lmpact of dental clearance on total joint arthroplasty:A systematic review
Christopher Frey,Sergio M Navarro,Terri Blackwell,Carla Lidner,H Del Schutte Jr
Abstract
Key words: Total knee arthroplasty; Total hip arthroplasty; Total joint arthroplasty;Periprosthetic joint infection; Dental screening
INTRODUCTION
While there have been improvements in total joint arthroplasty (TJA) throughout the years,it is compromised by the risk of periprosthetic joint infection (PJI),the most common cause of total knee arthroplasty (TKA) and total hip arthroplasty (THA)failure[1,2].It is a devastating complication which results in significant patient morbidity.Infected revisions can easily exceed the cost of performing the primary arthroplasty and are projected to total $ 1.62 billion by 2020[3].Key risk factors have been determined,and include poor nutritional status,smoking,inadequate blood sugar control,and poor dental health[4,5,6].Ideally,knowledge of these factors can be used to develop risk mitigation strategies.One potential application is discerning the impact of dental procedures and pathologies on adverse outcomes in TJA.
There exists no absolute criteria or single test to diagnose PJI.Instead,diagnosis is based upon a mixture of lab results,cultures,and clinical findings[7].The implication of a dental source is often based upon both the identification of a pathogen considered to be a constituent of the patient's oral flora at the infection site and the timing of the infection with a seeding procedure[8].This premise is based upon the finding that many events such as dental scaling and brushing one's teeth can cause transient bacteremia when dental pathology is present[9,10].Such reports have been cited when implementing dental prophylaxis in arthroplasty patients prior to dental procedures.Conversely,some orthopedic surgeons recommend that patients receive preoperative prophylactic antibiotics and/or dental clearance before TJA.
Given the lack of overarching guidelines on the role of dental clearance and its association with TJA outcomes,a systematic review was performed using data from primary studies to summarize the prevalence of dental pathology in patients scheduled for TKA and THA and the impact of dental evaluation and necessary interventions on outcomes.
METHODS
The literature search consisted of PubMed and Scopus database inquiries in February 2019 for the impact of dental clearance and the epidemiology of significant dental pathology in potential TJA patients (Figure 1).This was conducted by one author.Search terms consisted of “Arthroplasty AND Dental AND Clearance” and“Arthroplasty AND Dental AND Hygiene” for both databases.This yielded 6 papers that met all of the criteria (Table 1).One additional paper was selected from a review article that resulted from the initial search.Another paper was individually retrieved after the initial screen as it was accepted and published in May.
Literature assessing the association between dental clearance and TJA outcomes were included.Manuscripts examining prevalence of and risk factors for failing dental clearance were included as well.Considering the scarcity of evidence,various summary measures were accepted,with a preference for risk ratios.Only human studies within the last 25 years were included to ensure that the results are applicable.Interventional,case-control,and cross-sectional studies were included.In total,eight studies met criteria.All studies were evaluated for quality and bias using a modified 27 item Downs and Black checklist[11].For the power analysis (item 27),we substituted a simple score of 0 or 1 score.Papers received one point if they included power calculations.We decided to utilize this instrument to evaluate methodological quality because it is validated for both randomized and non-randomized studies.We did not use a formal metric to estimate risk of bias across studies.
After the studies were included,data concerning impact of dental clearance,model used,sample size,methods,results with statistical analysis,and conclusions were extracted by one author and transcribed in a table.This was reviewed by another author for verification.Next,inputs for the methodological quality analysis with the Downs and Black checklist were extracted.
