Research Progress on Diagnosis and Treatment of Chronic Osteomyelitis
Ziquan Wu, Delu Zeng, Jiangling Yao, Yangyang Bian, Yuntao Gu,Zhulong Meng, Jian Fu, Lei Peng*
1Trauma Center, The First Affiliated Hospital of Hainan Medical University,Haikou 570100, China
2Key Laboratory of Emergency and Trauma of Ministry of Education,Hainan Medical University, Haikou 571199, China
Key words: bone infection; chronic osteomyelitis; diagnosis; treatment
Abstract We review the representatives literatures on chronic osteomyelitis, sum up the new insights in recent years into diagnostic options and treatment regimens, analyze the advantages and disadvantages of various diagnostic approaches and treatment strategies, and propose areas of interest to make current diagnostic and treatment strategies more specific.
CHRONIC osteomyelitis is the most intractable infection developing from traumatic fracture and joint replacement, implicating bone or marrow, cortex, periosteum, and surrounding soft tissue. Early correct diagnosis of osteomyelitis is difficult and needs to be differentiated from bone tumor or bone tuberculosis. Due to the destruction of local blood supply system, the foreign body reaction and local inflammatory reaction, antibiotic is hard to arrive to the lesion area. The other reason is formation of a bacterial biofilm, which greatly reduces the efficacy of systemic antibiotics, increases the recurrence of bone infection, thus making treatment difficult.[1]In this article, we mainly provide an overview of the diagnosis and treatment for chronic osteomyelitis.
Diagnosis of Chronic Osteomyelitis
Chronic osteomyelitis is mainly caused by improper or untimely treatment of acute osteomyelitis, a penetrating bone injury, compound fracture, or application of a metal implant (such as internal fixation apparatus or artificial joint prosthesis).[2,3]Clinically, the affected site presents with localized bone pain, erythema and purulent secretion of the surrounding area as well as instability and deformity accompanied by impaired vascular circulation.[4,5]Serious consequences would ensue if the inflammation cannot be effectively controlled, such as inflammatory diffusion, sinus tracts,local osteopenia,[6]and osteonecrosis. Therefore, it is particularly important to diagnose and manage osteomyelitis early. Diagnosis and differential diagnosis are made mainly according to trauma history, clinical manifestations, hematological indicators, imaging studies,and bacteriological examination and bone biopsy.
Inflammatory markers
The commonly used indicators, including routine blood test, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and procalcitonin (PCT) as well as other indicators, reflect different degrees of inflammation.
ESRandCRPare inflammatory markers that have shown diagnostic use at other anatomic sites, including vertebral osteomyelitis, long bone osteomyelitis,periprosthetic joint infections, and diabetic foot osteomyelitis.[7-9]CRP is a relatively reliable indicator as a product of inflammation that increases during the first few hours after infection and returns to normal within 1 week after the disease is well controlled. Mouzopouloset al.[10]reported that CRP can be used for monitoring infection with higher sensitivity. Increased serum inflammatory markers such as CRP and ESR are often used to the diagnosis of bone infection with a sensitivity and specificity of > 0.70.[11,12]
PCTis a 116 amino acid protein with a molecular mass of 13 kDa, mainly produced by neuroendocrine cells such as the C cells of the thyroid, lung, and pancreatic tissue. It has been showed that monocytes stimulated by endotoxin and human hepatic tissue stimulated by tumor necrosis factor or interleukin 6 produced large amount of PCT.[13]Butbul-avielet al.[14]thought that, in most cases, PCT can be used to distinguish between skeletal infection, local infection, or inflammation, where as an acute phase reactant such as CRP cannot. Another study performed by Mutluoğluet al.[15]described no significant difference of PCT levels in serum between patients with and without osteomyelitis and concluded that PCT cannot distinguish osteomyelitis in diabetic foot infections. Moreover, Michailet al.[16]examined inflammatory markers of patients with diabetic foot developing chronic osteomyelitis,after 7 days of treatment with antibiotics, CRP, white blood cell count and PCT recovered the normal levels,only ESR maintained at a high level until 3 months of follow-up, suggesting that ESR can be used as a followup indicator in patients with osteomyelitis. We believe that the differences in the above conclusions may be caused by the small sample size. For these indicators,however, they cannot be used for the diagnosis of bone infection alone because they may agree with those obtained by patients with soft-tissue infections.So we can simultaneously detect and combine with the medical history and other factors to analyze results comprehensively.
