Factors associated with trigger digit following carpal tunnel release
Jacob Nosewicz,Carla Cavallin,Chin-I Cheng,Neli Ragina,Arno W Weiss,Anthony Zacharek
Abstract
Key words: Endoscopic carpal tunnel release; Open carpal tunnel release,Trigger digit;Carpal tunnel syndrome; Stenosing tenosynovitis
INTRODUCTION
Carpal tunnel syndrome (CTS) is a common entrapment neuropathy of the hand that affects 3.8% of the general population[1].Characteristic symptoms include burning pain,numbness,and tingling in the distribution of the median nerve distal to the wrist.CTS is diagnosed by a combination of clinical signs and median nerve conduction studies,with supportive diagnostic tools including ultrasonography,magnetic resonance imaging,and diffuse tensor imaging[2].Surgical treatment,or carpal tunnel release (CTR),involves division of the transverse carpal ligament in order to release pressure on the median nerve.Surgical decompression of the median nerve of the can be accomplishedviatwo different approaches:Open carpal tunnel release (OCTR) and endoscopic carpal tunnel release (ECTR).
Trigger digit is a common disorder of the hand associated with carpal tunnel syndrome[3].In trigger digit,the flexor tendon of the distal palm thickens,creating dysfunction between the flexor tendon and its encompassing sheath.The result is a painful locking of the affected digit in flexion or extension,most commonly due to obstruction at the A1 annular pulley[4].Markedly,systemic inflammatory conditions that increase the risk for carpal tunnel syndrome may also predispose to trigger digit[4-6].Current evidence also suggests that CTR surgery may be a risk factor for trigger digit development; however,the association between surgical approach to CTR and postoperative trigger digit is equivocal[6-8].Our study aimed to investigate patient risk factors for trigger digit development following CTR and whether these risk factors varied between OCTR and ECTR.
MATERIALS AND METHODS
IRB approval was obtained.All patients over the age of 18 from a single institution who underwent CTR from January 2013 to December 2016 were included.Two board certified surgeons from a single institution performed all procedures.One physician exclusively performed all of the OCTR procedures while the other physician exclusively performed all of the ECTR procedures.
Data collection plan and inclusion/exclusion criteria
Electronic medical record databases were queried for Current Procedural Technology codes 64721; Neuroplasty and/or transposition; median nerve at carpal tunnel(OCTR),and 29848; ECTR.This yielded 1138 carpal tunnel procedures from 800 patients for initial eligibility.
The initial list of eligible patients was merged with a query of all patients with ICD-10 Dx code “M65.3*,” trigger digit.Trigger digit was clinically diagnosed as tenderness over the A1 pulley of the digit with a history of locking in the digit.Electronic medical records of patients fulfilling both the initial CTR procedural code and trigger finger diagnosis code were evaluated for inclusion eligibility.All patients with a diagnosis of trigger finger prior to ipsilateral CTR were excluded.Paper charts were collected for these patients to confirm the accuracy of the electronic medical records.94 procedures were excluded for diagnosis of trigger finger prior to ipsilateral CTR.
Stringent exclusion criteria were employed in order to best isolate the effects of CTR.Only patients with first-time CTR for each specific hand were included.Patients undergoing recurrent CTR on the ipsilateral hand were excluded.73 recurrent CTR procedures were excluded.Further exclusion criteria included a patient history of dupuytren's contracture,tendon repair of the finger or hand,metacarpophalangeal joint arthroplasty,and trapeziectomy prior to ipsilateral CTR.These criteria yielded 16 excluded procedures.In total,171 CTR procedures from 106 patients were excluded.
Two authors accrued the variables of interestviapatient electronic medical records and paper records.967 CTR procedures from 694 patients were included in the final analysis.
Independent and dependent variables
Patients undergoing bilateral CTR were coded as two separate data units.These two procedures from the same patient were treated as independent entities for statistical analysis to account for the possibility that only one of the hands may develop trigger digit.Patient variables including age,gender,race,body mass index (BMI),hand dominance,smoking status,and the presence of diabetes mellitus,rheumatoid arthritis,and hypothyroidism at the time of CTR were also collected.Paper records were sought out to complete any input variables not available in the electronic medical records; however,some patient variables could not be found between electronic medical record and paper charts.BMI was further divided into three categories:Less than 25,between 25 and 30,and greater than 30.Smoking was defined as a patient being a “current every day smoker” within the electronic medical record at the time of CTR.The diagnosis of diabetes included both Type 1 and Type 2 diabetics.
