心肌缺血再灌注损伤不同表现形式的临床研究
张英 王亚柱 张皓然

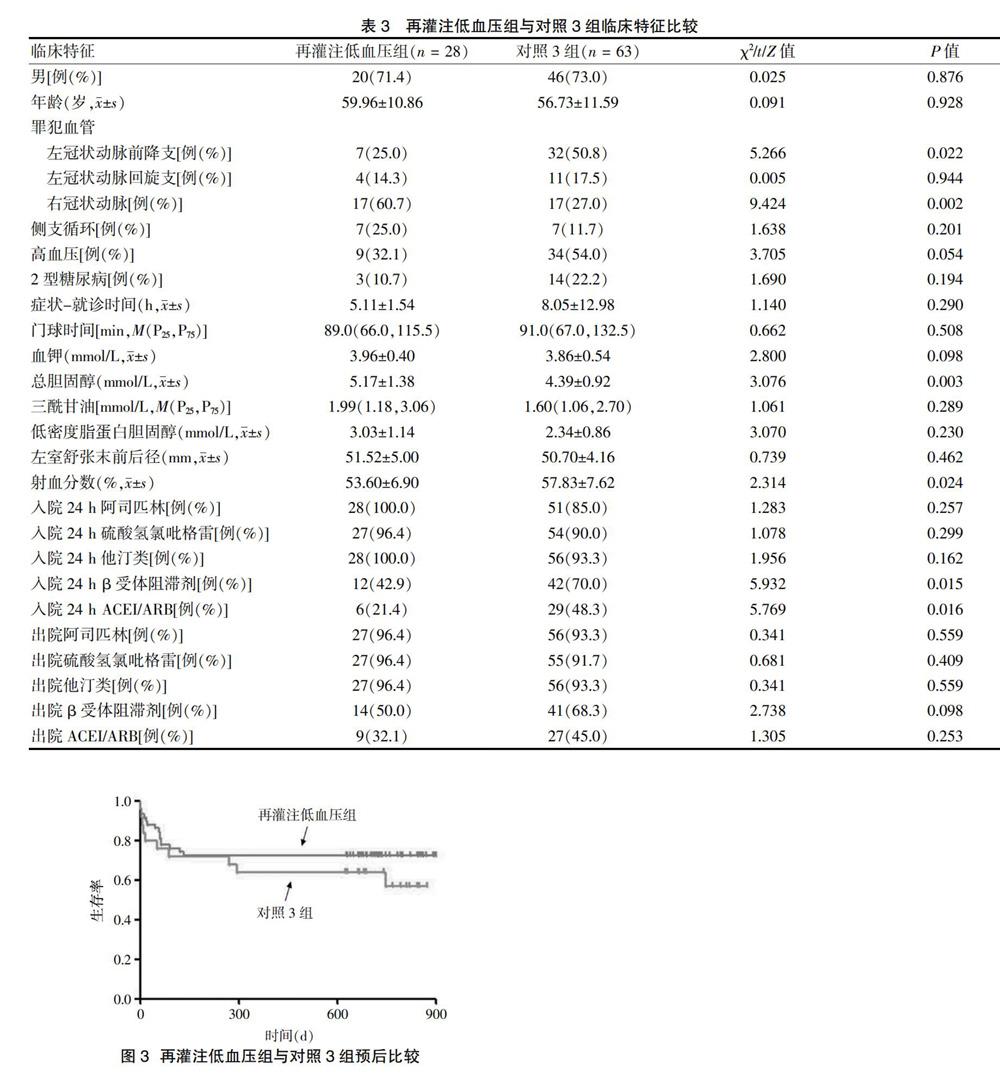

[摘要] 目的 探讨心肌缺血再灌注损伤不同表现形式的危险因素及预后。 方法 选取2015年1~11月于承德医学院附属医院行直接经皮冠状动脉介入治疗的患者91例,根据发生缺血再灌注损伤的不同临床表现形式进行分组,缓慢性心律失常组21例,对照1组70例;快速性心律失常组9例,对照2组82例;再灌注低血压组28例,对照3组63例。记录病史、诊断、手术及治疗方案,进行随访并完成汇总。 结果 缓慢性心律失常组罪犯血管为右冠状动脉、侧支循环发生率高于对照1组,罪犯血管为左冠状动脉前降支发生率低于对照1组,差异有统计学意义(P < 0.05)。快速性心律失常组症状-就诊时间早于对照2组,罪犯血管为右冠状动脉发生率高于对照2组,差异有统计学意义(P < 0.05)。再灌注低血压组罪犯血管为左冠状动脉前降支发生率、射血分数、入院24 h β受体阻滞剂及入院24 h 血管紧张素转化酶抑制剂/血管紧张素受体拮抗剂低于对照3组,罪犯血管为右冠状动脉发生率及总胆固醇水平高于对照3组,差异有统计学意义(P < 0.05)。根据术后随访结果绘制生存曲线,经Log Rank检验得出不同临床表现形式分组患者Kaplan-Meier生存曲线,差异均无统计学意义(P > 0.05)。 结论 罪犯血管为右冠状动脉是发生缺血再灌注损伤的危险因素。存在侧支循环对预测发生缓慢性心律失常、症状-就诊时间短对预测发生快速性心律失常、总胆固醇水平高对预测发生低血压具有重要意义。
[关键词] 冠状动脉介入治疗;缺血再灌注损伤;缓慢性心律失常;快速性心律失常;再灌注低血压
[中图分类号] R541 [文献标识码] A [文章編号] 1673-7210(2019)08(b)-0064-05
[Abstract] Objective To explore the risk factors and prognosis of different manifestations of myocardial ischemia-reperfusion injury. Methods Ninety-one patients who underwent direct percutaneous coronary intervention in Affiliated Hospital of Chengde Medical College from January to November 2015 were divided into groups according to different clinical manifestations of ischemia-reperfusion injury. Twenty-one cases in bradyarrhythmia group and 70 cases in control group 1; 9 cases in tachyarrhythmia group and 82 cases in control group 2; 28 cases in reperfusion hypotension group and 63 cases in control group 3. Medical history, diagnosis, operation and treatment plan, follow-up and summary were recorded. Results The incidence of right coronary artery and collateral circulation of criminals in bradyarrhythmia group was higher than that in control group 1, the incidence of left anterior descending coronary artery of criminals in bradyarrhythmia group was lower than that in control group 1, the differences were statistical significance (P < 0.05). The symptoms-visiting time of tachyarrhythmia group was earlier than that of control group 2, and the incidence of right coronary artery was