Five-year Clinical Outcomes of CAD Patients Complicated with Diabetes after StentBoost-optimized Percutaneous Coronary Intervention
Qiang Chen, Liwei Zhang, Dangsheng Huang, Chunhong Zhang,Qiushuang Wang, Dong Shen, Minjun Xiong, Feifei Yang*
Department of Cardiology, The Fourth Medical Center of Chinese PLA General Hospital, Beijing 100048, China
Key words: percutaneous coronary intervention; diabetes mellitus; stent; prognosis
Objective To evaluate the instant effects and five-year clinical outcomes of coronary artery disease patients complicated with diabetes mellitus after StentBoost-optimized percutaneous coronary intervention (PCI).Methods From March 2009 to July 2010, 184 patients undergoing PCI at our hospital were found stent underexpansion or malapposition by StentBoost after stents implantation and were divided into the diabetic(n=73, 39.67%) and the non-diabetic group (n=111, 60.33%). All patients received StentBoost-guided post-dilatation after stent implantation. The instant procedural results were measured and clinical outcome after five-year follow-up was analyzed in each group. Between-group comparisons were performed using Chi-square test or Student’s t test. Multivariate logistic regression analysis was carried out to reveal the independent predictors for long-term clinical outcomes of StentBoost-optimized PCI .Results After StentBoost-guided post-dilatation, the minimum diameter (MinLD), maximum diameter (MaxLD)and average diameter in both groups increased significantly than before (P<0.001), the (MaxLD-MinLD)/MaxLD ratio and the in-stent residual stenosis decreased accordingly (P<0.001). The five-year follow-up showed similar mortality rate (4.92% vs. 2.86%, P=0.67) and major adverse cardiac event rate (11.48% vs. 11.43%, P= 1.0) between the diabetic and the non-diabetic group, whereas the recurrence of angina pectoris was higher in the diabetic group compared to the non-diabetic group (47.54% vs. 29.52%; P=0.02). A multivariate logistic regression analysis revealed that age and left ventricular ejection fraction rather than diabetes mellitus were independent predictors for long-term clinical outcomes.Conclusions StentBoost could effectively improve instant PCI results; the long-term clinical outcomes of StentBoost-optimized PCI were similar between diabetic and non-diabetic patients. Age and left ventricular ejection fraction were the independent predictors for long-term clinical outcomes.
DIABETES mellitus (DM) is the equivalent of coronary artery disease (CAD) and a significant cardiovascular risk factor.[1]Patients with DM complicating CAD may have an increased mortality rate and repeated revascularization incidence,[2]partly due to more diffuse or complex lesions as compared to those without DM.[3,4]In addition, stent under-expansion has been confirmed as an important reason for in-stent restenosis in DM patients after percutaneous coronary intervention (PCI) regardless of the stent types.[5,6]Thus, post-dilatation at high pressure with noncompliant balloon could optimize stent deployment and reduce the frequency of stent restenosis or target vessel revascularization (TVR).[7,8]
StentBoost (SB) is a newly developed technology that facilitates the angiographic visualization of stent,which could identify stent under-expansion and guide post-dilatation effectively by highlighting the stent profile through a motion compensation technique.[9]About more than 20% of stents under-expansion could be detected by SB as compared to conventional coronary angiography.[10]Though intravascular ultrasound (IVUS)is the gold standard for detecting stent under-expansion to date,[11]we have previously confirmed a superior correlation between SB and IVUS than that between IVUS and coronary angiography.[12]Moreover, SB did not increase both the procedure costs and radiation exposure,[13]which makes it more feasible to be performed as compared to IVUS. The routine use of SB during PCI has also been shown to improve better midterm angiographic and clinical outcomes,[14]however few reports have evaluated the efficacy of long-term prognosis of SB-guided PCI, especially in DM patients.Thus, our prospective study sought to investigate the instant PCI effects and long-term outcomes in these subgroup patients through five-year clinical follow-up.