The development of postoperative trigger digit was evaluated at three time points:within 6 mo following CTR,between 6 and 12 mo following CTR,and after 12 mo following CTR.Analysis included only the first-time point at which a patient developed trigger digit to reflect the true total of hands that ultimately developed trigger digit.
Statistical analysis
Descriptive statistics were provided including mean and standard deviation for continuous variables,and frequency and proportions for categorical variables.The two-samplet-test was adopted to examine differences in means for age between the two surgical approach groups.Chi-squares tests were used to test the association between categorical variables and surgical approach.Fisher's exact test was used to examine the difference in proportion of postoperative trigger digit at each time interval.
Firth's[9]penalized likelihood logistic regression was conducted to evaluate patient risk factors for postoperative trigger digit development.Patient risk factors included age,gender,BMI,diabetes mellitus,rheumatoid arthritis,smoking status,hypothyroidism,and surgical approach.Hand dominance was not included in the analysis due to the high number of missing variables.Patients were then stratified by surgical approach into an ECTR group and an OCTR group.Two more Firth logistic regression models were conducted to test the association between patient risk factors and postoperative trigger digit within each surgical group.Significant risk factors found within each surgical group were added as an interaction term to the primary logistic regression model.All of the analytical results were considered to be significant whenPvalues were less than or equal to 0.05.Data were analysed using SAS software,version 9.4 (SAS Institute Inc.,Cary,NC,United States).
RESULTS
Table 1 presents the descriptive statistics for our two surgical groups.In total,we included 967 procedures in our analysis.More patients underwent ECTR (83.5%) than OCTR (16.5%).A higher percentage of women (60.3%) underwent CTR surgery than men (39.7%).The average age of patients who received endoscopic surgery (59.93 years) was higher than that of patients who received open surgery (57.24 years) (P=0.03).Our results found that the proportion of white patients who received endoscopic or open surgery were similar at 86.9% and 87.9%,respectively; however,not all patients had race identified in their chart (P= 0.01).Both the OCTR and ECTR groups showed no significant difference in all other patient risk factors.
A total of 47 hands developed postoperative trigger digit following 967 CTR procedures (4.9%).The timing of postoperative trigger digit are reported in Table 2.Postoperative triggering occurred 36 times following 807 ECTR.8 hands experienced trigger digit within 6 mo (22%),10 hands between 6 and 12 mo (28%),and 18 hands after 12 mo (50%).11 hands developed postoperative trigger digit following OCTR.Four hands developed postoperative trigger digit within 6 mo (36%),3 hands between 6 and 12 mo (28%),and 4 hands after 12 mo (36%).There was no significant difference between the ECTR and OCTR groups to develop trigger digit at all three postoperative time markers.
A total of 64 digits experienced postoperative triggering following 967 CTR procedures as shown in Table 3.The long finger was most commonly affected (28%),followed equally by the first and fifth digit (22%),then the fourth digit (19%),with the second digit being the least commonly affected (9%).
There is insufficient evidence to conclude that independent predictors are related to postoperative trigger digit development as shown in Table 4.However,preliminary within group analysis revealed a significant interaction effect between gender and surgical approach.This significant interaction effect between gender and surgical approach was confirmed in the primary multivariable logistic regression model demonstrated in Table 4 (P= 0.008).Females were more likely to develop postoperative trigger digit than males after OCTR [Odds ratio (OR) = 3.992],but were less likely to develop postoperative trigger digit than males after ECTR (OR = 0.489).
DISCUSSION
Patients experience similar functional outcomes between OCTR and ECTR; however,the influence of CTR surgical approach on the development of other hand comorbidities,such as trigger digit,is not cohesive[6,8,10].Furthermore,the interaction between patient comorbidities and the postoperative condition of the carpal tunnel remains unknown.Our study investigated the interaction between CTR surgical approach and patient comorbidities as risk factors for trigger digit.