higher in criminals than that of control group 2, the differences were statistical significance(P < 0.05). The incidence of anterior descending branch of left coronary artery, ejection fraction, 24 h β receptor blocker and 24 h ACEI/ARB of criminals in reperfusion hypotension group were lower than those in control group 3, while the incidence of right coronary artery and total cholesterol level of criminals in reperfusion hypotension group were higher than those in control group 3, the differences were statistical significance (P < 0.05). The survival curves were drawn according to the follow-up results. The Kaplan-Meier survival curves of patients with different clinical manifestations were obtained by Log Rank test, there was no significant difference (P > 0.05). Conclusion The criminals′ right coronary artery is a risk factor for ischemia-reperfusion injury. The presence of collateral circulation is of great significance in predicting bradyarrhythmia, short symptom-visit time, rapid arrhythmia and high total cholesterol level.
[Key words] Percutaneous coronary intervention; Ischemia reperfusion injure; Bradyarrhythmia; Tachyarrhythmia; Reperfusion hypotension
急性ST段抬高型心肌梗死(STEMI)是危及患者生命的临床危重症之一,目前认为急诊介入是最有效的治疗手段,但可能因缺血再灌注损伤(IRI)而加重病情甚至危及生命。IRI在临床上表现形式复杂、多样,本文旨在探讨发生IRI时不同表现形式的危险因素与预后。
1 资料与方法
1.1 一般资料
选取2015年1~11月于承德医学院附属医院心脏内科因STEMI于发病12 h内接受直接经皮冠状动脉介入治疗且血管完全闭塞的患者91例,依据发生IRI时不同的临床表现形式进行分组:缓慢性心律失常组21例,对照1组70例;快速性心律失常组9例,对照2组82例;再灌注低血压组28例,对照3组63例。
1.2 排除标准
①发病12 h内未能接受PPCI;②非完全闭塞病变;③PPCI术中或术后24 h内死亡者。
1.3 IRI的判断
IRI的诊断标准[1]:血管开通后发生的严重心动过缓、低血压、频发室性期前收缩;药物治疗和/或电复律、电除颤治疗后,仍有严重室性心律失常。
1.4 临床资料采集
采集患者病史、诊断、治疗方案,统一录入并汇总。
1.5 随访
出院前超声心动图评价。术后1、3、6、12、24、36个月电话及门诊随访,记录冠心病二级预防药物使用情况、是否发生MACE事件。MACE定义:因冠心病再次住院、再发急性心肌梗死、再次血运重建、致命性心律失常、心力衰竭、脑卒中、重要脏器出血及心源性死亡。
1.6 统计学方法
采用SPSS 21.0处理数据,计量资料符合正态分布用均数±标准差(x±s)表示,组间比较采用t检验,计量资料符合偏态分布用中位数(M)和四分位数(P25,P75)表示,组间比较采用Mann-Whitney U检验;计数资料用百分率(%)表示,采用χ2检验;两组COX回归应用Kaplan-Meier法绘制生存曲线,Log Rank检验为双侧检验,以P < 0.05为差异有统计学意义。
2 结果
2.1 缓慢性心律失常组与对照1组临床特征比较