Imaging studies
X-rayhave characteristic appearances of widely available, inexpensive,[17]fast, small damage and easy operation. X-ray, with the sensitivity ranging from 43%to 75% and specificity of 75%-83%, is considered to reflect the degree of osteomyelitis, especially after the 2-week onset of the disease.[18]The main features of X-rays for chronic osteomyelitis may include nonspecific periosteal reaction, osteolysis, a dense intramedullary cortical sequestrum, endosteal scalloping, an involucrum,[19]and decalcification of pathological bone.Post arthroprosthesis osteomyelitis may show periprosthetic lucency and fracture nonunion.[20]The major limitation of X-rays is low sensitivity for early osteomyelitis as well as cannot distinguish it from fracture or Charcot arthropathy.
CTis also an important modality to be performed to diagnose osteomyelitis. CT images of osteomyelitis mainly show swelling of local bone tissue, muscle, the muscle interspace or subcutaneous tissue, the capsular space and inflammatory parcels, gas in soft tissue,fat-fluid level, and the sinus.[21]CT sensitively detects destruction of cortical bone, periosteal proliferation,soft tissue expansion, dead bone, and small foreign matter related to an infection.[22]In addition, CT can guide biopsy, but it is susceptible to the interference by metal fixation devices.
Positron emission tomography-CT(PET-CT), which is a practice of image fusion of PET and CT having been exhibiting more accurate diagnoses than the two scans performed separately, has been shown to provide the accurate location of abnormal metabolic or functional activity within the body. It has been reported when used to diagnose internal fixation-related osteomyelitis, PET-CT has high accuracy with diagnostic sensitivity being over 95% and specificity between 75% and 99%, if there are no metal fixtures. Disadvantages of this modality include radiation exposure as well as considerable costs and limited availability.[23,24]
Magnetic resonance imaging(MRI) is obviously superior to X-ray and CT in pinpointing the extent and pathologic conditions of the infectious bone and soft tissues involved due to its multi-orientation, multi-parameter,high soft tissue contrast, and no bone artifacts, etc.Moreover, MRI is a useful method to detect early osseous erosion,[25]so it is more suitable for an early diagnosis.Due to the absence of ionizing radiation and the accuracy for the demonstration of multifocality, symmetry, osseous inflammation, and bone marrow replacing processes.Whole Body MRI (WB-MRI) has become more popular at many institutions worldwide.[26,27]Furthermore, the uperior soft tissue resolution of MRI affords the accurate characterizations of fascia, muscles, tendons, ligaments,vessels, and nerves, which can yield important information toward the differential diagnosis.[28]For the pediatric population with chronic recurrent multifocal osteomyelitis, MRI might provide the optimal radiology outcomes that are possible, and further insight into the potential of pediatric bone to recover and remodel when affected by inflammatory conditions.[29]However, MRI has poor specificity for calcification, high costs and more contraindications such as pacemakers, prosthetic valve implantation,and other ferromagnetic implants.