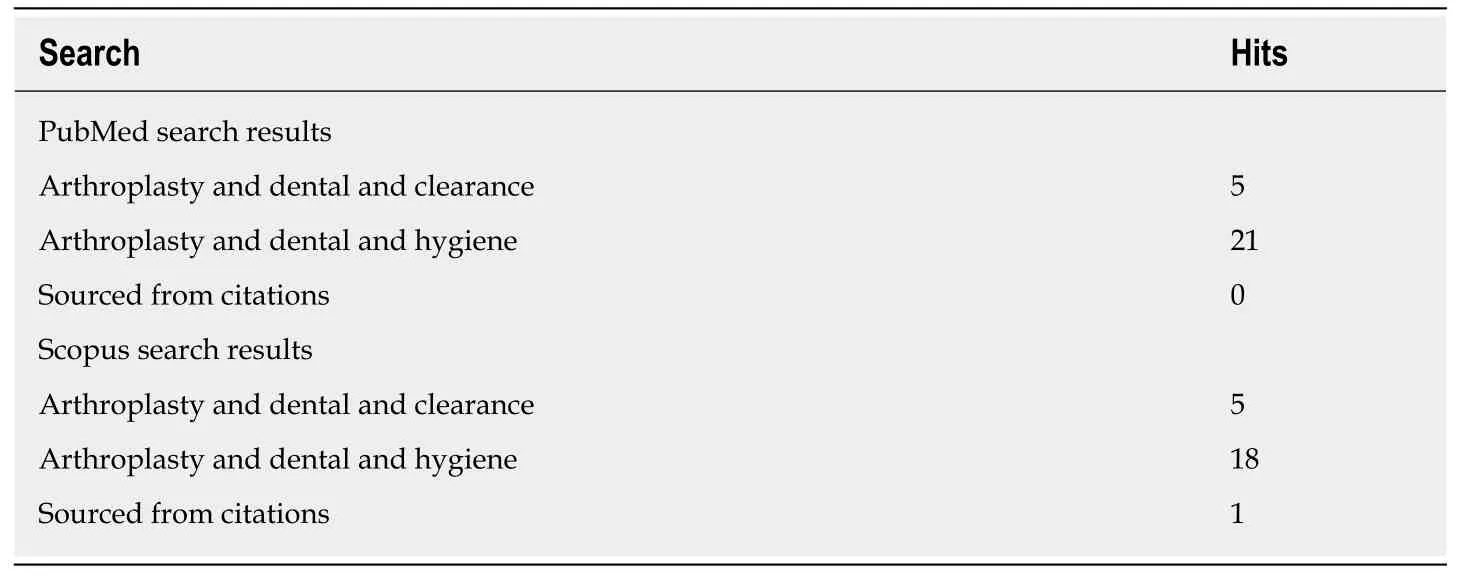
Table 1 PubMed and Scopus search results
RESULTS
Quality assessment
Eight studies were included[12-19].Of the 8,7 (86%) included a dental evaluation performed by a dental professional[12-14,16-19]and five utilized questionnaires or interviews (71%)[13-17].One paper used a questionnaire alone[15].Although papers were selected from peer reviewed publications,2 were not listed on PubMed[15,19].The articles scored between 15 and 23 using our modified DandB checklist (Table 2).The papers were limited by several factors.For instance,none of the selected manuscripts were randomized or blinded,increasing risk of bias.Additionally,many of the papers had small sample sizes,and none demonstrated calculation of power.Lastly,it should be noted that the paper by Barrington and Barrington was designed to capture the primary outcome of dental pathology incidence,not for detecting PJI[16].
Prevalence of periodontal pathology
Four studies focused on the prevalence of dental pathology and/or dental hygiene practices in patients to undergo TJA (Table 3)[12-15].Adamkiewiczet al[12]had dental evaluations performed on patients admitted for TJA preoperative workup in Poland.They found that 28.5% had clinically significant periodontal disease.This compares with 23% in previously published national data[20].There were no significant differences in inflammatory markers or cell counts between the periodontal disease and healthy groups.
Tokarskiet al[13]employed a dental hygiene questionnaire along with a dental evaluation.They found that 12% failed dental clearance,which,in this case,was defined as requiring a tooth extraction or root canal.The number increases to 19%when patients requiring fillings are included.Additionally,they identified that patients with one of three key risk factors (narcotic use,tobacco use,and last dentist visit over one year ago) had a 22% chance of failing the dental evaluation,compared with 6% if they did not have any.
Vuorinenet al[14]also used both questionnaires and dental evaluation in an attempt to determine which patients ought to receive dental clearance based on risk factors.Twenty-nine point four percent of patients failed clearance,34% were found to have moderate gingivitis,and 5.1% of patients had severe periodontitis.This compares with national reports that 27% of Finnish patients had periodontal disease[21].It was found that the only significant risk factors for failing dental clearance were history of root canal,dental visit for symptoms within the last 3 mo,infrequent dental checkups,and tobacco use.Patients with regular examination and no history of root canal were 50% less likely to fail clearance.
