Exploration on Integrative Traditional Chinese and Western Medicine Strategy for Treating Patients of Lung Cancer over 80 Years Old
SUN Ling-yun (孙凌云), XU Yun (许 云), YANG Yu-fei (杨宇飞)
1. Oncology Department, Xiyuan Hospital, China Academy of Chinese Medical Sciences,Beijing, 100091, China
ABSTRACT Lung cancer incidence and mortality are much higher among elderly patients over 80 years'old. However, surgery, chemo and radiotherapy, target therapy all are refined in treating this population.This article summarized 3 types of over 80 years' old elderly cancer patient in real world, which include:1. advanced non-small cell lung cancer that cannot be tolerated by targeted therapy; 2. Suspected lung malignancies for which a clear pathological diagnosis cannot be obtained; 3. Advanced lung cancer with distance metastasis at first diagnosis. The current paper summarized real cases from YANG Yu-fei at Xiyuan Hospital and her traditional Chinese medicine treatment methods and experiences to guide further clinical practice were discussed and shared.
KEYWORDS Elderly; lung cancer; integration of traditional Chinese and Western medicine; Real world;Explore ideas
DISEASE CHARACTERISTICS OF ELDERLY LUNG CANCER PATIENTS OVER 80 YEARS OLD
Lung cancer is currently the first malignant tumor in China with morbidity and mortality[1]. With the aging of China's population, the average age of onset of lung cancer has now surpassed 65 years and continues to rise, with the highest mortality rate among elderly lung cancer patients over 80 years of age[2]. The elderly patients with lung cancer suffer from a decline in body function, often with underlying diseases, and poor tolerance to surgical trauma. The incidence of postoperative arrhythmia is reported to be 60.6%[3].
At present, clinical trials have confirmed that single-agent chemotherapy and targeted therapy can benefit with elderly patients, but the clinical study age is mostly included between 65 and 80 years old. Elderly patients with lung cancer over 80 years old still lack sufficient evidence-based regulatory treatment[4]. In addition, social and ethical issues such as family members and patients personal willingness to treat, psychological state, family relationship, and life value also play an important role in the treatment decision of elderly patients with lung cancer[5]. Studies have shown that functional scores are a major factor affecting elderly patients with lung cancer[6], so improving quality of life, rehabilitation, and palliative support are key goals to focus on.
This article summarized the treatment thoughts and strategies of integrated traditional Chinese and Western medicine by YANG Yu-fei, the chief physician of the tumor diagnosis and treatment center in our hospital by summarizing the characteristics of the 3 typical types of lung cancer patients over 80 years old in the real world, in order to provide reference for actual clinical work. It is mainly aimed at the above-mentioned groups of integrated traditional Chinese and Western medicine. The cases adopted in this article have been obtained the informed consent by the patients and their families.
TYPE I: TARGETED THERAPY INTOLERABLE ADVANCED NON-SMALL CELL LUNG CANCER
Typical Cases
Ms LI is 80 years old. Her first consultation was on July 14th, 2011. Multiple nodules of the left lung were found due to pneumonia in January 2010.Later review revealed that the left lung nodules continued to increase. Then she performed a left upper lobe resection in People's Hospital in April 2011. Postoperative pathology: mucoid bronchial alveolar cancer could not be excluded. Symptoms at first diagnosis: left oppression in chest, tightness,oppression in chest, lumbago, poor appetite, cold stomach bloating, bitter taste in mouth, thin stools,poor sleep, previous years of depression, pale tongue with thick yellow fur, and pulse string.