The incidence rate of new-onset trigger digit development following CTR has been reported between 4%-31.3%[8,11].Linet al[12]'s meta-analysis found a collective incidence rate of 7.7% after excluding patients with a history of trigger digit prior to their CTR.Our incidence rate is at the low end of what has been reported (4.9%).Postoperative trigger digit has been reported to primarily occur in the first 6 mo following CTR[12].In our study,postoperative trigger digit development most commonly happened after 12 mo.The extended time length for patient follow up in our study may explain why the majority of trigger digits occurred beyond one year.
There were no significant individual predictors revealed for the development of trigger digit following CTR (Table 4).Leeet al[13]evaluated biomechanical changes within the carpal tunnel following 497 OCTR procedures.The authors found significant differences in volar migration of the flexor tendons between those patients who developed postoperative trigger digit and those that did not.The authors suggested that this increased volar positioning of the flexor tendons resulted in increased friction upon entrance to the A1 pulley,thereby increasing the risk for trigger digit development.Karalezliet al[14]confirmed these findings in their study of cadavers subject to OCTR.This change was most pronounced in the third,fourth,and first digits.The frequency these digits triggered in our study support volar migration of the flexor tendons as an important factor for postoperative trigger digit development (Table 3).
Momoseet al[15]utilized MRI to study structural changes within the carpal tunnel following 36 ECTR procedures.Similar structural changes occurred within the carpal tunnel compared to prior cadaver studies evaluating OCTR.These studies suggest that volar migration of the flexor tendons within the carpal tunnel may occur following both endoscopic and OCTR.Our results also reflect that a similar postoperative condition within the carpal tunnel may exist for both surgical techniques as surgical approach was not found to be an independent risk factor for postoperative trigger digit development.
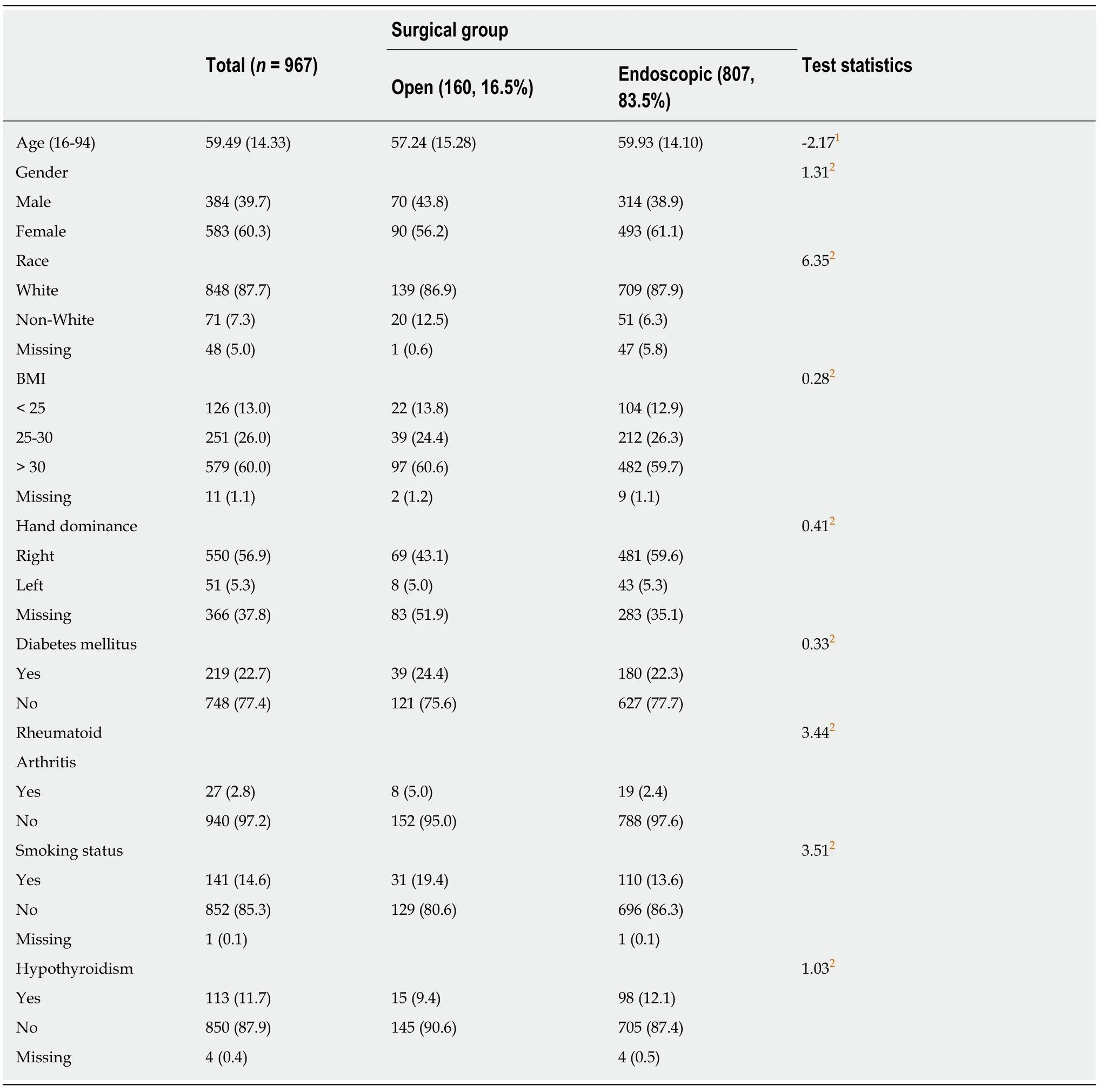
Table 1 Descriptive statistics for open and endoscopic surgical groups,n (%)
In contrast,Goshtasbyet al[6]reported ECTR as an independent predictor for trigger digit after CTR.The authors suggested that blunt force trauma from endoscope insertion and an earlier return to work offered by ECTR may be contributing factors for trigger digit development.These suggestions were not reflected in our results.Furthermore,prior retrospective studies in our practice have found no difference in return to work following open and ECTR,which is also reflected in the current discourse[10].
