黄韧带骨化所致胸椎管狭窄症脊髓MRI信号改变与手术效果关系
王德训 王亭 郭建伟 侯建文 王其尊 李书忠

[摘要]目的探討胸椎黄韧带骨化(TOLF)所致的胸椎管狭窄症(TSS)脊髓MRI T2加权像上信号改变与手术预后的相关性。方法选取手术治疗的TOLF病人69例,所有病人术前均行胸椎CT检查证实为TOLF所致的TSS,术前均行胸椎MRI检查明确脊髓信号情况。根据MRI所示髓内信号情况进行分组,脊髓内信号正常者44例(A组),脊髓内信号出现改变者25例(B组)。所有病人均行后入路胸椎椎管减压内固定术,分别于术前、术后3个月及末次随访行日本骨科学会(JOA)评分及下肢肌力评定,计算JOA评分改善率及肌力改善情况并进行比较。结果B组术前、术后3个月及末次随访JOA评分均低于同时期A组,各随访时间JOA评分改善率低于A组,差异有统计学意义(t=3.459~4.357,P<0.01)。两组组内比较,JOA评分术后3个月较术前、末次随访较术后3个月均有改善,差异有统计学意义(F=114.473、34.983,P<0.01)。两组术后3个月、末次随访肌力分级与术前比较,差异均有显著性(χ2=55.280、15.055,P<0.05)。结论术前存在脊髓MRI T2加权信号改变的TOLF病人,手术治疗后效果明显,但是手术效果劣于术前脊髓信号正常TOLF病人。
[关键词]胸椎;椎管狭窄;黄韧带;核磁共振成像;脊髓损伤;疗效比较研究
[ABSTRACT]ObjectiveTo investigate the association of signal changes on the MRI T2`-weighted image of the spinal cord with surgical outcome in patients with thoracic spinal stenosis (TSS) caused by thoracic ossification of the ligamentum flavum (TOLF). MethodsA total of 69 patients with TOLF who underwent surgical treatment were enrolled. All patients underwent thoracic spinal CT before surgery to confirm TSS caused by TOLF. Thoracic spinal MRI was performed before surgery to observe the signals of the spinal cord. According to the intraspinal signals on MRI, the patients were divided into group A (44 patients with normal intraspinal signals) and group B (25 patients with changes in intraspinal signals). All patients underwent thoracic spinal decompression and internal fixation via the posterior approach. The Japanese Orthopedic Association (JOA) score and muscle strength of the lower limbs were evaluated before surgery and at 3 months after the surgery, the improvement rate of JOA score and the improvement in muscle strength were calculated and compared between groups. ResultsCompared with group A, group B had a significantly lower JOA score before surgery, at 3 months after surgery, and at the last follow`-up, as well as a significantly lower improvement rate of JOA score at each follow`-up (t=3.459-4.357,P<0.01). Both groups had a significant improvement in JOA score from before surgery to 3 months after surgery and from 3 months after surgery to the last follow`-up (F=114.473,34.983;P<0.01). Both groups had a significant change in muscle strength at 3 months after surgery and at the last follow`-up (χ2=55.280,15.055;P<0.05). ConclusionPatients with TOLF who have changes in spinal cord signals on T2`-weighted MRI before surgery tend to have a good outcome after surgery, but their surgical outcomes are poorer than patients with normal spinal signals before surgery.