Traditional Chinese physician diagnosis:internal cancer, liver stagnation, spleen deficiency,lung deficiency, internal sputum stasis. Prescription:Trichosanthes hisrilowii (Quan Gua Lou) 30 g,Bulbus Allii Macrostemonis (Xie Bai) 10 g, Rhizoma Pinelliae Preparata (Qing Ban Xia) 10 g, Astragalus mongholicus Bunge (Sheng Huang Qin) 15 g,Rhizoma Polygonati (Huang Jing) 10 g, Herba Rhodiolae (Hong Jing Tian) 10 g, Radix Asparagi(Tian Dong) 10 g, Radix Ophiopogonis (Mai Dong) 10 g, Radix Adenophorae (Nan Sha Shen)10 g, Radix Glehniae (Bei Sha Shen) 10 g, Radix Pseudostellariae (Tai Zi Shen) 30 g, Poria (Fu Ling) 10 g, Rhizoma Atractylodis (Cang Shu) 10 g,Rhizoma Atractylodis Macrocephalae (Bai Shu)10 g, Endothelium Corneum Gigeriae Galli (Jin Nei Ji) 15 g, Jiao Sanxian 30 g, stir-frying Fructus Setariae Germinatus (Chao Gu Ya) 10 g, Herba Hedyotis (Bai Hua She She Cao) 15 g, Selaginella doederleinii Hieron (Shi Shang Bai) 10 g, Panax pseudo-ginseng (San Qi Fen) 3 g, Ramulus Cinnamomi (Gui Zhi) 6 g, Radix Paeoniae Alba (Bai Shao) 10 g. After taking 14 doses of medicines,oppression in chest was relieved, and chest CT was reviewed 2 weeks later: local postoperative changes in the left lung, small lung nodules, and metastasis? The nature of mediastinal lymph nodes is to be determined, and the symptoms are the same as before. In September 2011, she was admitted to our ward for comprehensive treatment of traditional Chinese medicine, and given intravenous injections of Chinese patent medicne, such as Aidi injection and Kanglaite injection to benefit qi and dispel stasis, and Chinese medicine dietetic therapy, foot bath, and five-element music therapy were combined. In October of the same year, the patient started oral gefitinib treatment, and she had abnormal liver function after taking it for 41 days.Modern Chinese pharmacological herbs Herba Abri and Herba Sedi were added. On February 23th,2012, her liver function was normal. Gefitinib was discontinued in January 2014 due to abnormal liver function.
Since then, the patient has been admitted to our hospital for comprehensive treatment of traditional Chinese medicine every 4 months and rechecked, with stable condition. In September 2016, the patient developed liver metastases and was not specifically targeted for tumor treatment.She continued to be treated with comprehensive traditional Chinese medicine. In April 2017, the patient developed symptoms such as nocturia,dreaminess, and tinnitus. And she changed to take modifed Liuwei Dihuang Decoction. The last visit was in September 2017. The patient's KPS score was 70, and her general condition was OK.
Targeted Therapy and Adverse Reactions in the Elderly with NSCLC
The emergence of molecularly targeted drugs has provided new treatment strategies for elderly with non-small cell lung cancer[7]. The first representative dermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKI) include gefitinib,erlotinib, and ectinib. Among them, the phase II clinical trial of gefitinib monotherapy for advanced NSCLC aged75 years shows that gefitinib monotherapy can be used as first-line treatment for elderly with advanced NSCLC[8]. The adverse reactions of targeted drug therapy are lighter than those of chemotherapy, mainly rash, diarrhea, and pneumonia[9].
Traditional Chinese medicine treatment can reduce the adverse reactions of targeted therapy[10],and can also reverse drug resistance mechanism[11].For this kind of patients, asymptomatic liver damage caused by targeted therapy, clinical studies suggest that 9.4% of patients withdrawn from the test due to drug-related toxicity, and 1.9% were caused by elevated 3-4 degree aminotransferases, and liver toxicity It is also a major cause of discontinuation[12].Chinese herbal medicines can play a certain role in protecting liver function. It is necessary to reduce the burden of liver detoxification, and the use of Chinese patent medicines should be minimized.
Coping Strategies for Comprehensive Treatment of Traditional Chinese Medicine
Comprehensive treatment of traditional Chinese medicine is one of the concepts of comprehensive treatment of tumors proposed by Professor YANG Yu-fei 20 years ago. The concept is that under the guidance of the basic theory of traditional Chinese medicine, based on dialectical treatment,combining syndrome differentiation with disease differentiation, combining with modern science and technology, and using various traditional Chinese medicine treatment methods in a planned and rational way to maximize the overall treatment of traditional Chinese medicine advantages, and to strive for the full treatment of tumors.