Non-enzymatic glycosylation of collagen seen in hyperglycemic states may lead to connective tissue thickening,thereby lowering the threshold for trigger digit occurrence[4,8].Grandizioet al[8]evaluated 1217 CTR patients,214 of which were diabetics,and found diabetes to be a significant risk factor for the development of trigger digit following CTR.They repeated their chi-square analysis for OCTR to account for the dissimilar percentages of this procedure between their patient groups.The authors found diabetes to no longer predict trigger digit following CTR.This coincides with our study results that found no association between diabetes and trigger digit development after OCTR; however,our study did not find diabetes to be an independent risk factor for both OCTR and ECTR patients.
Goshtasbyet al[6]reported thyroid disease as a categorical predictor of postoperative trigger digit.The authors theorized that the soft tissue swelling seen in thyroid disease may lead to flexor tendon dysfunction.Consequently,this may lower the threshold for trigger digit development when compounded with the postoperative inflammatory state of the carpal tunnel.Our study did not find an association between hypothyroidism and an increased risk of developing trigger digit.While we specifically looked at the effects of hypothyroidism on trigger digit development,Goshtasbyet al[6]evaluated hyper- and hypothyroidism together as one independent variable.
We are the first to report gender as a potential risk factor for trigger digit following CTR.Females were as likely as males to develop trigger digit when controlling for surgical approach as an independent variable; however,the effect of gender became significant when patients were stratified into separate surgical groups.There appears to be a positive interaction between being female and receiving OCTR and a negative interaction between being female and receiving ECTR.This suggests each surgical approach may affect the carpal tunnel differently between males and females,thereby changing the threshold for trigger digit occurrence in each gender.
Current studies evaluating structural changes in the postoperative carpal tunnel do not make comparisons between genders.In contrast,imaging studies reveal gender differences in baseline carpal arch morphology.Females have a smaller cross-sectional area of the carpal tunnel and decreased palmar bowing of the carpal arch distally compared to males[16].These baseline morphological differences may reduce the postoperative volar migration of the flexor tendons necessary for trigger digit development in females.Markedly,similar morphological changes of the carpal tunnel,including volar migration of the flexor tendons,occurs following both ECTR and OCTR[13,15,17].Therefore,it may be expected that females are more likely than males to develop postoperative trigger digit given the smaller cross-sectional area of their carpal tunnel.This was not reflected in our study,which suggests that baseline morphological differences between genders may not contribute to postoperative trigger digit development.Gender differences in the postoperative carpal tunnel need to be further explored in order to support our findings.