缓慢性心律失常组罪犯血管为右冠状动脉、侧支循环发生率高于对照1组,罪犯血管为左冠状动脉前降支发生率低于对照1组,差异有统计学意义(P < 0.05)。见表1。根据术后随访结果绘制生存曲线,经Log Rank检验得出两组患者Kaplan-Meier生存曲线,差异无统计学意义(χ2 = 2.548,P = 0.110)。见图1。
2.2 快速性心律失常组与对照2组临床特征比较
快速性心律失常组症状-就诊时间早于对照2组,罪犯血管为右冠状动脉发生率高于对照2组,差异有统计学意义(P < 0.05)。见表2。根据术后随访结果绘制生存曲线,经Log Rank检验得出两组患者Kaplan-Meier生存曲线,差异无统计学意义(χ2 = 0.017,P = 0.896)。见图2。
2.3 再灌注低血压组与对照3组临床特征比较
再灌注低血压组罪犯血管为左冠状动脉前降支发生率、射血分数、入院24 h β受体阻滞剂及入院24 h ACEI/ARB低于对照3组,罪犯血管为右冠状动脉发生率及总胆固醇水平高于对照3组,差异有统计学意义(P < 0.05)。见表3。术后随访结果绘制生存曲线,经Log Rank检验得出两组患者Kaplan-Meier生存曲线,差异无统计学意义(χ2 = 1.103,P = 0.294)。见图3。
3 讨论
长期以来,因IRI的严重性使再灌注治疗被称为双刃剑,IRI在临床上可表现为缓慢性心律失常、快速性心律失常、低血压。目前研究认为,IRI与氧自由基的释放与堆积[2]、细胞内钙超载[3]、线粒体通透性转换孔开放[4]、坏死心肌局部离子与电位差、炎性反应[5-6]、儿茶酚胺释放过多与一氧化氮释放减少[7]有关。根据IRI表现形式不同考虑其发生机制与患者本身病情的特异性有关,因此本研究按照IRI的不同表现形式进行分组,研究其危险因素与预后改变。
对于缓慢性心律失常、快速性心律失常、低血压,罪犯血管为右冠状动脉更常见,考虑与其为窦房结动脉、房室结动脉的主支血管,右冠状动脉闭塞后常伴有迷走神经兴奋性增强,可表现为低血压及缓慢性心律失常,同时缓慢性心律失常造成Q-T间期延长亦增加快速性心律失常风险[8-9]。对于缓慢性心律失常,合并侧支循环比例高于对照组,侧支循环意味着更为严重、弥漫的长期、缓慢性病变。
合并快速性心律失常者发病-就诊时间明显早于对照组,目前认为6 h为IRI的时间临界点[10]。本研究证明,发病-就诊时间快速性心律失常组早于对照2组,缺血时间过长心肌完全坏死、丧失电活动,反而不易发生IRI[11]。故早期行急診介入治疗反而容易发生IRI,尤其是快速性心律失常。合并低血压患者较对照组总胆固醇水平明显增高,血脂增高可造成血管内膜细胞损伤,引起冠状动脉狭窄、阻塞;可造成血管壁弹性下降,促进动脉硬化与血栓形成[12-13]。目前认为,低密度脂蛋白胆固醇、三酰甘油、总胆固醇均为动脉硬化的危险因素[14],本研究证实,合并低血压患者较对照3组总胆固醇水平明显增高。
总之,无论何种类型的IRI,患者出院后药物治疗方案及3年长期随访的预后均无明显差异,提示IRI仅对发作时及围术期造成影响[15-17],无论是否出现IRI,患者仍长期获益,获益于积极的血运重建与规范的药物治疗[18-20]。
[参考文献]
[1] Thygesen K,Alpert JS,Jaffe AS,et al. Third universal definition of myocardial infarction [J]. Eur Heart J,2012,33(20):2551-2567. doi:10.1093/eurheartj/ehs184.
[2] Ghaderi S,Alidadiani N,Dilaver N,et al. Role of glycogen synthase kinase following myocardial infarction and ischemia-reperfusion [J]. Apoptosis,2017,22(7):887-897.doi:10.1007/s10495-017-1376-0.
[3] Sventzouri S,Nanas I,Vakrou S,et al. Pharmacologic inhibition of the mitochondrial Na+/Ca2+ exchanger protects against ventricular arrhythmias in a porcine model of ischemia-reperfusion [J]. Hellenic J Cardiol,2018,59(4):217-222.doi:10.1016/j.hjc.2017.12.009.