PATIENTS AND METHODS
Study population
From March 2009 to July 2010, 552 patients received PCI in our department, 184 cases (33.33%) of them were found stent under-expansion or malapposition by SB after stents deployment, SB-guided post-dilatation were applied and then the patients were divided into the DM group (n=73, 39.67%) and the non-DM group(n=111, 60.33%). Baseline clinical characteristics were compared between two groups. Patients with acute myocardial infarction receiving emergency PCI were excluded. All the patients were informed about the research details and consent forms were obtained. The study protocol was approved by the ethics committee of our hospital.
SB-optimized PCI
All patients received 300 mg of aspirin and 300 mg of clopidogrel prior to the procedures. Heparin (1mg/kg body weight) was administered at the beginning of the operation to maintain an activated clotting time (ACT)for 250-300 s. All angiographic images were acquired with the Allura Xper FD 20 digital, flat-panel cardiac imaging system (Philips Medical Systems, Bothell, WA,USA). The treated lesions were classified according to the ACC/AHA lesion angiographic classification system.[11]
Briefly >75% stenosis of diameter was visually considered as a target lesion, and the number and position of the vessels was calculated as baseline lesion characteristics. All procedures were performed following standard interventional techniques. After stent implantation, SB was used to firstly detect stent underexpansion or malapposition: a balloon (usually noncompliant) was placed within the stent segment;afterwards a three-second digital cineangiogram without contrast injection was acquired and automatically analyzed by the system, and the balloon markers were considered as spatial reference points to display the stent profiles automatically. Then quantitative coronary angiography (QCA) was applied to measure the lengths and parameters of the stent by taking a catheter lumen size of 2 mm as reference: minimal diameter (MinLD), maximal diameter (MaxLD), average diameter, (MaxLD-MinLD)/MaxLD ratio, early gain and residual stenosis, as the indexes for instant PCI effects.The results were discussed by two interventional cardiologists to determine whether further high pressure post-dilatation was necessary. If post-dilatation was done, SB was applied to confirm complete stent expansion and the above parameters were measured again as instant PCI results at the end of the operation.
Clinical outcomes and five-year follow-up
Clinical follow-up was performed five years after the procedure, which consisted of outpatient visit, telephone interview or coronary angiography review. All clinical outcomes included: all-cause death, cardiac death, recurrent angina pectoris (self-report), major adverse clinical events [MACEs; non-fatal acute myocardial infarction (AMI), target lesion revascularization(TLR), and target vessel revascularization (TVR)].
Statistical analysis
The continuous variables were presented as mean values ± standard deviation and categorical variables were presented as frequency (%). Between-group comparisons were quantified using theChi-squaretest or Student’sttest. To assess the determinants of outcomes,multivariate logistic regression analyses were performed and logistic odds ratios (ORs) with 95% confidence intervals (CIs) were obtained. All analyses were performed using SPSS 22.0 software (IBM, Chicago, IL,USA). Two-tailed probability (P) values <0.05 were set as the threshold for statistical significance.
RESULTS
Baseline clinical characteristics
As shown in Table 1, no differences were observed in age, gender, PCI history, prior myocardial infarction,hypertension, hyperlipidemia, smoking status and left ventricular ejection fraction (LVEF) between the two groups (allP> 0.05).
PCI procedural characteristics
As shown in Table 2, no differences were observed in baseline lesion parameters, details of stent implantation and instant PCI results between the two groups (allP> 0.05).

Table 1. Comparisons of baseline clinical characteristics of the two groups

Table 2. Comparisons of PCI procedural characteristics between the two groups
SB-guided post-dilatation measurements
As shown in Table 3, after post-dilatation in the both groups, the in-stent MinLD, MaxLD and average diameter increased significantly as compared to those before post-dilatation, respectively (P< 0.001). Accordingly,the (MaxLD-MinLD)/MaxLD ratio and in-stent residual stenosis decreased significantly (P< 0.001). No differences were observed in diameters mentioned above between the two groups post-dilatation (P> 0.05, Table 2).
Clinical outcomes of five-year follow-up
Finally, 166 (90.22%) out of the 184 cases were followed successfully. As shown in Table 4, the recurrent rate of angina pectoris in the DM group was higher than that in the non-DM group (47.54%vs. 29.52%,P=0.020), but no differences were observed in rates of death, cardiac death, MACEs between the two groups(P>0.05).
