excision of part of the mucosa (up to the depth of the submucosal tissue).
Research objectives
Investigate the endoscopic morphologic features, pathologic types and clinical situation, evaluate the efficacy and safety of endoscopic mucosal resection EMR ‰,and guide clinicians in their daily practice.
Research methods
In total, 234 patients who underwent EMR in our hospital from January 1, 2018 to December 31, 2019 were recruited. Data including sex, age, endoscopic morphology of the polyps, and pathological characteristics were analyzed among groups.
Research results
A total of 295 polyps were resected from the 234 subjects enrolled in the study, of which 4 (1.36%) were Yamada type I. There were 75 (25.42%) type II, 101 (34.24%) type III, and 115 (38.98%) type IV adenomas. Among them, 41 were non-adenomas, 110 were low-risk adenomas, 139 were high-risk adenomas, and 5 were carcinomas. The differences in distribution were not statistically significant, withPvalues greater than 0.05. The risk of cancer increased significantly for polyps ≥ 1 cm in diameter (c2=199.825,P= 0.00). Regarding the endoscopic morphological features, congestion,erosion, and lobulation were more common on the surface morphology of high-risk adenomas and cancerous polyps (c2= 75.257,P= 0.00), and most of them were Yamada types III and IV. In all, 6 of the 295 polyps could not be removed completely, with a one-time resection rate of 97.97%. There were two cases of postoperative bleeding and no cases of perforation, with an overall complication rate of 0.09%.
Research conclusions
Colorectal polyps ranging from non-adenomatous polyps, low-risk adenomas, and high-risk adenomas to adenocarcinomas each has their own endoscopic features, while EMR, as a mature intervention, has good safety and operability and should be promoted clinically, especially at the primary care level.
Research perspectives
Endoscopic mucosal resection is becoming the preferred method of polyp treatment.
 World Journal of Clinical Cases2020年21期
World Journal of Clinical Cases2020年21期
- World Journal of Clinical Cases的其它文章
- Strategies and challenges in the treatment of chronic venous leg ulcers
- Peripheral nerve tumors of the hand: Clinical features, diagnosis,and treatment
- Treatment strategies for gastric cancer during the COVID-19 pandemic
- Oncological impact of different distal ureter managements during radical nephroureterectomy for primary upper urinary tract urothelial carcinoma
- Clinical characteristics and survival of patients with normal-sized ovarian carcinoma syndrome: Retrospective analysis of a single institution 10-year experiment
- Assessment of load-sharing thoracolumbar injury: A modified scoring system