Other imaging methodsUltrasonography can be used to diagnose soft tissue lesions of osteomyelitis early, as it clearly shows swollen soft tissue, cystic and solid parcels,subperiosteal abscesses, a thickened periosteum, and fluid accumulation around abnormal bone. Ultrasonography can determine the site and extent of infection, and the inducing factors such as foreign bodies and deep blind fistula, providing reference for diagnosis or assisting in tissue biopsy.[30]Compared to conventional X-rays,ultrasound can detect osteomyelitis days in advance(mainly for children). However, Single photon emission computed tomography (SPECT-CT) has shown to noticeably increase the accuracy of the three-phase bone scan,allowing better distinction between osteomyelitis and soft tissue infection as well as improved localization of osteomyelitis.[31]Nuclear medicine imaging, with sensitivities of more than 95% and specificities ranging from 75% to 99%, has been reported in acute and subacute bone and soft-tissue infection. It is sensitive, has a high negative predictive value, and can differentiate degenerative from infectious vertebral body end-plate abnormalities.[32]It is highly sensitive, but has the inconvenience of low specificity. Nuclear medicine scans may be a useful adjunctive study[33], when X-rays are altered by pathologic or postsurgical changes. Furthermore, white blood cell scans are considered the “gold standard” for diagnosing traumatic or postoperative chronic osteomyelitis.[34]
Bacterial culture
Due to the nonstandard use of antibiotics, Gram-negative bacteria infections have increased significantly in recent years. Variations in drug resistance of bacteria and the infection type of chronic suppurative osteomyelitis have undergone significant changes. The reason is that the endogenous normal flora or the opportunistic pathogens in the surrounding environment have become the major pathogens of pyogenic osteomyelitis.Staphylococcus aureus (SA) occupies the primary position of a mixed bacterium causing chronic osteomyelitis.[35]A bacteriologic diagnosis of chronic osteomyelitis based on isolation SA from sinus tracts must be verified by an appropriate operative culture.[36]Three to five tissue specimens should be removed from the most suspicious sites for culture before surgical disinfection and antibiotics, and the appearance of SA in the sinus bacteria culture is of certain significance for the diagnosis of chronic osteomyelitis. The identification of the causative microorganisms is essential for diagnosis and treatment. But the evidence from swabs of ulcers or sinus, however, is often misleading.
Bone histopathology or bone biopsy
Definitive diagnosis of infections was determined based on a combination of clinical and histopathological findings.[37]The characteristic histopathological findings of chronic osteomyelitis are the persistence of microorganisms, low-grade inflammation, the presence of devitalized bone, reactive new bone formation, fistulous tracts, and soft tissue involvement.[38]Sometimes only the histopathological examination of a bone-biopsy specimen with special staining procedures will permit the accurate diagnosis of infection. Surgical sampling or a needle biopsy of infected tissue provides this indispensable information.[39,40]The biopsy or purulent specimen processed with standard microbiology culture methods for isolation and identification of the causative organisms is considered as the “gold standard”for the diagnosis of osteomyelitis.[41]
Treatment of Chronic Osteomyelitis
Antibiotic treatment
The early administration of large-dose sensitive antibiotics is the basis of all treatment.[42]Changes in bacterial resistance and the bacterial spectrum are a severe challenge to clinicians. Therefore, early empirical medication and bacteria cultures are particularly important, not only to select sensitive antibiotics but also to choose the appropriate route of administration, so that drugs can reach the infected area quickly.[43]
Closed irrigation perfusion is the traditional method for treating osteomyelitis. After debriding the infected area and administering a single or combination of antibiotics, an iodophor solution, hydrogen peroxide solution, and other methods should be applied with continuous irrigation of physiological saline. Antibiotics and disinfectants can play the role of a sustained antibacterial by washing away local bacteria and other effects to reduce the spread and recurrence of infection.[44]The relatively low cost of these method, that has certain curative effect, reduces the side effects of systemic medication.
