Factors associated with metastasis in superior mesenteric vein lymph node in subtotal gastrectomy for gastric cancer:Retrospective case control study
Won Ho Han,Jungnam Joo,Bang Wool Eom,Keun Won Ryu,Young-Woo Kim,Myeong-cherl Kook,Hong Man Yoon
1Center for Gastric Cancer,Research Institute &Hospital,National Cancer Center,Goyang-si 410-769,Republic of Korea;2Division of Cancer Epidemiology and Prevention,National Cancer Center,Goyang-si 410-769,Republic of Korea
Abstract Objective:The revised Japanese treatment guideline for gastric cancer recommends dissection of the superior mesenteric vein lymph node (No.14v LN) if there is metastasis in infrapyloric lymph node (No.6 LN).However,it is still controversial whether LN dissection is necessary.The aim of this study was to investigate the factors associated with metastasis in No.14v LN.Methods:Patients who underwent D2 lymphadenectomy between 2003 and 2010 were included.We excluded patients who underwent total gastrectomy,had multiple lesions,or had missing data about the status of metastasis in the LNs that were included in D2 lymphadenectomy.Clinicopathologic characteristics and the metastasis in regional LNs were compared between patients with No.14v LN metastasis (14v+) and those without (14v−).Results:Five hundred sixty patients were included in this study.Univariate analysis showed that old age,larger tumor size,tumor location,differentiation,lymphatic invasion,venous invasion,perineural invasion,T classification,and N classification were related to metastasis in No.14v LN.Multivariate analysis showed differentiation (P=0.027) and N classification (P<0.001) were independent related factors.Metastasis in infrapyloric lymph node (No.6 LN) and proxiaml splenic lymph node (No.11p LN) was independently associated with metastasis in No.14v LN.Conclusions:Differentiation and N classification were independent factors associated with No.14v LN metastasis,and No.6 and No.11p LN metastasis were independent risk factors for No.14v LN metastasis.
Keywords:Gastric cancer;gastrectomy;lymphadenectomy;superior mesenteric vein;risk factor
Introduction
D2 lymphadenectomy has been a standard treatment for treating gastric cancer (1-3).However,the extent of D2 lymphadenectomy is controversial.The additional dissection of the para-aortic lymph nodes (LNs) shows no survival benefit (4,5).The superior mesenteric vein lymph node (No.14v LN) is a gateway to the para-aortic LNs (6).however,it is still controversial whether LN dissection provides survival benefit.
In the past,the Japanese treatment guideline for gastric cancer (2nd edition) included resection of No.14v LN in D2 lymphadenectomy (7).The gastrocolic trunk and the middle colic vein had to be dissected around,resulting in a high risk of vessel injury and bleeding.Because of this,the recently revised Japanese treatment guideline for gastric cancer no longer includes dissection of No.14v LN as part of D2 lymphadenectomy,although it recommends dissection of No.14v LN if there is metastasis in infrapyloric lymph node (No.6 LN) (8).
Several retrospective studies have also reported that patients with No.14v LN metastasis have similar survival compared to those with systemic metastasis (9,10).In contrast,No.14v lymphadenectomy in patients with stage III or higher gastric cancer was associated with survival improvement in some studies (11-13).Therefore,the prediction of No.14v LN metastasis is necessary to determine whether No.14v lymphadenectomy has benefit;however,there has not been much research on this topic.The aim of this study was to investigate the factors associated with metastasis in No.14v LN.
Materials and methods
Patients and inclusion criteria
Patients who underwent D2 lymphadenectomy with No.14v LN dissection for gastric cancer in middle or lower third of the stomach between January 2001 and December 2010 at the National Cancer Center,Korea were included in this study.We excluded patients who underwent total gastrectomy,had multiple lesions,had distant metastasis at the time of operation or had missing data on the status of metastasis in LNs that were included in D2 lymphadenectomy according to the Japanese Classification of Gastric Carcinoma.Dissection of infrapyloric area (No.6 LN) and superior mesenteric vein area (No.14v LN) is shown inFigure 1.
Evaluation of operative outcomes
Preoperative evaluation usually consisted of esophagogastroduodenoscopy with biopsy,abdominopelvic computed tomography,and serum tumor markers.Patients underwent radical subtotal with more than D2 dissection,as defined by the Japanese treatment guideline for gastric cancer.After surgery,patients were followed up regularly according to the routine follow-up schedule for 5 years.Tumors were evaluated as pathologic stage after operation using the Union Internationale Contre le Cancer tumornode-metastasis (TNM) system,7th edition (14).