Our study has a few limitations.First,our sample population was largely homogenous.Our findings may not be generalizable to more diverse populations.Second,the inconsistent coding of osteoarthritis (not included in Table 1) and hand dominance in our electronic medical records did not allow us to include these variables.Osteoarthritis and hand dominance have previously been found to be independent risk factors for trigger digit following CTR[6,18].Third,the retrospective nature of this study dictates that our diagnosis of trigger digit be dependent on electronic medical records.Patients are educated on the potential for trigger digit occurrence; however,some patients may delay seeing a physician until they reach a subjective threshold of disability.This may explain the minority of our patients developing trigger digit in the first 6 mo following CTR.
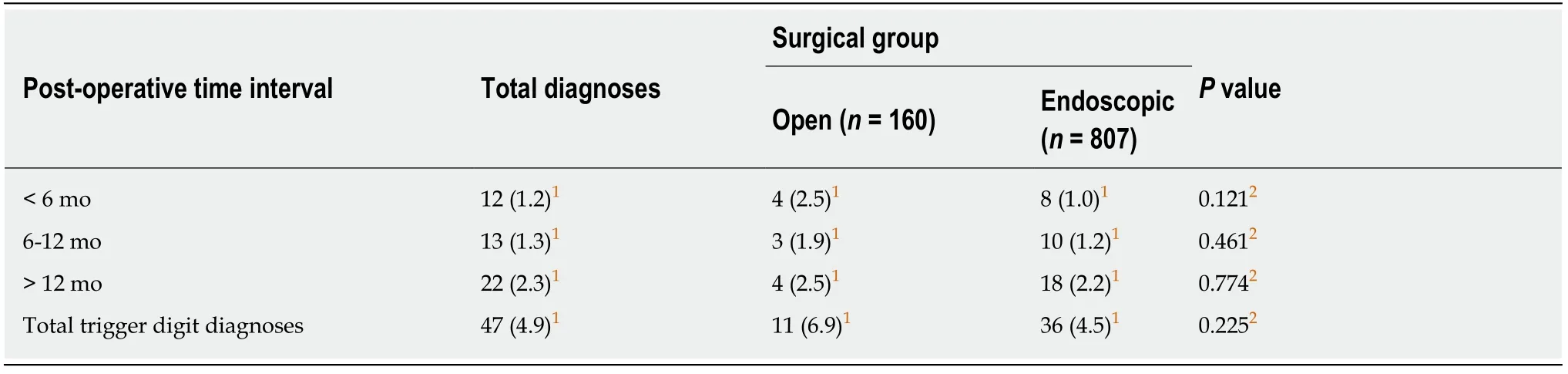
Table 2 Frequency and proportion for trigger digit diagnosis at < 6 mo,6-12 mo,and > 12 mo for each surgical group,n (%)
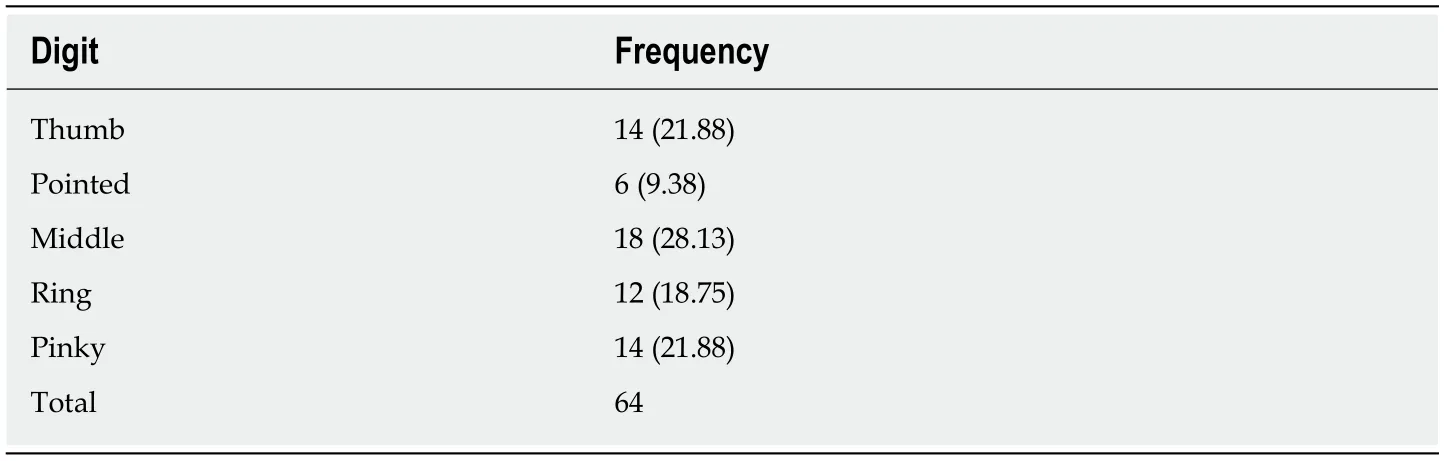
Table 3 Trigger digit frequency and proportion by digit,n (%)
Strengths of this study include a large patient population size,stringent exclusion criteria for our sample population,and a study paradigm that explored the interaction between surgical approach to CTR and patient comorbidities.One unique aspect of this paradigm was examining the interaction effect between surgical approach and gender.A prospective randomized intervention is needed to confirm the gender differences we found between the two surgical groups.
Our study reveals that patient comorbidities do not influence the development of trigger digit following CTR.
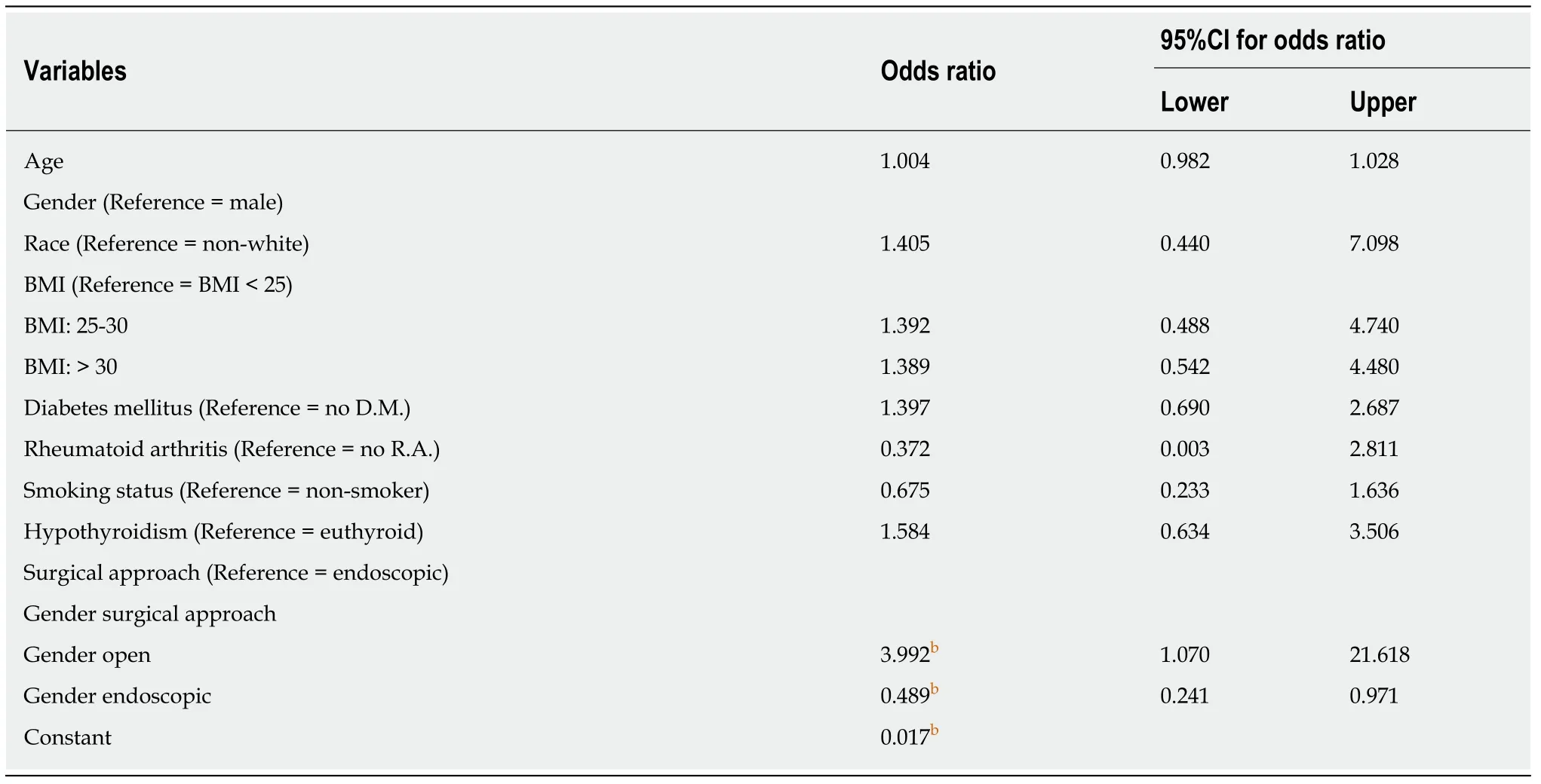
Table 4 Multivariable logistic regression analysis predicting post-operative trigger digit development
ARTICLE HIGHLIGHTS