Studies have shown that the majority of antibiotics in early antibiotic bone cement carrier systems were permanently trapped in cement and could not be released. At present, the application of antibiotic carriers and sustained-release systems has been greatly improved and has played a role in the treatment of chronic osteomyelitis. Poly lactic-co-glycolic acid (PLGA)microsphere antibiotic carrier provides antibiotics at or above the minimum bactericidal concentration to the bone tissue for at least 4 weeks. This microsphere carrier does not interfere with new bone formation and is non-inflammatory and self-degradable, resulting in a significant effect, in combination with topical antibiotics to treat chronic osteomyelitis in animal models.[45]In addition, nafcillin PLGA nanoparticles[46]and pressurized cancellous bone grafts of bone marrow granulocyte precursors can be used to protect the infected non-healing sites and prevent recurrence of infection and resorption of transplanted bone.[47]Moreover, liposome carrier systems are also an option. Ciprofloxacin and vancomycin liposome combined carrier is a very good complement to other methods for treating SA-induced chronic osteomyelitis.[48]
Carrying antibiotic carrier graft technology for bone defects caused by chronic osteomyelitis is also developing rapidly. A biodegradable antibiotic implant can provide bone filling material, eliminate dead cavities, promote bone repair, and need not osteotomy.This implant promotes progressive bone repair with no residual or new bone osteolysis. No abnormal change in the periosteum occurs during treatment and patients have no obvious exudation or adverse reactions.The implant does not need to be removed and avoids secondary surgery and bone grafting of an autologous iliac.[49]Biodegradable bioactive sodium borate sustained-release vancomycin graft has been used to treat osteomyelitis and bone defects without any foreign body reaction, and has shown good biocompatibility and compressive strength. It fully integrates with the newly formed bone. Implants are ultimately absorbed.[50]Antibiotic bone cement combined with autologous bone transplantation and ilizarov external fixator for repair of post-osteomyelitis posterior tibial bone defects can control infection, promote fracture healing, and restore joint functions.[51]Pförringeret al.[52]have confirmed that formulations of calcium sulfate in combination with gentamicin (CaSO4-G) or vancomycin (CaSO4-V) and tripalmitin were testedin vitroandin vivoby implantation in rabbit tibiae. Those materials combined with potent antibiotics may be utilized to support bone healing as well as prophylactically protecting implants from infections. It is desirable to have a high local concentration of antibiotics to prevent methicillin-resistant staphylococcus aureus (MRSA) infections without reaching toxic blood levels. Peiet al.[53]developed a particle formulation based on a blend of polymers which can release vancomycin in the acidity of lysozymes, and effectively kill intracellular pathogens. Karr[54]studied 143 lower-extremity osteomyelitis locations in 125 patients treated with a calcium sulfate/hydroxyapatite liquid bone void filler with antibiotic. There was no recurrence of osteomyelitis in 96.15% of the treatable patients over 7 years. In addition, Bioactive Glass (BAG)S53P4 is one of the latest materials to be studied, with its properties presenting solutions to some of the weaknesses of the treatment currently advocated with polymethyl methacrylate (PMMA) or cement, and it presented antibacterial properties as much as antibiotic-loaded PMMA for multidrug resistant bacteria producing osteomyelitis.[55]Although all of these studies show the effectiveness of treatment, well-designed comparative studies should be performed to elucidate the most appropriate treatment options. Therefore, the choice of antibiotic and administration route should be based on the safety of the various drugs used over the long term, as well as the cost and utility of the chosen therapeutic regimen.[56]
Surgical treatment