Multivariate analysis to identify risk factors predicting mortality
Multivariate analysis showed DM did not serve as an independent predictor of mortality (OR: 1.07; 95%CI:0.002-2.637;P= 0.151), but age (OR: 1.605; 95%CI:1.045-2.457;P= 0.031) and LVEF (OR: 0.845;95%CI: 0.727-0.982;P= 0.028) were independent predictors for mortality during follow-up.
DISCUSSION
In this prospective study, we proved that the DM patients undergoing SB-optimized PCI acquired ideal instant effects and similar long-term outcomes as compared with the non-DM patients.
The SB technology has been used frequently to evaluate stent positioning and expansion, which provided superior resolution over conventional angiography through enhancing stent visualization.[15-17]Moreover, there was a positive correlation between SB and IVUS.[18]Mishellet al.[19]reported the correlation of MinLD between SB and IVUS was higher (r= 0.75;P< 0.0001) than that between QCA and IVUS (r=0.65;P< 0.0001). We also reported the superior correlations of MinLD, MaxLD and (MaxLD-MinLD)/MaxLD ratio between SB and IVUS than those between QCA and IVUS previously (P< 0.0001).[12]In this study, the MinLD, MaxLD, average diameter increased significantly, the (MaxLD-MinLD)/MaxLD ratio and residual stenosis of stents decreased significantly after SB-guided post-dilatation (P< 0.001) in both the groups, but the differences between the DM and the non-DM group were not significant after dilatation (P> 0.05), suggesting that both the DM and non-DM patients could benefit from SB technology and achieve ideal instant PCI effects.
Only a few researches concerned about the clini-cal outcomes of patients undergoing SB-guided PCI. Ohet al.[14]reported the instant (one month) outcomes between the SB-group and the non-SB group were similar, but the rates of TLR and TLR-related MACE were lower at mid-term (twelve months) follow-up (P<0.05)in the SB-group. However the long-term outcomes of SB-guided PCI remain unknown, especially in the DM patients. According to our five-year follow-up results,the rates of all-cause death, cardiac death and MACEs were similar between the DM and non-DM groups(P>0.1), and the rates of revascularization, TLR, as well as TVR were also similar between the two groups(P>0.1). The results demonstrated that DM patients might achieve similar long-term outcomes as compared with non-DM patients after SB-guided PCI.
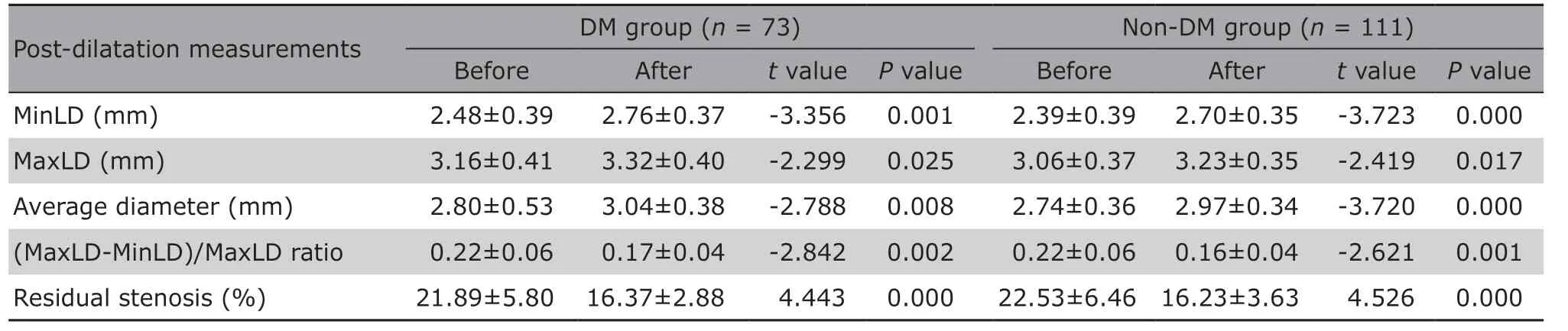
Table 3. SB-guided post-dilatation measurements compared with those before post-dilatation§

Table 4. Comparisons of clinical outcomes of five-year follow-up between the two groups (%)
DM usually presents with endothelial dysfunction,excessive inflammatory activities and heavy plaque burden[20]that lead to increased risk of revascularization.[21]In addition, stent underexpansion was considered as a primary reason for revascularization,especially in DM patients, no matter what type of stent was used.[5]Routine post-dilatation using noncompliant balloon at high pressure could improve instant PCI effects and subsequently reduce the rates of MACE and TLR in the patients with drug-eluting stents implantation.[22]However “optimal” effects of stent deployments were rarely achieved according to Cheneauet al’s research,[23]which could be improved under IVUS measurements. Given that extra fees and operation skills were required for IVUS, SB could be the potential substitution just as mentioned before.[18]In our study, an adequate post-dilatation was applied and no differences in post-dilated diameters were observed between the two groups (P>0.05), which might partly explain a similar long-term outcome in the DM group, with similar rates of all-cause death, cardiac death, revascularization, TLR and TVR as compared to the non-DM group.