Its immediate goal is to combine with Western medicine tumor treatment, to alleviate adverse reactions, to improve symptoms, to control tumor progression, and the long-term goal of treatment is to extend the effective survival time. In-patient comprehensive treatment cannot only be comprehensively reviewed to evaluate the efficacy, but also can be combined with traditional Chinese medicine comprehensive diet therapy,foot bath, external application, acupuncture therapy, and music therapy to help patients improve their quality of life[13].
TYPE II: SUSPECTED MALIGNANT LUNG SPACE WITH NO CLEAR PATHOLOGICAL DIAGNOSIS
Typical Cases
Ms ZHAO, was 86 years old. The initial consultation time was July 28th, 2014. A chest CT scan was performed on the patient after a fall on July 20th, 2014. The soft tissue density of the lower lobe of the left lung can be seen, and multiple calcifications can be seen. The bronchus of the lower lobe was stretched, and the enlarged lymph can be seen in the mediastinum. Lung cancer was not excluded. Patients and their families hoped that pure traditional Chinese medicine treatment was used because the patient was old.
Symptoms at the first diagnosis: dry cough, no sputum, fatigue, shortness of breath, and acceptable appetite, 1 stool day, 1-2 times of nocturia, red tongue, less moss, and thick yellow moss. Western medicine diagnosis: left lung occupancy (malignant tumors to be excepted); traditional Chinese physician diagnosis: internal cancer, lung and kidney deficiency, internal phlegm and blood stasis.
Chinese medicine prescription: Radix Asparagi(Tian Dong) 10 g, Radix Ophiopogonis (Mai Dong)10 g, Radix Adenophorae (Nan Sha Shen)10 g,Radix Glehniae (Bei Sha Shen) 10 g, Cortex Mori(Sang Bai Pi) 10 g, Cortex Lycii (Di Gu Pi) 10 g,Poria (Fu Ling) 10 g, Fructus Ligustri Lucidi (Nv Zhen Zi) 10 g, Echinacea (Han Lian Cao) 10 g,Endothelium Corneum Gigeriae Galli (Jin Nei Ji)10 g, 30 g each of stir-frying three Xian, stir-frying Fructus Setariae Germinatus (Chao Gu Ya) 10 g,dried Radix Stemonae (Zhi Bai Bu) 10 g, Rhizoma Zingiberis 6 g, Ramulus Euonymi Alatis 15 g, Salvia chinensis Benth 15 g, Selaginella doederleinii Hieron 15 g, Rhizoma Polygonati 15 g; Chinese patent medicine prescription: Weimaining Capsule,and Bailing Capsule. After 2 weeks of follow-up, the tumor marker CA125 (246.6). Cough and fatigue were relieved, and mental strength and appetite improved. The upper part was mainly followed by addition and subtraction with symptoms; If rich sputum, adding Semen Sinapis (Bai Jie Zi), Semen Raphani (Lai Fu Zi), Perilla (Su Zi), if cough add Radix Platycodonis (Jie Geng), Semen Armeniacae Amarum (Xing Ren), and Radix Scutellariae (Zuo Huang Qin) to clear the lung heat, or appropriately modified the anti-tumor Chinese herbal medicines such as Herba Scutellariae Barbatae (Ban Zhi Lian), Hedyotis diffusa Willd (She She Cao) etc.After taking the drug for 1 year, the patient's cough and shortness of breath continued to decrease,and his mental and physical strength gradually recovered. Regular review of tumor markers showed a continuous downward trend, see Figure 1. Chest CT tumors were stable and no progress was seen,see Figure 2. At the end of 2015, she refused to take medicines because of a sudden death of a loved one,with a mental shock. She died of a lung infection after 1 year.