Surgical treatment of chronic osteomyelitis is an important part of the treatment process, including thorough debridement and filling of cavities, as well as how to obtain better function and treatment after epluchage and loss of bone stability.[57]An acute attack of chronic osteomyelitis should be treated as acute osteomyelitis,and drainage should be performed when necessary.Timely surgical treatment is necessary if sinus, cavity,and sequestrum or foreign body discharge is detected with a local or systemic inflammatory response. Thorough debridement is crucial, including inflammatory tissue, sequestrum, sinus, scar tissue, infected granulation tissue, medullary cavity abscesses, and sclerotic bone,[58]until the bone section and soft tissue bleed significantly. Studies have shown that bacteria in the cortical bone of patients with chronic osteomyelitis can survive for several years, so Haidaret al.[59]advocated expanding debridement as much as possible to clear the infected and suspicious infected or necrotic tissues. If necessary, bone transport technology should be used to promote bone defect healing and to prevent recurrence. Masquelet technology (membrane-induced technique) combined with antibiotic coated intramedullary nailing can effectively control infection and create a good biological and mechanical environment for bone defect repair. It has good clinical efficacy.[60]The Masquelet technique can be used for long bone defects. In the first stage, the membrane structure is induced in the bone defect after the wounds are completely debrided and closed. In the second stage,autologous cancellous bone is implanted.[61]However,reports on membrane-induced techniques for treating chronic osteomyelitis are relatively few.[62]
Autogenous musculocutaneous flaps, fascial flaps,and a vacuum sealing drainage (VSD) device provide a solution for tissue defects. VSD device can be trimmed to the shape and size of the wound defect, and let antibiotics flow through the foci uninterrupted, attract secretions and irrigation fluid. The most important function VSD is that it temporarily fills the defects in bone and soft tissue, closes the wound to prevent the spread of local inflammation, promotes the growth of granulation tissue, and fully prepares the site for post-treatment.[63,64]Myocutaneous flap is considered the best option for tissue defects, as a good blood supply to the muscle filling the defect area increases local blood circulation, enhances bacteriostasis, and promotes wound healing. Salgadoet al.[65]reported that muscle flaps have obvious advantages in reducing bacteria. However, most muscular flaps cover damage at the donor site, which affects function and appearance.Peroneal perforator artery flaps provide an improved approach to chronic osteomyelitis of the lower extremities with fewer postoperative complications and less impaired daily function, and do not sacrifice any major vessels or nerves. Because microvascular anastomosis is not required, surgery takes less time, with a lower risk of vascular thrombosis, and the treatment effect is satisfactory. Therefore, peroneal perforator artery flap is a reliable choice to treat chronic osteomyelitis tissue defects in the lower extremities.[66]Gonzalezet al.[67]debrided 33 cases of soft tissue defects in patients with lower limb osteomyelitis and treated the area using local or regional muscle flaps. About 81% of patients had stable soft tissue coverage and no evidence of recurrent infection at the mid-term follow-up.
Other treatments
Ozone therapyResearch reported Ozonated water at a concentration of 2 mg/L can effectively kill SA and pseudomonas aeruginosa, and inhibit the inflammatory reaction. It was thought that preventive and curative effects of medical ozone in rats exposed to experimental osteomyelitis had been found by Gonenciet al.[68]through animal experiments. Bilgeet al.[69]demonstrated that ozone treatment may reduce the deleterious biochemical and histopathological effects of osteomyelitis by enhancing antioxidant mechanisms and decreasing oxidative stress. Although above findings may provide novel insights about preventive and therapeutic alternatives to treat osteomyelitis, the need for surgical debridement and antibiotic treatment should not be ignored.
Hyperbaric oxygen (HBO)therapyis a procedure that allows patients to inhale pure oxygen or high concentrations of oxygen in a hyperbaric oxygen chamber while maintaining pressure > 1 atm. The high-pressure oxygen penetrates the blood and diffuses into diseased tissue. A clinical study[70]showed that HBO therapy has an obvious curative effect in patients with antibiotic-resistant osteomyelitis. Some papers[71,72]reported that HBO improves the local state of ischemia and hypoxia by increasing the partial pressure of oxygen in anoxic tissue and triggers the oxidative stress mechanism of hydrogen peroxide, which have bactericidal effect with neutrophils.