[KEY WORDS]thoracic vertebrae; spinal stenosis; ligamentum flavum; magnetic resonance imaging; spinal cord injuries; comparative effectiveness research
胸椎黄韧带骨化(TOLF)所致的胸椎管狭窄症(TSS)是一种发病率低且起病隐匿的临床病症,多表现为TOLF压迫脊髓平面以下出现躯体感觉及运动功能障碍,如下肢疼痛、麻木无力甚至是大小便障碍等[1`-2]。目前, TOLF尚无明确有效的保守治疗方式,手术治疗为公认的首选治疗方式[2]。CT结合MRI是诊断TOLF所致TSS首要的检查方法,既能判断椎管内黄韧带骨化物的大小、位置、累及节段等情况,还能判断毗邻脊髓的受压及损伤情况[3`-4]。正常脊髓MRI的T1加权像及T2加权像上表现为中等信号强度,但是某些病程长、压迫严重的病人MRI显示信号改变,而在T2加权像上则多显示高信号强度的条索状或斑块样改变,其发生率为41%~79%[5]。脊髓信号改变对于病人术后疗效的影响,不同文献报道结果不一致,且多见于颈椎疾病报道[6]。本文对TOLF所致TSS脊髓内信号改变与术后疗效关系进行分析,探讨MRI脊髓内信号改变与TOLF所致TSS病人术后预后的相关性。
1资料与方法
1.1一般资料
选取2014年1月—2018年1月在我院行胸椎后路椎板切除、椎管减压内固定术的TOLF所致TSS病人69例。纳入标准:①术前CT检查证实存在TOLF;②术前MRI证实存在胸椎脊髓受压情况;③存在脊髓受压导致的神经症状;④所有病人均接受了胸椎后路椎板切除、椎管减压内固定术。排除标准:①合并颈椎或者腰椎疾患的病人;②合并胸椎间盘突出或者胸椎后纵韧带骨化;③合并糖尿病或者其他周围神经病变病人;④其他脊柱疾病或者肿瘤疾病病人。根据病人MRI的T2加权像上脊髓信号变化分为2组。脊髓内信号正常者44例为A组,男19例,女25例;年龄36~76岁,平均(59.4±10.3)岁;病程2~48个月,平均12个月;术前日本骨科学会(JOA)评分5~8分,平均(6.5±1.0)分;术前下肢肌力Ⅲ级13例,Ⅳ级27例,Ⅴ级4例。脊髓信号改变者25例为B组,男10例,女15例;年龄44~82岁,平均(63.7±1.0)岁;病程4~42个月,平均12个月;术前JOA评分4~8分,平均为(6.1±1.1)分。术前下肢肌力Ⅲ级者11例,Ⅳ级者14例。两组病人年龄、性别、病程等差异均无统计学意义(P>0.05)。
1.2手術方法
所有病人麻醉后取俯卧位,C型臂X线机行术前定位,常规消毒铺巾后,以责任节段为中心行后入路正中切口,逐层分离筋膜、椎旁肌至两侧关节突附近,充分暴露责任节段两侧关节突,在手术节段两侧椎弓根植入椎弓根螺钉,使用高速磨钻沿关节突内侧磨薄骨质,直至椎板骨质呈半透明状态,然后在椎板最薄处使用椎板咬骨钳咬除骨质,期间用神经剥离子分离保护硬膜囊,防止硬膜囊与骨化黄韧带粘连导致术中硬膜破裂;无法分离者则在保护硬膜囊的基础上尽量打磨椎板骨质。在责任节段两侧放置钛棒固定后,透视椎弓根钉棒固定位置良好,生理盐水冲洗手术视野,放置20 mm直径引流管,双极电凝止血出血点,依次关闭手术切口。
1.3手术疗效评价