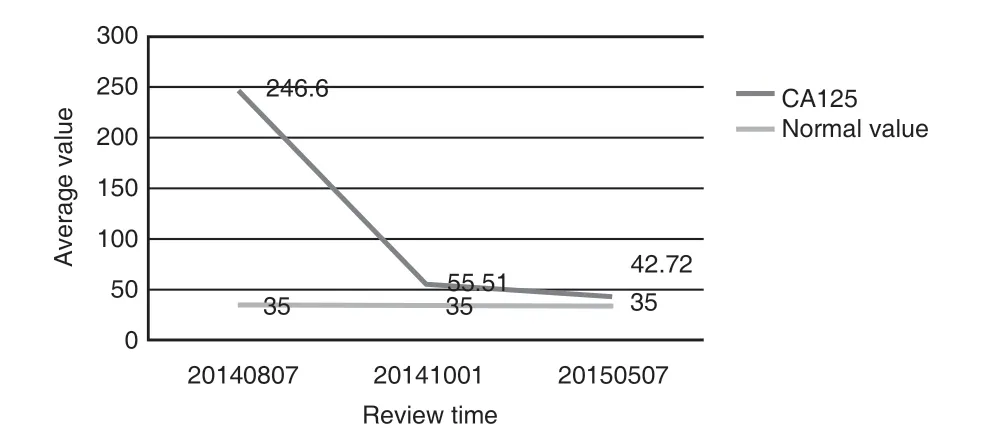
Figure 1. Changes of Tumor markers in Patients During Traditional Chinese Medicine Treatment
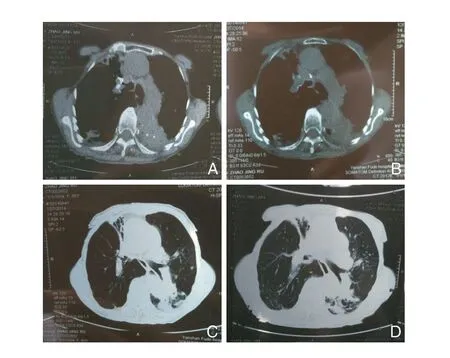
Figure 2. Chest CT Lesions Are Basically Stable During Medication
Common Causes and Countermeasures of Unclear Pathological Diagnosis
The main reasons why elderly patients with lung cancer over 80 years of age cannot obtain a clear pathological diagnosis are: 1. family members or themselves do not want to undergo invasive biopsy; 2. the tumor location is difficult to perform puncture or bronchoscopy biopsy; 3. unable to get clear pathological evidence from sputumin or from pleural fluid. The lack of a clear pathological diagnosis hinders the selection and implementation of subsequent treatment schemes. Coping strategies are as follows: 1. The tumor markers[14]and PET-CT results can be used as a reference to make a rough judgment of the condition; 2. Traditional Chinese medicine treatment was actively used.
Objectives and Strategies of Integrated Traditional Chinese and Western Medicine
The development of overall treatment goals needs to focus on: 1. comprehensive physical fitness status; 2. Comorbidities; 3. patient and family members' willingness to treat and personal conditions(economic, place of residence). For example, patients with the above cases have probles such as mobility,a Karst score of 60, and being far away from Beijing.Based on the wishes of their families, the treatment plan is determined as follows: 1. It is mainly traditional Chinese medicine treatment in the outpatient; 2.Chest CT and tumor markers are the main judgment basis for the condition monitoring; 3. Follow-up visits can be replaced by family members in the form of photos, videos, etc., as far as possible, home rehabilitation and palliative support. If the patient is in good physical condition and has a strong willingness to treat, he can try to find tumor cells through pleural effusion. If possible, bronchial biopsy can be used to further clarify the pathology. Meanwhile, genetic testing is performed. For example targeted therapy can be attempted if it is a mutation target.
The Idea of Supporting the Right by Traditional Chinese Medicine
Professor YANG Yu-fei believes that lung cancer in the elderly is mainly to support lungs qi, and the commonly used formula is Shashen Maidong Decoction. The spleen and stomach are acquried, and the solidifying stomach qi also plays an important role in the treatment. Clinically, Jiao San Xian, stir-fried Fructus Setariae Germinatus(Chao Gu Ya), and Endothelium Corneum Gigeriae Galli (Jin Nei Ji) are often used to stimulate appetite.Elderly lung cancer often suffers from lung and kidney losses. Clinically, it is necessary to add products such as Rhizoma Polygonati (Huang Jing),which can supplement both lung and kidney. If necessary, Fructus Ligustri Lucidi (Nv Zhen Zi) and Han Lian Cao are added, which are not too warm.In addition, these patients need to avoid external feelings in particular, and should be told to take good care of them, and often give them a cold to prepare for occasional needs.