Clinicopathologic factors of the enrolled patients,including age,sex,tumor size,differentiation,location,Lauren’s classification,lymphatic invasion,venous invasion,perineural invasion,and stage,postoperative complications were retrospectively analyzed.Harvested lymph nodes were classified according to the Japanese treatment guideline for gastric cancer.This study was approved by the Institutional Review Board at the National Cancer Center (No.NCC2017-0271).
Statistical analysis
All analyses were performed using SAS®for Windows®(Version 9.1.3;SAS Institute,Cary,NC,USA).A logistic regression analysis was used to test univariate and multivariate associations between variables to investigate risk factors of No.14v LN metastasis.Continuous variables are presented as median (range) and categorical variables as proportions.Differences between patients with No.14v LN metastasis (14v+) and those without (14v−) werecompared using the Chi-squared test or Fisher’s exact test for categorical variables,andt-test or Wilcoxon rank sum test for continuous variables,as appropriate.Univariate and multivariate logistic regression were conducted to examine the prognostic impact of variables on No.14v LN metastasis.Multivariable logistic regression utilized a backward variable selection method with an elimination criterion of P>0.1.Statistical significance was set at P<0.05.
Results
Patient demographics
Of the 560 patients who underwent D2 lymphadenectomy with No.14v LN dissection,No.14v LN metastasis was pathologically confirmed in 24 (4.3%) patients.Compared to patients without No.14v LN metastasis,patients with No.14v LN metastasis were older (median age 66vs.60 years) and had larger tumors (median 6.5vs.4.0 cm).Differentiation,tumor location,lymphatic invasion,perineural invasion,venous invasion,and T and N classification were significantly different according to No.14v LN metastasis status.Other groups in pathology include mucinous type 27 cases,squamous cell type 3 cases,papillary type 32 cases,hepatoid carcinoma 2 cases.The 14v LN metastasis was rare in early stage,especially in T1 cancer (<1%),but metastasis rate increased to 5%−10% in advanced cancer with T2 or higher T category.In N1 patients,there was no No.14v LN metastasis,but 5% of N2 and 19% of N3 patients had No.14v LN metastasis.Postoperative complication rates and severe complications(>Clavien-Dindo grade II) were not statistically different between the two groups (Table 1).
Risk factors for No.14v LN metastasis
Univariate analysis showed that age,tumor size,histopathological type,tumor location (middle to lower third),lymphatic invasion,venous invasion,perineural invasion,T classification,and N classification were related to metastasis in No.14v LN.Multivariate analysis showed that differentiation (P=0.027) and N classification(P<0.001) were independently related factors (Table 2).
Regional LN metastasis related to No.14v LN metastasis
To analyze the relationship of No.14v LN metastasis with metastasis in other regional LNs,the metastasis in regional LNs and No.14v LN metastasis were compared for each station.The univariate analysis of all LN stations were statistically significantly related to No.14v LN metastasis,except No.1 LN (P=0.055) and No.4sb LN (P=0.493).In multivariate analysis,metastasis in No.6 LN [odds ratio(OR)=8.593,P<0.001]and No.11p LN (OR=6.640,P=0.001) was significantly associated with metastasis in No.14v LN,respectively.There was a marginal increase in the OR when metastasis was found in No.12a LN (OR=3.050,P=0.057).Among 24 patients with No.14v LN metastasis,19 (79.2%),9 (37.5%),and 8 (33.3%) also had metastasis in No.6 LN,No.11p LN,and No.12a LN,respectively(Table 3).
Discussion
In this study,we analyzed the risk factors associated with metastasis in No.14v LN-dissected patients.No.14v LN metastasis was significantly associated with differentiation and N classification.Metastasis in No.6 was the most significant risk factor for No.14v LN metastasis.
No.14v LN dissection is performed for curative resection because 20%−25% of patients with T2 stage or higher have been shown to have No.14v LN metastasis(15,16).However,this study showed a metastasis rate as low as 4.3%.We believe that this is owing to a disproportionate percentage of early-stage patients in our study.About 37.1% of our patients (208/560) were pT1 stage,and 52.5% (294/560) were N0.In other retrospective studies,the No.14v LN metastasis rate was very low in these cohorts:0% in stage I and 1.6% in stage II patients(12).Another study found metastasis rates of 0.6% in T1 patients and 1.2% in N1 patients (10).As mentioned above,due to the adverse effect of No.14v LN dissection and the very low rate of No.14v LN metastasis,No.14v LN is currently not included as part of D2 dissection in the revised Japanese treatment guideline for gastric cancer,and is recommended only when there is metastasis in No.6 LN (8).