两组分别于术前、术后3个月及末次随访时,应用JOA评分 [7]评价脊髓神经功能,以术后3个月及末次随访的胸椎JOA评分以及JOA评分改善率(IR)分级变化评价手术疗效。IR=(术后JOA评分-术前JOA评分)÷(胸椎JOA评分-术前JOA评分)×100%。手术疗效评价:以IR≥75%为优, 50%~74%为良, 25%~49%为中,<25%者为差。两组病人分别于术前、术后3个月及末次随访时,采用LOVETT肌力分级评估下肢肌力,以下肢肌力分级变化评估手术疗效。
1.4统计学处理
应用SPSS 20.0软件进行统计学处理, Kolmogorov`-Smirnov正态分布检验法检验变量的分布,满足正态分布的计量资料用±s表示,多组数据比较采用重复测量数据的方差分析,两组间比较采用t检验;计数资料用频数(百分比)表示,组间比较采用卡方检验。P<0.05为差异有统计学意义。
2结果
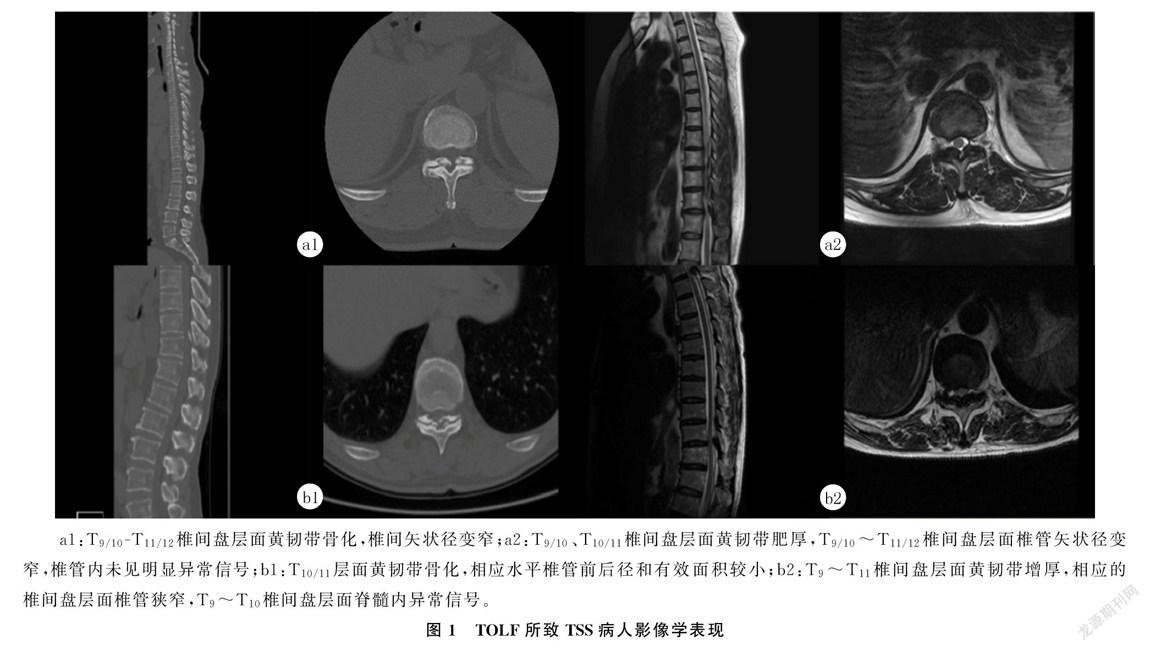
所有病人术前均存在TOLF的影像学证据(图1a1、b1),T9/10、T10/11椎间盘层面黄韧带骨化。但是A组病人MRI T2加权像可见黄韧带增生肥厚,而脊髓内未见异常信号(图1a2),T9/10~T11/12椎间盘层面椎管矢状径变窄,椎管内未见明显异常信号。B组病人的MRI T2加权像中不仅可见黄韧带增生肥厚,还可见脊髓内有长条状或者斑片状的高信号影(图1b2),T9~T11椎间盘层面黄韧带增厚,相应的椎间盘层面椎管狭窄,T9~T10椎间盘层面脊髓内异常信号。病人分组和随访时间之间存在交互作用(F组别×时间=5.006,P<0.05),随着手术随访时间的增加,两组JOA评分均增加,两组病人术后3个月及末次随访的JOA评分均高于术前,末次随访的IR优于术后3个月,差异有统计学意义(F=114.473、34.983,P<0.01)。B组术前、术后3个月及末次随访JOA评分均低于同时期A组,各随访a1:T9/10`-T11/12椎间盘层面黄韧带骨化,椎间矢状径变窄;a2:T9/10、T10/11椎间盘层面黄韧带肥厚,T9/10~T11/12椎间盘层面椎管矢状径变窄,椎管内未见明显异常信号;b1:T10/11层面黄韧带骨化,相应水平椎管前后径和有效面积较小;b2:T9~T11椎间盘层面黄韧带增厚,相应的椎间盘层面椎管狭窄,T9~T10椎间盘层面脊髓内异常信号。
时间IR低于A组,差异有统计学意义(t=3.459~4.357,P<0.01)。两组术后3个月、末次随访肌力分级与术前比较,差异均有显著意义(χ2=55.280、15.055,P<0.05)。见表1。
3讨论
TOLF所致TSS椎管内MRI信号改变很早就被学者们注意到,已有研究结果显示TOLF病人中MRI T2加权像上高信号改变的发生率为41%~79%[5,8]。LIAO等[9]研究显示,24例TOLF病例中有11例出现不同程度的MRI T2加权像高信号改变,占病例总数的45.8%。本文研究显示,TOLF所致TSS病人术前MRI T2加权像上出现斑片状或长条狀高信号改变25例,占总数的36.2%,与文献结果不一致原因可能与样本纳入标准不同有关。目前,手术是TOLF所致TSS首选的治疗方案[10`-12],但是针对椎管内脊髓MRI信号改变与术后疗效的分析报道多见于颈椎疾病方面,而关于TOLF所致TSS脊髓MRI信号改变与手术疗效关系的报道较少,且对术前脊髓信号改变是否影响术后疗效的认识存在分歧[13`-15]。大多数学者认为,脊髓MRI信号的改变与脊髓局部受压有关[16`-17]。经过充分手术减压,脊髓水肿将会消失,随后神经功能恢复。因此,脊髓内MRI信号改变与术后疗效并无明显相关性。有研究指出,脊髓信号改变是由于脊髓发生水肿变性等可逆性变化导致,在解除脊髓机械性压迫后,脊髓水肿信号会迅速消失,因此脊髓信号升高与病人手术预后无明显关联[8,18`-19]。