TYPE Ⅲ: ADVANCED LUNG MALIGNANT TUMORS WITH DISTANT METASTASIS AT THE BEGINNING
Typical Case
Mr LI was 83 years old. The first consultation was on September 1st, 2014. The patient developed oppression in chest and cough at the end of June 2014, which continued to aggravate.Chest CT showed mass lesions in the right lower lobe, and abdominal CT showed low-density lesions in the liver S7 segment and low-density lesions in the left kidney. It was considered as the possibility of lung cancer with liver-kidney metastasis. Due to older age, no further Western medical treatment was recommended. Symptoms at first diagnosis: severe fatigue, occasional cough, sputum, white color, sleepiness,unconstrained stools, 2 night up at night, dry throat in the morning, fear of coldness, slow pulse strings, and pale tongue cracks. Past history:hypertension, coronary artery heart disease,emphysema, smoking history for 60 years. The diagnosis was deficiency of lung and spleen,and internal sputum stasis. Prescriptions are as follows: Astragalus mongholicus Bunge (Sheng Huang Qin) 15 g, Codonopsis pilosula (Franch.)Nannf (Dang Shen) 10 g, Rhodiola (Hong Jing Tian) 6 g, Polygonatum (Huang Jing) 15 g, Herba Rhodiolae (Zhi Yuan) 6 g, Radix Asparagi (Tian Dong) 10 g, Radix Ophiopogonis (Mai Dong)10 g, Radix Adenophorae (Nan Sha Shen) 10 g,Radix Glehniae (Bei Sha Shen) 10 g, Ju Hong 10 g, Rhizoma Pinelliae Preparata (Qing Ban Xia)10 g, Rhizoma Acori Tatarinowii (Shi Chang Pu)10 g, Ramulus 6 g (Gui Zhi), Semen Armeniacae Amarum (Xiong Ren) 10 g, stir-frying largehead atractylodes rhizome (Chao Bai Shu) 10 g and Glycyrrhizae (Zhi Gan Cao) 6 g. Ramulus Euonymi Alati (Gui Jian Yu) 15 g, Salvia chinensis Benth (Shi Jian Chuan) 15 g, Selaginella doederleinii Hieron (Shi Shang Bai) 15 g, Rhizoma Fagopyri Dibotryis (Jin Qiao Mai) 15 g. Chinese patent medicines were as follows: Kanglaite Capsule, and Bailing Capsule; Western medicine examination: a full set of tumor markers, and liver and kidney function were checked. After a followup visit in September 2014, the cough and fatigue improved significantly after taking the medicines.Rhizoma Phragmitis (Mao Gen) and Rhizoma Imperatae (Bai Mao Gen) were added 15 g each.On the basis of this formula, the symptoms increased and decreased with symptoms, and the symptoms were significantly relieved. The lesions were stable. He died of a sudden severe illness at the end of 2015.
Coping Strategies for the Elderly Patients with Primary Lung Cancer with Distant Metastases
This type of patients is no longer clinically possible to radically cure tumors, so the main goals of treatment are to alleviate symptoms, improve quality of life, and at the same time delay the rapid progression of the tumor as much as possible. If the patient is accompanied by liver and kidney metastasis, extra care should be taken to protect liver and kidney function. Therefore, Chinese medicines that may cause liver and kidney function damage should be avoided, and liver and kidney function should be reviewed regularly. In the treatment by Chinese medicines, the lungs and kidneys were still used, and the major method was to benefit qi and dissipate phlegm. Rhizoma Polygonati(Huang Jing), Radix Asparagi (Tian Dong), Radix Ophiopogonis (Mai Dong), Radix Adenophorae and Radix Glehniae (Nan Bei Sha Shen) were used to supplement and not dry, while Ramulus Euonymi Alati (Gui Jian Yu), Salvia chinensis Benth (Shi Jian Chuan), and Selaginella doederleinii Hieron (Shi Shang Bai) were used to clear heat, resist tumors and to delay the rapid tumor progression. For elderly patients with lung cancer with bone metastases,attention should be paid to preventing falls and fractures, and to avoid traditional Chinese medical treatments such as massage and Chinese traditional manipulation.