In other studies,histologic grade was not associated with No.14v LN metastasis (9,12).However,in this study,histologic grade was a risk factor of No.14v LN metastasis.Although histologic grade is generally known to have little effect on prognosis (17,18),undifferentiated adenocarcinoma increases the risk of LN metastasis in early gastric cancer (19,20).Other types include mucinous type,papillary type and squamous cell type were also associated with 14v metastasis.These pathology types have a relatively poor prognosis than the differentiated type,which maysuggest that it is related to 14v metastasis (21,22).Although the histology was a related factor in the present study,it is not significant in early-stage cancer,since the rate of No.14vLN metastasis is very low (1%).
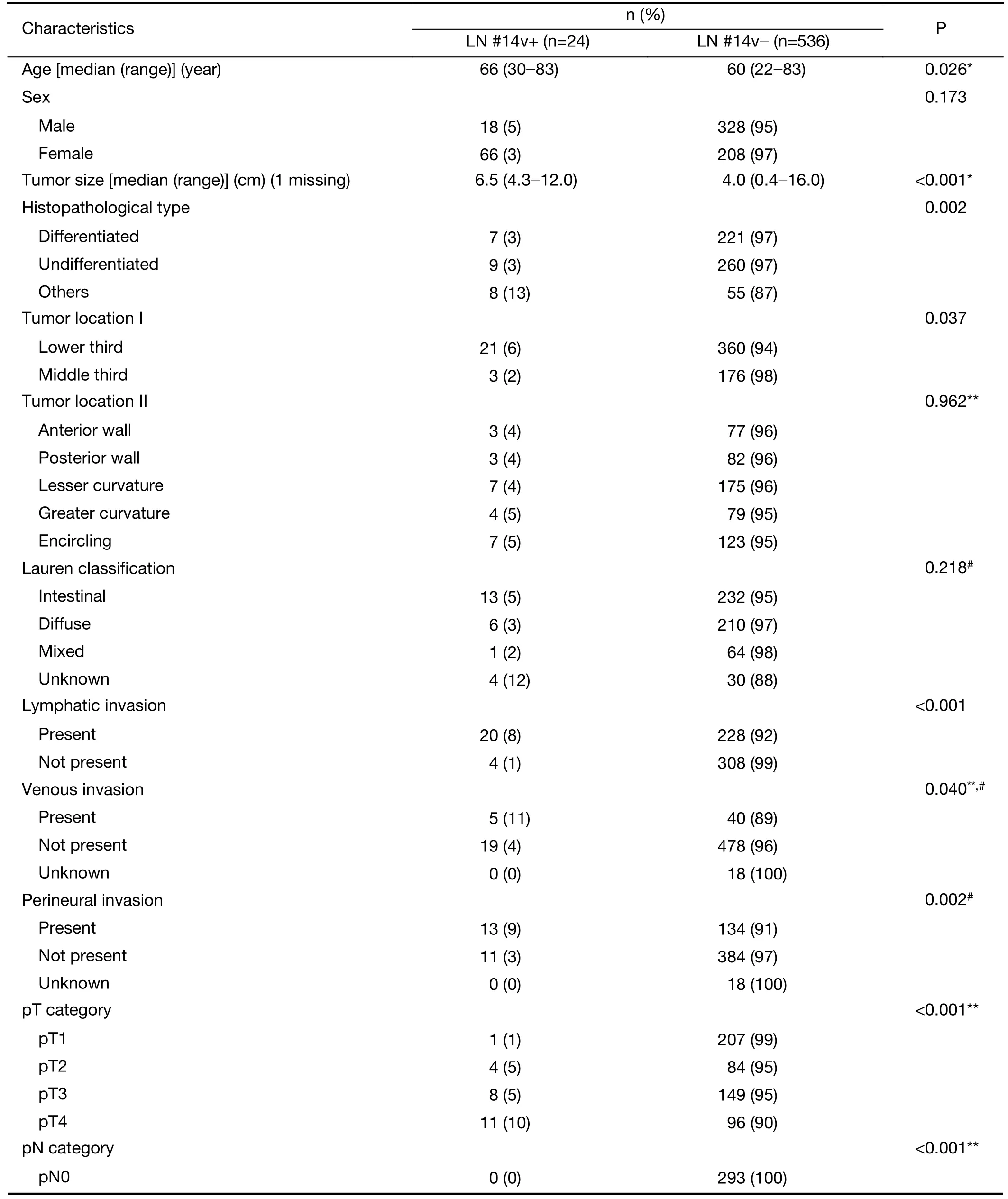
Table 1 Patients’ characteristics
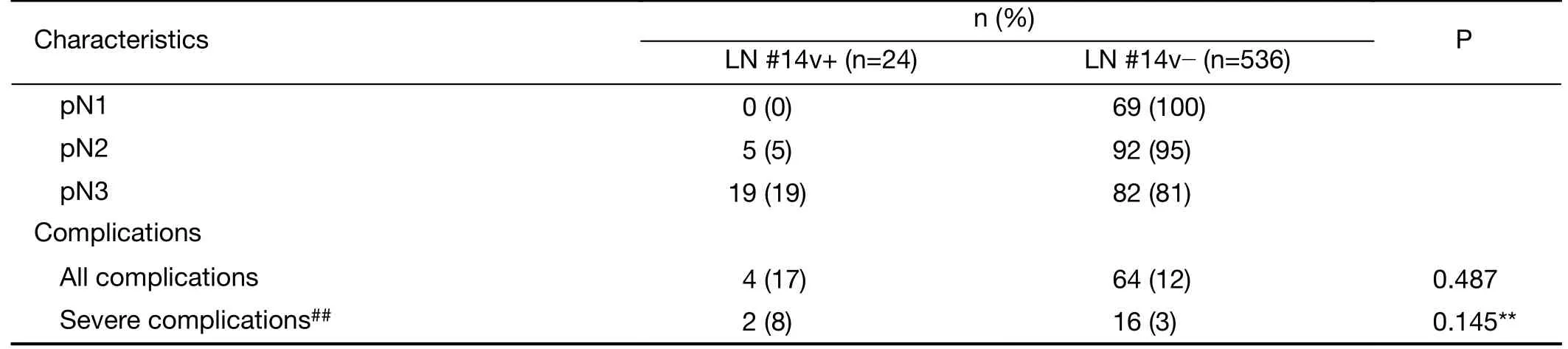
Table 1 (continued)
Since the TNM stage is one of the important risk factors for 14v metastasis and anatomical features of LN station,it is difficult to analyze 14v metastasis except for the N stage.Anatomically,the lymphatic flow of the lower stomach is mainly composed of three lymphatic flows.No.3,No.5 and No.6 LN through No.8a LN and No.6 LN through No.14v LN are known to join at the paraaortic LN (6,23).No.6 LN is reported to be a sentinel LN of No.14v LN metastasis (8).In current study,16.2% (19/117) of patients had No.6 LN metastasis with No.14v LN metastasis,and only 1.2% (5/419) had No.14v LN metastasis without No.6 LN metastasis.