Research background
Carpal tunnel release (CTR) surgery consists of dividing the carpal tunnel ligament in order to decompress the median nerve.CTR is accomplishedviaeither an open or endoscopic approach.Markedly,CTR surgery may predispose patients to trigger digit,a common orthopedic hand condition.
Research motivation
The association between surgical approach to CTR,either open or endoscopic,and postoperative trigger digit development remains equivocal.
Research objectives
Our study aimed to investigate patient risk factors for trigger digit development following CTR and whether these risk factors varied between open carpal tunnel release (OCTR) and endoscopic carpal tunnel release (ECTR).
Research methods
This retrospective chart analysis evaluated 967 CTR procedures from 694 patients for the development of postoperative trigger digit.Patients were stratified according to the technique utilized for their CTR,either open or endoscopic.The development of postoperative trigger digit was evaluated at three time points:within 6 mo following CTR,between 6 and 12 mo following CTR,and after 12 mo following CTR.Firth's penalized likelihood logistic regression was conducted to evaluate sociodemographic and patient comorbidities as potential independent risk factors for trigger digit.Secondary regression models were conducted within each surgical group to reveal any potential interaction effects between surgical approach and patient risk factors for the development of postoperative trigger digit.
Research results
There was no significant difference between the ECTR and OCTR groups to develop trigger digit at all three postoperative time markers.Furthermore,there were no significant individual predictors revealed for the development of trigger digit following CTR; however,within group analysis revealed a significant