Traditional Chinese Medicine Treatment Ideas of Eliminate Pathogenic
The "pathogenic" in the theory of traditional Chinese medicine is not completely equivalent to the tumor body itself in modern medicine. The pathogenic qi of patients with lung cancer is mainly manifested in fire stasis and cold phlegm. ① Clear fire stasis in the lungs is also pathogenic qi, so the Cortex Lycii (Di Gua)and Cortex Mori (Sang Bai Pi) are commonly used in clinical practice to clear the fire stasis in lungs; ② Dissolve cold phlegm: the lung is the sputum storage device, and the lung tumors are mostly the fire stasis leading to sputum. Long-term sputum coagulation, the stagnation of vicioussputum lead to cold phlegm,so it is necessary to pay attention to dissolving cold phlegm, and add Pericarpium Citri Reticulatae(Chen Pi), Rhizoma Pinelliae (Ban Xia), Ju Hong,Rhizoma Arisaematis Cum Bile (Dan Nan Jing),Bulbus Fritillariae Thunbergii (Zhe Bei Mu) etc. ③Application of anti-tumor Chinese herbal medicines:In clinical practice, the "timely" flexible application of anti-tumor Chinese medicines are emphasized,such as Herba Scutellariae Barbatae (Ban Zhi Lian),Herba Hedyotis (Bai Hua She Cao), and Selaginella doederleinii Hieron (Shi Shang Bai) etc. When adding such drugs of clearing fire and removing toxicity, we must pay attention to protecting the stomach qi and supplementing the products with warmth.
SUMMARY
At present, traditional Chinese medicine intervention in the treatment of non-small cell lung cancer has formed a standardized system.For example, in the Department of Oncology of Guang'anmen Hospital it was summarized that the clinical path of integrated traditional Chinese and Western medicine for elderly lung cancer,and calculated the core prescription of traditional Chinese medicine[15], which was in accordance with the core clinical prescriptions of YANG Yu-fei.The comprehensive assessment of the elderly and palliative treatment has also attracted attention in the treatment of lung cancer with integrated traditional Chinese and Western medicine in recent years[16]. Recent studies have shown that the use of traditional Chinese medicine interventions and targeted therapy are independent factors related to the prognosis of elderly patients with advanced non-small cell lung cancer[17]. The median survival of elderly patients (over 80 years old) with advanced lung cancer alone can reach 18 months,while the combined treatment of traditional Chinese and Western medicine can reach 23 months[18]. Therefore, it is of great clinical value to formulate individualized Chinese and Western medicine diagnosis and treatment programs for this specific population. The characteristics of the typical cases listed in this article are the actual situations often encountered in real-world clinics,but they are often outside the scope of modern medicine diagnosis and treatment scope. Through the above analysis and summary, combined with Professor YANG Yu-fei's clinical experience and ideas, it is hoped that it will provide some guidance and reference for the problems that are more difficult in actual clinical work and take the advantages of integrated traditional Chinese and Western medicine.
 World Journal of Integrated Traditional and Western Medicine2020年2期
World Journal of Integrated Traditional and Western Medicine2020年2期
- World Journal of Integrated Traditional and Western Medicine的其它文章
- Systematic Review and Meta-Analysis of Hugan Tablets(护肝片) in the Treatment of Drug-Induced Liver Injury
- Systematic Evaluation (Meta-analysis) of the Efficacy and Safety of Pudilan Xiaoyan Oral Liquid (蒲地蓝消炎口服液) in the Treatment of Suppurutive Tonsillitis in Children
- Clinical Study on the Treatment Efficacy of Cerebral Hemorrhage with Xingnaojing Injection in Real World
- New Year's Message