本文研究结果显示,相同时间点脊髓信号改变组的JOA评分及IR显著低于脊髓内信号正常组,差异有显著性;并且脊髓信号改变组术后3个月LOVETT肌力评分较术前、末次随访较术后3个月虽然都有一定的改善,但是其改善程度低于无信号改变组,说明术前脊髓存在MRI T2加权像上高信号改变的病人,预后要差于术前脊髓无MRI T2加权信号改变病人。有研究显示,术前合并脊髓MRI T2加权像高信号病人IR低于术前脊髓信号正常组,推测其原因可能与脊髓受损伤程度有关[20]。脊髓病理性变化与受压时间密切相关,因此我们推测受压时间也是影响术后疗效的重要因素,脊髓受压时间越长,脊髓发生不可逆损伤可能性越大,越容易出现脊髓坏死、液化等情况[21]。有研究结果表明,术前病人脊髓信号改变往往是由于脊髓坏死、空洞等不可逆损伤导致的,脊髓坏死、液化、空洞等均是不可逆的病理变化,即使是通过手术对受压脊髓进行充分解压,其不可逆的病理变性也不能得到恢复,脊髓T2加权像高信号术后不易恢复正常,甚至受损脊髓会因为解除压迫后出现缺血再灌注损伤而导致脊髓功能进一步受损[22`-23]。术前MRI T2加权像高信号改变提示脊髓变性,可逆性的脊髓变性在解除压迫后脊髓T2加权像上高信号可得到不同程度的恢复[24`-27]。即使脊髓功能得到一定程度的恢复,也预示着术后恢复缓慢,脊髓神经功能恢复较差;存在MRI T2加权像上高信号改变的病人术后神经功能可得到一定程度的恢复,但是改善程度较脊髓信号正常病人差。
本研究为回顾性研究,存在一定的局限性。①由于TOLF起病隐匿、症状进展缓慢等原因,病人脊髓硬膜囊受压的时间无法准确统计,而脊髓MRI信号改变及其程度与脊髓受压时间密切相关,脊髓MRI信号改变提示已经出现脊髓水肿、脊髓软化或脊髓空洞。在脊髓受压初期多出现脊髓水肿或脊髓软化,术后解除压迫病人神经功能恢复较迅速[28];而一旦压迫时间过长则可能会出现脊髓空洞坏死等不可逆的病理变化,多预示着术后恢复不良[25,29`-30]。②脊髓MRI T2加权像上信号改变程度暂无统一的评价标准,一些临界性脊髓信号改变尚缺乏共识,因此导致脊髓MRI信号改变分级、分期标准制定出现争议[31`-32]。这些因素都为判断脊髓MRI信号改变是否影响术后疗效增加了难度[27,33]。同时,TOLF手术预后不能单纯以病人影像资料加以判断,而应该综合考虑病人的基础状态、TOLF影像学资料及TOLF分型和累及范围等因素[6,24]。
综上所述,TOLF所致TSS病人无论脊髓MRI T2加权像上信号改变与否,手术治疗后都能取得一定程度的恢复。但是术前脊髓存在MRI T2加权像上高信号改变的病人,预后效果要差于术前脊髓无MRI T2加权像信号改变病人。
[参考文献]
[1]GUO J J, LUK K D K, KARPPINEN J, et al. Prevalence, distribution, and morphology of ossification of the ligamentum flavum a population study of one thousand seven hundred thirty`-six magnetic resonance imaging scans[J]. Spine, 2010,35(1):51`-56.