The recurrence of angina pectoris of the DM group was higher (DM 47.54%vs. non-DM 29.52%,P< 0.05) during the follow-up, which is consistent with Arnoldet al’s research.[24]Some functional mechanisms such as microvascular dysfunction or vasospasm etc.were involved in angina after PCI,[25]especially in DM patients.[26]Besides, the restenosis rate after PCI was higher in the DMvs. non-DM patients. Taken together,these might contribute to a higher recurrence rate of angina pectoris in the DM group, even though the basic clinical and coronary arterial characteristics were similar among those with or without DM in our study.However the microvascular functions were not evaluated in our study, and other factors such as medications or lifestyles etc. also deserved careful investigations in the future.
Through a multivariate logistic regression analysis, age and LVEF were defined as the independent predictors of mortality during follow-up. Aged patients may have more comorbidities, and thereby resulting in worse clinical outcome.[27]And the HORIZONS-AMI trial established that lower LVEF is a powerful predictor of both early and late mortality in patients undergoing primary PCI,[28]our study drew the same conclusion as well. In some researches DM might be a predictor of mortality,[29]in our study a trend toward higher mortality was observed in the DM group (OR: 1.07, 95%CI:0.002-2.637), however no significant difference was found (P=0.151), thus, DM could not serve as an independent predictor of mortality. In other words, both groups achieved similar long-term outcomes after SB-guided PCI irrespective of the DM status.
In conclusion, our study confirmed an ideal instant effects of SB-optimized PCI in both the DM and non-DM patients. And the long-term clinical outcomes of SB-optimized PCI were similar between the two groups. Age and LVEF were the independent predictors of mortality during follow-up.
There are several limitations for our study. Firstly,it was a single center study with limited sample size,meanwhile all patients were not assigned randomly into each group. The results required further investigation by larger-scale random, double-blinded trials.Secondly, all patients received drug-eluting stents implantation in the study. However, differences between different types of stents might exist and we did not make further analysis. Thirdly, about 10% of the patients were lost during follow-up, this might influence the study results. Finally, different glycemic levels of DM patients might also influence the final result, which also deserved further investigation.
Conflicts of interest statement
The authors declare no conflicts of interest.
 Chinese Medical Sciences Journal2019年3期
Chinese Medical Sciences Journal2019年3期
- Chinese Medical Sciences Journal的其它文章
- Research on the Antitumor Compounds from Cephalotaxus Hainanensis
- Artificial Musk R&D and Manufacturing
- Management of an Adult with Goodpasture’s Syndrome Following Brain Trauma with Extracorporeal Membrane Oxygenation: A Case Report
- Transvaginal Reduction of a Heterotopic Cornual Pregnancy with Conservation of Intrauterine Pregnancy
- Research Progress on Diagnosis and Treatment of Chronic Osteomyelitis
- Association between GSTT1 Homozygous Deletion and Risk of Pancreatic Cancer: A Meta Analysis