[4] Hausenloy DJ,Yellon DM. Ischaemic conditioning and reperfusion injury [J]. Nat Rev Cardiol,2016,13(4):193-209.doi:10.1038/nrcardio.2016.5.
[5] Mohamadi Y,Mousavi M,Mahboubeh H,et al. The role of inflammasome complex in ischemia-reperfusion injury [J]. J Cell Biochem,2018.doi:10.1002/jcb.27368.
[6] He Z,Ma C,Yu T,et al. Activation mechanisms and multifaceted effects of mast cells in ischemia reperfusion injury [J]. Exp Cell Res,2019,376(2):227-235.doi:10.1016/j.yexcr.2019.01.022.
[7] Intachai K,Chattipakorn S,Chattipakorn N,et al. Revisiting the cardioprotective effects of acetylcholine receptor activation against myocardial ischemia/reperfusion injury [J]. Int J Mol Sci,2019(9):E2466.doi:10.3390/ijms19092466.
[8] Gatzke N,Güc N,Hillmeister P,et al. Cardiovascular drugs attenuated myocardial resistance against ischaemia-induced and reperfusion-induced injury in a rat model of repetitive occlusion [J]. Open Heart,2018,5(2):e000889.
[9] Ferdinandy P,Hausenloy DJ,Heusch C,et al. Interaction of risk factors,comorbidities,and comedications with ischemia/reperfusion injury and cardioprotection by preconditioning,postconditioning,and remote conditioning [J]. Pharmacol Rey,2014,66(4):1142-1174.
[10] Yip HK,Chen MC,Chang HW,et al. Angiographic morphologic features of infarct-related arteries and timely reperfusion in acute myocardial infarction- predictors of slow-flow and no-reflow phenomenon [J]. Chest,2002, 122(4):1322-1332.doi:10.1378/chest.122.4.1322.
[11] 趙艳辉,朱智明,高连如,等.ST段抬高型心肌梗死再灌注心律失常患者主要心血管事件的观察研究[J].中国急救复苏与灾害医学杂志,2106,10(6):577-581.
[12] Musman J,Paradis S,Panel M,et al. A TSPO ligand prevents mitochondrial sterol accumulation and dysfunction during myocardial inshemia-reperfusion in hypercholesterolemic rats [J]. Biochem Pharmacol,2017,142(15):87-95.doi:10.1016/j.bcp.2017.06.125.
[13] D′Annunzio V,Donato M,Buchholz B,et al. High cholesterol diet effects on ischemia-reperfusion injury of the heart [J]. Can J Physiol Pharmacol,2012,90(9):1185-1196.doi:10.1139/y2012-085.
[14] Gomaraschi M,Calabresi L,Franceschini G. Protective effects of HDL against ischemia/reperfusion injury [J]. Front Pharmacol,2016,25(7):2.doi:10.3389/fphar.2016. 00002.eCollection 2016.
[15] Kazmi DH,Kapoor A,Sinha A,et al. Role of metabolic manipulator trimetazidine in limiting percutaneous coronary intervention-induced myocardial injury [J]. Indian Heart J,2018,12(70):S365-S371. doi:10.1016/j.ihj.2018. 10.415.
[16] Xiao Y,He S,Zhang Z,et al. Effect of high-dose statin pretreatment for myocardial perfusion in patients receiving percutaneous coronary intervention (PCI):a meta-analysis of 15 randomized studies [J]. Med Sci Monit,2018,12(24):9166-9176.doi:10.12659/MSM.911921.
[17] Li J,Xu X,Zhou X,et al. Cardiovascular events associated with nicorandil administration prior to primary percutaneous coronary intervention in patients with acute ST-segment elevated myocardial infarction:a systematic review and meta-analysis [J]. Expert Opin Drug Saf,2019, 18(6):537-547.doi:10.1080/14740338.2019.1617848.
[18] Shah VK,Shalia KK. Reperfusing the myocardium-a damocles Sword [J]. Indian Heart J,2018,70(3):433-438.
[19] Lavi S,Abu-Romeh N,Wall S,et al. Long-term outcome following remote ischemic postconditioning during percutaneous coronary interventions-the RIP-PCI trial long-term follow-up [J]. Clin Cardiol,2017,40(5):268-274.doi:10.1002/clc.22668.
[20] Stiermaier T,Jensen JO,Rommel KP,et al. Combined intrahospital remote ischemic perconditioning and postconditioning improves clinical outcome in st-elevation myocardial infarction [J]. Circ Res,2019,124(10):1482-1491.doi:10.1161/CIRCRESAHA.118.314500.
(收稿日期:2019-05-02 本文編辑:李亚聪)