[2]宁尚龙,陈仲强,马信龙,等. 胸椎黄韧带骨化基础与临床研究进展[J]. 中国矫形外科杂志, 2017,25(11):999`-1004.
[3]陈农,董健. 胸椎黄韧带骨化的基础与诊断治疗进展[J]. 中国矫形外科杂志, 2010,18(5):389`-392.
[4]曹家敏,王清,王高举,等. 探讨MRI在颈椎管狭窄伴脊髓损伤中的诊断价值[J]. 中国修复重建外科杂志, 2009,23(7):800`-802.
[5]INAMASU J, GUIOT B H. A review of factors predictive of surgical outcome for ossification of the ligamentum flavum of the thoracic spine[J]. Journal of Neurosurgery`-Spine, 2006,5(2):133`-139.
[6]赵宇. 脊髓MRI信号改变与胸椎管狭窄症手术预后的关系[J]. 中国脊柱脊髓杂志, 2014,24(7):580`-581.
[7]FUKUI M, CHIBA K, KAWAKAMI M, et al. Japanese orthopaedic association back pain evaluation questionnaire. part 2. verification of its reliability: the subcommittee on low back pain and cervical myelopathy evaluation of the clinical outcome committee of the Japanese orthopaedic association[J]. Journal of Orthopaedic Science, 2007,12(6):526`-532.
[8]TAKENAKA S, KAITO T, HOSONO N, et al. Neurological manifestations of thoracic myelopathy[J]. Archives of Orthopaedic and Trauma Surgery, 2014,134(7):903`-912.
[9]LIAO C C, CHEN T Y, JUNG S M, et al. Surgical expe`-rience with symptomatic thoracic ossification of the ligamentum flavum[J]. Journal of Neurosurgery`-Spine, 2005,2(1):34`-39.
[10]SUN Jingcheng, ZHANG Chao, NING Guangzhi, et al. Surgical strategies for ossified ligamentum flavum associated with dural ossification in thoracic spinal stenosis[J]. Journal of Cli`-nical Neuroscience, 2014,21(12):2102`-2106.
[11]ANDO K, IMAGAMA S, KOBAYASHI K, et al. Comparative study of surgical treatment and nonsurgical follow up for thoracic ossification of the posterior longitudinal ligament: radiological and clinical evaluation[J]. Spine, 2017,42(6):407`-410.
[12]吳德鹏,裴磊,袁伟,等. 胸椎黄韧带骨化症的临床特点及手术治疗[J]. 中华骨与关节外科杂志, 2018,11(1):30`-34.
[13]KATO S, NOURI A, REIHANI`-KERMANI H, et al. Postoperative resolution of magnetic resonance imaging signal intensity changes and the associated impact on outcomes in degenerative cervical myelopathy analysis of a global cohort of patients[J]. Spine, 2018,43(12):824`-831.
[14]魏磊鑫,田野,华东方,等. 多节段脊髓型颈椎病伴髓内MRI T2WI高信号改变患者的手术入路选择及疗效分析[J]. 中国脊柱脊髓杂志, 2016,26(2):101`-107.