Interventional therapyLiuet al.[73]reported the use of an indwelling interventional catheter to treat chronic osteomyelitis of the lower extremities. Using Seldinger’s femoral artery puncture,[74]the catheter is placed on the lesion side for femoral artery angiography to find the local feeding artery for the focus. Antibiotics are injected into the local blood supply artery to achieve a good curative effect.[75]
Calcium hydroxide bone cementIt has been shown that the calcium hydroxide bone cement carrier system is effective for treating chronic osteomyelitis. Since Herman B.W. reported in 1920, Ca(OH)2has been widely used to treat dental pulpitis. Through related research and literature analysis, our conclusion is: calcium hydroxide bone cement can be rapidly sterilized with good biocompatibility, slow dissolution, sustainable sterilization, and it can rapidly inactivate bacterial endotoxins with low body allergic. A study showed that direct contact with Ca(OH)2paste killed all microorganisms in a mixed infection within 72 h.[76]The antibacterial mechanism is directly linked to the release of OH-.[77]OH-caused lipid peroxidation can increase bacterial cell membrane permeability, protein denaturation and DNA damage,[78]which causes bacteria death (Figure 1).Ca(OH)2can also dissolve necrotic tissue in the medullary cavity, clean the medullary cavity, induce formation of hard tissue,[79]inhibit osteoclast activity, and activate alkaline phosphatase activity. The blood and tissue fluid mixes to form calcium salt deposit that can block small sinus, wrap and close infected area, and prevent the spread of infection. The hydration reaction of calcium phosphate cement (CPC) is carried out at 37°C and humidity of 100% to obtain solidified hydroxyapatite or calcium-permeable apatite,[80]which is similar to human bone tissue. Hence there produced the mixture of Ca(OH)2and CPC. The irregular shape of the CPC powder particles is beneficial for release of loaded calcium hydroxide, and osteoblasts are less influenced by particle diameters > 10 µm.[81]In addition to the advantages of PMMA, CPC also has the advantages of slow degradation, quick release of drugs, and long-term maintenance of drug efficacyin vivo. Its advantages of good biocompatibility, biodegradability,and promotion of bone healing have allowed CPC to rapidly replace PMMA, and CPC has become a hot spot in the treatment of osteomyelitis.
Conclusions and Prospects
In summary, the current diagnosis and treatment of osteomyelitis remain a difficult problem for clinicians. In recent advances in experimental and clinical studies of osteomyelitis, it has become especially important to elucidate the mechanisms of bacterial adhesion, biofilm formation, intracellular infection from the point of view of pathology and molecular biology.On the basis of its pathogenesis, combining with clinical manifestations and various diagnostic techniques and therapeutic methods, there still needs many of experimental and clinical data to develop a complete and unified path for diagnosing and treating chronic osteomyelitis. Developing more effective strategies to diagnose and intervene in a timely manner, increases the cure rate significantly, shortens the duration of the disease, and reduces the economic burden of patients. Many new methods and technologies have a bright future, but need further exploration and research.
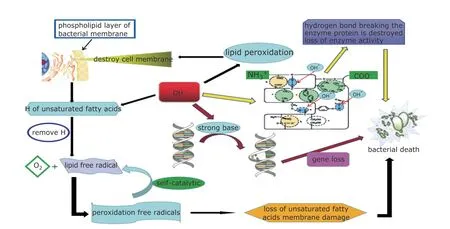
Figure 1. Three sterilization mechanisms of OH- which eventually lead bacteria to die through different routes: increasing bacterial cell membrane permeability(); protein denaturation;(); DNA damage:().
Conflicts of interest statement
All authors declare no conflicts of interest.
 Chinese Medical Sciences Journal2019年3期
Chinese Medical Sciences Journal2019年3期
- Chinese Medical Sciences Journal的其它文章
- Regional Differences of the Urinary Proteomes in Healthy Chinese Individuals
- Identification of CDK6 and RHOU in Serum Exosome as Biomarkers for the Invasiveness of Non-functioning Pituitary Adenoma
- Five-year Clinical Outcomes of CAD Patients Complicated with Diabetes after StentBoost-optimized Percutaneous Coronary Intervention
- Downregulation of iASPP Expression Suppresses Proliferation,Invasion and Increases Chemosensitivity to Paclitaxel of Head and Neck Squamous Cell Carcinoma In Vitro
- Value of CT-Angiography in the Emergency Management of Severe Hemoptysis
- IL-36β Promotes Inflammatory Activity and Inhibits Differentiation of Keratinocytes In Vitro