interaction effect between gender and surgical approach.This significant interaction effect between gender and surgical approach was confirmed in the primary multivariable logistic regression model (P= 0.008).Females were more likely to develop postoperative trigger digit than males after OCTR(OR = 3.992),but were less likely to develop postoperative trigger digit than males after ECTR (OR = 0.489).
Research conclusions
Our study found that patient comorbidities do not influence the development of trigger digit following CTR.Markedly,gender differences for postoperative trigger digit may depend on surgical approach to CTR.We are the first to report gender as a potential risk factor for trigger digit following CTR.Females were as likely as males to develop trigger digit when controlling for surgical approach as an independent variable; however,the effect of gender became significant when patients were stratified into separate surgical groups.
Research perspectives
Current studies evaluating structural changes in the postoperative carpal tunnel do not make comparisons between genders.A prospective randomized intervention study is needed to confirm the gender differences we found between ECTR and OCTR.We also suggest the use of magnetic resonance imaging to compare changes in the morphological differences of the postoperative carpal tunnel,including volar migration.
 World Journal of Orthopedics2019年12期
World Journal of Orthopedics2019年12期
- World Journal of Orthopedics的其它文章
- lmpact of dental clearance on total joint arthroplasty:A systematic review
- Pilot study of a novel serum mRNA gene panel for diagnosis of acute septic arthritis
- Effect of clopidogrel in bone healing-experimental study in rabbits
- Anterior cruciate ligament reconstruction using a double bundle hamstring autograft configuration in patients under 30 years