Lastly Woodet al[15]used a post-operative dental hygiene survey without professional dental evaluation.They found that patients in general report adequate oral hygiene and 76% having had a dental cleaning within the last year.Only 5%admitted to not having a dentist.
Impact of dental clearance and/or scaling on infection
Four studies measured the impact of preoperative dental clearance on TJA outcomes(Table 4)[16-19].Barrington and Barrington required patients to receive dental evaluation and the appropriate interventions before elective TJA[16].Twenty-three percent were found to have active tooth decay requiring treatment.There were no significant differences between primary and revision groups.Although it was not the primary outcome,there were no infections related to the operation detected within the first 90 d post-operatively in any of the 100 patients.
Lampley and colleagues compared postoperative infections between elective TJA patients who had received dental clearance and hip fracture patients who received THA or hemiarthroplasties who did not receive pre-operative dental clearance[17].Out of the patients who received dental clearance,8.8% required treatment for periodontal disease.There was no significant difference in postoperative infection (less than 6 mo post-op) requiring reoperation.Of the 6 (1.7%) patients with infections in the elective group,only one failed the dental screen.A pathogen was detected in 5 out of the 6 cases.Four (2.5%) patients in the hip fracture group required reoperation for infection concern.Only one patient had an identifiable pathogen.None of the pathogens except,possibly,Peptostreptococcus magnus in the dental clearance group were of likely dental origin.
Taiet al[18]utilized a retrospective data from the National Health Insurance Research Database (NHIRD) to compare TKA patients who required “removal of hardware” plus 7 d of antibiotics within five years of the operation to those who did not.They found that dental checkups and scaling were associated with significantly lower post-operative infection rates.Only 7.1% of the infection group had regular checkup and scaling (5-6 times over last three years) compared to 9.9% in the healthy group.Moreover,73.1% had no visits in the infection group compared to 67.8% in the healthy group.The adjusted OR of PJI when receiving regular checkup and scaling was 0.69 (0.54-0.89) and 0.84 (0.71-0.99) when less frequent.
Sonnet al[19]performed a retrospective review of 2457 patients who underwent primary TJA.Seventy-nine point one percent of these patients received dental evaluation before the operation,however,it appears this was decided on an individualized basis and not based on a predetermined,randomized approach.Complication-free rates at 36 mo were similar between those who did and did not receive dental evaluation.Although not significant,both the dental evaluation and extraction groups appeared more hazardous than the groups that did not have a dental workup [Hazard ratio (HR) = 1.95,P= 0.07 and HR = 1.24,P= 0.57].The rate of PJI was measured to be 1.51%,however this was not compared between groups.

Figure 1 Workflow of PubMed and Scopus database query.

Table 2 Quality assessment based on downs and black questionnaire
DISCUSSION
In this systematic review,we attempted to capture the prevalence of dental pathology and risk factors in populations in consideration for TJA as well as the impact of dental clearance and interventions on the outcomes of TJA procedures.In order to advocate for the institution of these rules,the benefits of pre-operative dental evaluation must outweigh the not-insignificant costs imposed on patients and the healthcare system at a whole.Overall,there is not enough concrete evidence to support dental evaluation for all patients.
We included four studies that paint a picture of dental health of TJA patients.Failure of dental clearance ranged from 8.8%[17]to 29.4%[14].However,the standards for evaluation varied.The criteria used by Tokarskiet al[13]measured failure as requiring tooth extraction or root canal.In fact,when carious lesions are included,failure rates increased from 12% to 19%[13].Similarly,Lampleyet al[17]measured failure as dental pathology necessitating intervention prior to surgery and only found a failure rate of 8.8%.Wood and colleagues detected good overall dental hygiene at a tertiary care center in Canada with 76% having had a dental checkup within the previous 12 mo and only 5% admitting to not seeing a dentist[15].When compared by region,TJA patients in American tertiary care centers had failure rates from 8.8% to 23%[13,16].This is moderately higher than failure rates in Poland (28.5%)[12]and Finland(29.4%)[14].However,it is difficult to pool data do to differences in baseline patient population oral health status and variation in dental evaluation practice.