Unlike other retrospective studies,No.11p LN metastasis was also related risk factor for No.14v LN metastasis in our study.Generally,greater curvature lymphatic flow is known to drain into the paraaortic LN via the splenic hilum or around the splenic artery LN.The LNs around the splenic artery are also connected via the lymphatic system along the superior border of the pancreas(24).In a study of the lymphatic flow of pancreatic carcinoma,it was reported that the lymph vessels of the pancreas head could lead to the paraaortic LN through two pathways (through the celiac trunk:No.12a LN−No.9 LN,and through the superior mesenteric LN:No.14v LN) (25,26).Because of this complicated lymphatic anatomy of the pancreas head,it is presumed that metastasis in No.14v LN is related to metastasis in No.11p,No.9 and 12a LN.However,as no other studies have found an association between No.14v LN metastasis and No.11p LN metastasis in gastric adenocarcinoma,further studies are needed.
It is known that there is a risk of bleeding and caution for dissection,there was no difference in complications in the present study.Recently,laparoscopic 14v lymphadenectomy has also been reported and there was no difference in complications between the two groups (27).
Previous study in institution has reported survival results that extended D2 gastrectomy including No.14v LN dissection seems to be associated with improved overall survival of patients with clinical stage III/IV gastric cancer(11).In other studies,there also has reports on relationship between No.14v lymphadenectomy and the survival rate retrospectively (12,13).A randomized multi-centered controlled study is ongoing to examine disease-free survival when dissection of No.14v LN is performed as part of D2 lymphadenectomy (14VIGTORY trial,ClinicalTrials.gov Identifier:NCT 03264807).