[15]刘晓光. 胸椎管狭窄症患者MRI髓内高信号的原因及对预后的影响[J]. 中国脊柱脊髓杂志, 2014,24(7):581`-582.
[16]YONE K, SAKOU T, YANASE M, et al. Preoperative and postoperative magnetic resonance image evaluations of the spinal cord in cervical myelopathy[J]. Spine, 1992,17(10 Suppl): S388`-S392.
2期王德训,等. 黄韧带骨化所致胸椎管狭窄症脊髓MRI信号改变与手术效果关系163
[17]NOURI A, MARTIN A R, MIKULIS D, et al. Magnetic re`-sonance imaging assessment of degenerative cervical myelopathy: a review of structural changes and measurement techniques[J]. Neurosurgical Focus, 2016,40(6): E5.
[18]ALAFIFI T, KERN R, FEHLINGS M. Clinical and MRI predictors of outcome after surgical intervention for cervical spondylotic myelopathy[J]. Journal of Neuroimaging, 2007,17(4):315`-322.
[19]SHIOKAWA K, HANAKITA J, SUWA H, et al. Clinical analysis and prognostic study of ossified ligamentum flavum of the thoracic spine[J]. Journal of Neurosurgery, 2001,94(2, S):221`-226.
[20]王林峰. 胸椎管狭窄症脊髓高信号的基础研究与临床预后分析[D]. 石家庄:河北医科大学, 2014.
[21]贾宁阳. 脊髓损伤的病理变化及其与磁共振成像演变[J]. 中国矫形外科杂志, 1998,6(3):63`-64.
[22]李凤宁,张帆,何平,等. MRI T2加权像伴有髓内高信号的轻度脊髓型颈椎病的治疗[J]. 脊柱外科杂志, 2014,12(3):156`-160.
[23]刘晓明,张锐光,李小强. 胸椎管狭窄症后路手术疗效及相关影响因素分析[J]. 临床医药文献杂志, 2018,5(62):16.
[24]KUH S U, KIM Y S, CHO Y E, et al. Contributing factors affecting the prognosis surgical outcome for thoracic OLF[J]. European Spine Journal, 2006,15(4):485`-491.
[25]HE S S, HUSSAIN N, LI S H, et al. Clinical and prognostic analysis of ossified ligamentum flavum in a Chinese population[J]. Journal of Neurosurgery`-Spine, 2005,3(5):348`-354.
[26]张健,贾连顺,陈雄生,等. 颈脊髓信号改变对颈椎后纵韧带骨化手术疗效的影响[J]. 中国矫形外科杂志, 2017,25(17):1541`-1545.
[27]贺宝荣,许正伟,郝定均,等. 胸椎黄韧带骨化症患者髓内MRI高信号与手术疗效的关系[J]. 中国脊柱脊髓杂志, 2014,24(10):928`-932.
[28]曲景文,马清田,张希诺,等. 脊髓型颈椎病减压术后早期脊髓MRI T2WI信号改变对临床疗效的影响[J]. 中国骨与关节杂志, 2018,7(10):744`-749.
[29]WANG Linfeng, LIU Fajing, ZHANG Yingze, et al. Clinical results and intramedullary signal changes of posterior decompression with transforaminal interbody fusion for thoracic myelopathy caused by combined ossification of the posterior longitudinal ligament and ligamentum flavum[J]. Chinese Medical Journal, 2013,126(20):3822`-3827.
[30]刘法敬,丁晓坤,曹俊明,等. 胸椎管狭窄程度与脊髓内高信号及临床症状的相关性研究[J]. 现代中西医结合杂志, 2014,23(33):3664`-3666.
[31]董健. 胸椎管狹窄症术后疗效与脊髓MRI T2WI高信号的关系[J]. 中国脊柱脊髓杂志, 2014,24(7):582`-583.
[32]冯法博,孙垂国,陈仲强,等. “揭盖式”胸椎管后壁切除术治疗单节段胸椎黄韧带骨化症的疗效及其影响因素[J]. 中国脊柱脊髓杂志, 2014,24(7):585`-592.