Two of the studies evaluated risk factors for failing dental clearance.Tokarskiet al[13]found that of several risk factors,patients who had one or more of:Narcotic use,tobacco use,and no dental visit within the last 12 mo had a 22% risk of failure compared to 6% for patients with no risk factors.The authors concluded that it is feasible to exclusively screen those with high risk profiles.However,Vuorinenet al[14]found that tobacco use,history of root canal,dental visit for symptoms,and infrequent dental visits were significant risk factors.Patients with no root canal and regular checkups were less likely to fail,but grouping,as performed in the previous study,did not yield a significantly different risk profile.The authors concluded that they were unable to identify a group of patients who could avoid dental clearance.

Table 3 Risk factors and epidemiology of total joint arthroplasty patients
We identified four papers that detail the impact of dental clearance and/or necessary interventions on the outcomes of TJA,with one of the four finding a significant positive impact of dental clearance and/or evaluation[16,18].Firstly,Barrington and Barrington detected pathology requiring treatment in 23% of patients[16].No periprosthetic joint infections were detected within 90 d of surgery.However,the study was small (n= 100) and not designed to capture the effect of dental evaluations so the results are difficult to interpret.Taiet al[18]found that patients with frequent dental scaling in the previous three years had 31% lower risk of PJI after TKA than those who did not receive scaling.Although these results reflect well upon frequent dental examination and scaling,it does not directly assess the impact of pre-operative dental clearance.In contrast,neither Lampleyet al[17]nor Sonnet al[19]found evidence to support dental evaluations.Although the hip fracture group in the former study had an insignificantly higher reoperation rate (2.5%vs1.7%),hardware was not removed in any of the four cases as no bacterial infection was identified.It should be noted that there were no true controls,follow up was poor in the hip fracture group (18% were deceased),and the threshold for failing clearance was high.Sonnet al[19]actually found higher complication rates in the dental evaluation and extraction groups,although this was not significant.This may be attributed to other confounding health risks not captured by the study.
The results of our systematic analysis are somewhat in line with current recommendations.In the proceedings of international consensus on orthopedic infections,92% of voters agreed that patients with oral disease should receive appropriate interventions before elective TJA to reduce risk of infection despite limited evidence[8].It was proposed that dental screening may be required for high risk patients.76% of voters agreed that dental clearance should not be required for all patients to undergo TJA.Much like how prophylactic antibiotics for common dental procedures in all patients with joint prostheses is falling out of favor,we expect dental clearance protocol to change as new data emerges[22-25].At the moment,we would not recommend for universal dental screening before TJA.
We performed this study to preferred reporting items for systematic reviews and meta-analyses guideline standards,however,there were still several limitations.First and foremost,literature regarding dental clearance for TJA is scarce.Our methods only disinterred four papers capturing the impact of dental evaluation and/or treatment on infections after TJA.Considering the relatively low incidence of periprosthetic infection,few of the studies were adequately powered to detect significance and none were designed as randomized controlled trials.Additionally,there is no common standard for preoperative dental evaluation.Criteria for failing dental clearance ranged from diagnosing dental caries to requiring tooth extraction or root canals.Amongst studies assessing prevalence of dental pathology,differences in location and clinical setting hinder synthesis of data.Lastly,some studies relied on self-reporting of questionnaires and surveys,which incur several inherent biases[26].

Table 4 lmpact of dental clearance on infection
CONCLUSION
With an aging population,the number of total joint arthroplasties is likely to continue growing.Periprosthetic infection remains a great concern and quality improvement problem despite improvements in sterile and prophylactic techniques.There is little evidence to support universal dental clearance before TJA,even for higher risk patients.There remains a need for future research to elucidate the mechanism of periprosthetic infections and more robust analysis of patients with high risk dental pathologies to help guide interventions.
 World Journal of Orthopedics2019年12期
World Journal of Orthopedics2019年12期
- World Journal of Orthopedics的其它文章
- Pilot study of a novel serum mRNA gene panel for diagnosis of acute septic arthritis
- Effect of clopidogrel in bone healing-experimental study in rabbits
- Anterior cruciate ligament reconstruction using a double bundle hamstring autograft configuration in patients under 30 years
- Factors associated with trigger digit following carpal tunnel release