The limitation of this study is that firstly it is a retrospective study,and it could be possible that a large number of patients were excluded due to inaccurate classification of LN status,resulting in selection bias.Since the pathologic stage was used,it is not easy to apply the results of the present study to the extent of LN dissection during operation.Second,compared to other previous studies,the number of early-stage patients was relatively higher,resulting in fewer 14v metastasis.the low number of patients with No.14v LN metastasis was also a limitation in the analysis of No.14v LN risk factors.Third,only five patients underwent neoadjuvant chemotherapy and none had 14v LN metastasis in the present study.Neoadjuvant chemotherapy is not a standard therapy for the resectable gastric cancer in this institution,so it is difficult to elucidate the effect of neoadjuvant chemotherapy.
Conclusions
Differentiation and N classification were independentfactors associated with No.14v LN metastasis.Additionally,metastasis in No.6 and No.11p LN were independent risk factors for No.14v LN metastasis.Metastasis in No.6 and No.11p LN may indicate thenecessity of No.14v LN dissection if metastasis is suspected intraoperatively.Further studies are needed to examine the survival benefit of No.14v LN dissection.
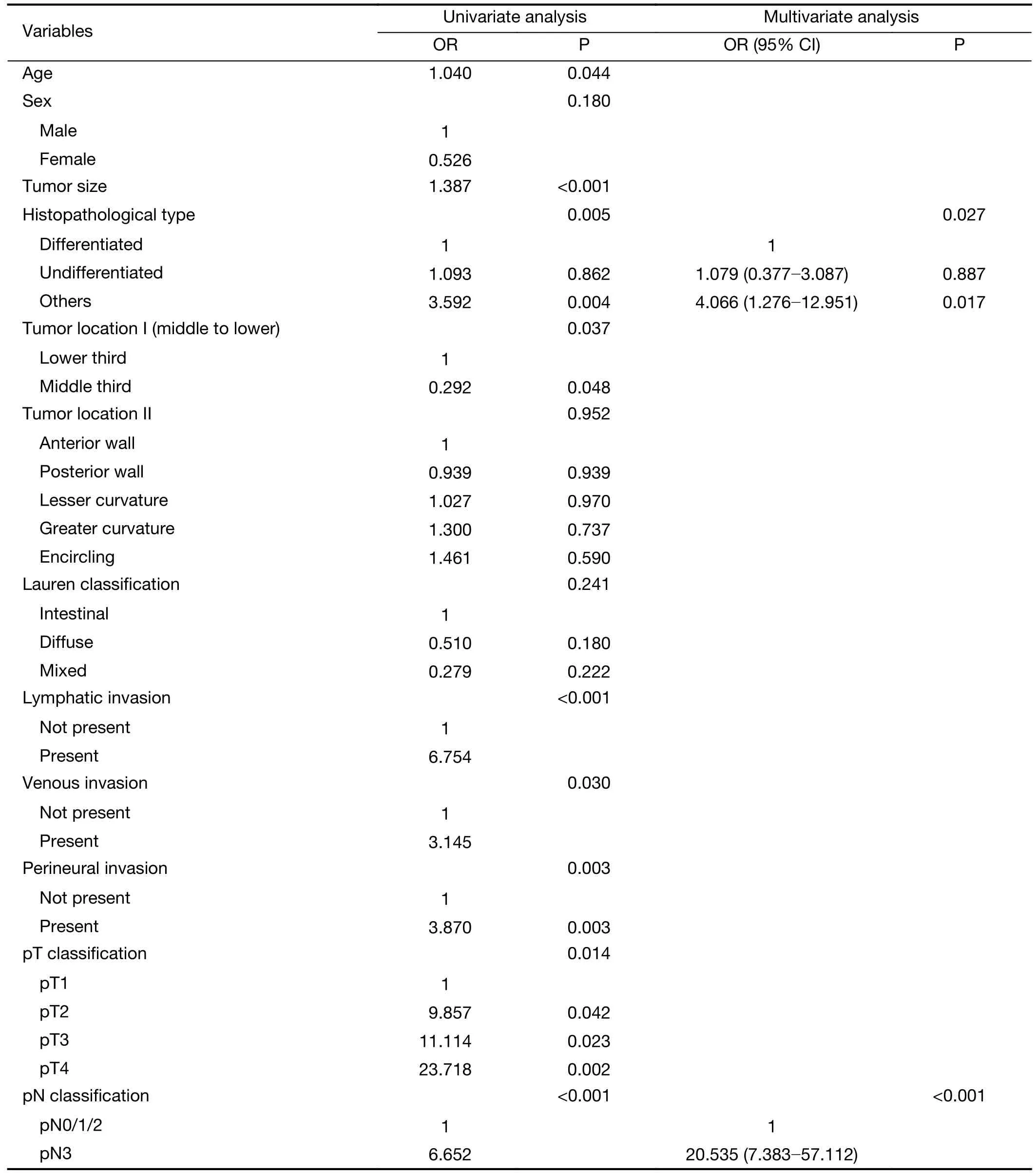
Table 2 Multivariate analysis of risk factor for 14v LN metastasis
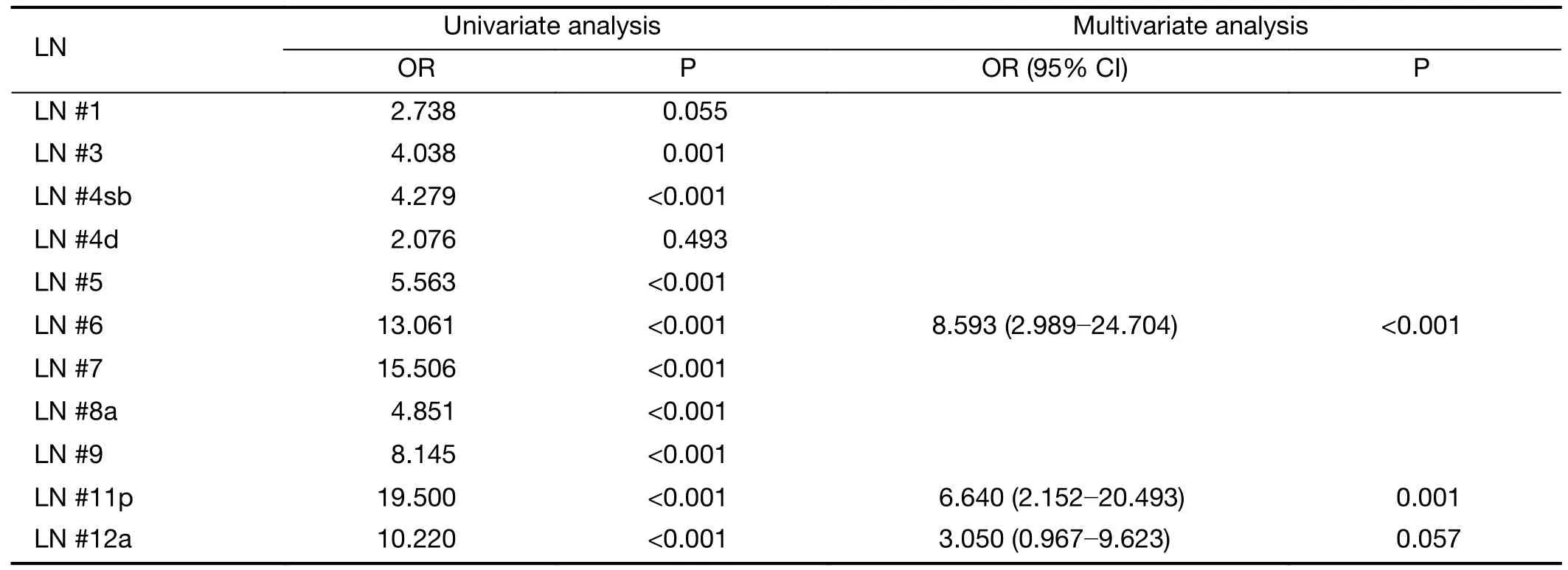
Table 3 Multivariate analysis of regional LN metastasis for 14v LN metastasis
Acknowledgements
This work was supported by the grants (No.1510210,1810320 and 2010360) from the National Cancer Center,Republic of Korea.
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2020年1期
Chinese Journal of Cancer Research2020年1期
- Chinese Journal of Cancer Research的其它文章
- Incidence and mortality of oral and oropharyngeal cancer in China,2015
- Incidence and mortality of laryngeal cancer in China,2015
- Updates on larynx cancer epidemiology
- An exploration for quantification of overdiagnosis and its effect for breast cancer screening
- Effects of neoadjuvant chemotherapy on respiratory function in patients with breast cancer
- Prognostic impact of D2-plus lymphadenectomy and optimal extent of lymphadenectomy in advanced gastric antral carcinoma:Propensity score matching analysis
