学龄前儿童骨密度与血清25-(OH)D水平的相关性
邢存乔 陈海琼 曾广萍


[摘要] 目的 调查学龄前儿童骨密度(BMD)状况及其与血清25-羟维生素D[25-(OH)D]的关系。 方法 收集2017年3月~2018年3月629例在三亚市妇幼保健院儿童保健科门诊体检行BMD检查的0~7岁学龄前儿童为研究对象,采用定量超声仪测量BMD,根据BMD水平将研究对象分为BMD正常组(n = 492)和BMD异常组(n = 137)。采用多因素Logistic回归分析法分析学龄前儿童BMD的影响因素;采用酶联免疫吸附法测定25-(OH)水平,比较不同25-(OH)D水平儿童的BMD,并采用Pearson积矩相关分析学龄前儿童BMD与血清25-(OH)D相关性。 结果 学龄前儿童BMD异常率为21.78%。5~7岁儿童BMD异常率较高,1岁儿童其次。女童、1岁及5~7岁儿童BMD异常率高于男童、2~4岁儿童(P < 0.05);活动时间≤3 h/周、睡眠时间≤8 h/d、日照时间≤7 h/d的学龄前儿童BMD异常率高于活动时间>3 h/周、睡眠时间>8 h/d、日照时间>7 h/d儿童(P < 0.05);挑食、维生素D摄入≤400 U/d、奶制品摄入≤150 mL/d、豆制品摄入≤4次/周、水果摄入≤5次/周的学龄前儿童BMD异常率高于不挑食、维生素D摄入>400 U/d、奶制品摄入>150 mL/d、豆制品摄入>4次/周、水果摄入>5次/周儿童(P < 0.05)。与2岁儿童比较,1岁、5~7岁是BMD异常的独立危险因素(OR = 1.113、1.373、1.433、1.479,P < 0.05),活动时间、睡眠时间、日照时间、挑食情况、维生素D摄入、奶制品摄入、豆制品摄入、水果摄入是学龄前儿童BMD异常的影响因素(OR = 1.377、1.654、1.642、1.525、1.788、1.598、1.384、1.443,P < 0.05)。随着25-(OH)D水平的降低,SOS值逐渐增大,Z值逐渐减小,BMD异常率逐渐增加(P < 0.05)。学龄前儿童SOS与血清25-(OH)D呈负相关(r = -0.729,P < 0.05),Z值与血清25-(OH)D呈正相关(r = 0.761,P < 0.05)。 結论 学龄前儿童BMD异常率较高,尤其多见于1岁以前及5~7岁儿童,对BMD异常高危儿童应合理补充维生素D和钙剂,并加强户外活动,注意饮食均衡。
[关键词] 学龄前儿童;骨密度;25-羟维生素D;相关性
[中图分类号] R179 [文献标识码] A [文章编号] 1673-7210(2019)06(b)-0063-05
The correlation between bone mineral density and serum 25-(OH)D level in preschool children
XING Cunqiao CHEN Haiqiong CENG Guangping
Department of Child Health Care, Sanya City Womenfolk and Infant Health Care Hospital, Hainan Province, Sanya 572000, China
[Abstract] Objective To investigate the bone mineral density (BMD) in preschool children and its relationship with serum 25-hydroxyvitamin D [25-(OH)D]. Methods From March 2017 to March 2018, 629 preschool children aged 0-7 who underwent BMD examination in the Outpatient Department of Child Health Care of Sanya City Womenfolk and Infant Health Care Hospital were collected as subjects. BMD was measured by quantitative ultrasound, according to BMD level, the subjects were divided into normal BMD group (n = 492) and abnormal BMD group (n = 137). The influencing factor of BMD of preschool children was analyzed by multivariate Logistic regression analysis. The level of 25-(OH) was determined by ELISA, the BMD of children with different 25-(OH)D level was compared. Pearson product moment correlation analysis was used to analyze the correlation between BMD and serum 25-(OH)D in preschool children. Results The abnormal rate of BMD in preschool children was 21.78%, which in children aged 5-7 was higher than that in others, followed by children aged 1. The abnormal rate of BMD in girls, children aged 1-year-old and 5-7-year-old was higher than that in boys and children aged 2-4-year-old (P < 0.05). The abnormal rate of BMD in preschool children with activity time ≤3 h/week, sleeping time ≤8 h/d, sunshine time ≤7 h/d was higher than that of children whose activity time >3 h/week, sleeping time >8 h/d and sunshine time >7 h/d (P < 0.05). The abnormal rate of BMD in preschool children with picky diet, vitamin D intake ≤400 U/d, dairy intake ≤150 mL/d, bean products intake ≤4 times/week, fruit intake ≤5 times/week was higher than those of children without picky diet, vitamin D intake > 400 U/d, dairy intake >150 mL/d, bean products intake > 4 times/week, fruit intake > 5 times/week (P < 0.05). Compared with 2-year-old children, 1-year-old and 5-7-year-old was independent risk factors for abnormal BMD (OR = 1.113, 1.373, 1.433, 1.479, P < 0.05). Activity time, sleeping time, sunshine time, picky diet, vitamin D intake, dairy intake, bean products intake, fruit intake was the influencing factor of abnormal BMD in preschool children (OR = 1.377, 1.654, 1.642, 1.525, 1.788, 1.598, 1.384, 1.443, P < 0.05). With the decrease of 25-(OH)D level, SOS value increased gradually, Z value decreased gradually, and abnormal rate of BMD increased gradually (P < 0.05).There was a negative correlation between SOS and serum 25-(OH) D in preschool children (r = -0.729, P < 0.05), and a positive correlation between Z value and serum 25-(OH) D (r = 0.761, P < 0.05). Conclusion The abnormal rate of BMD in preschool children is higher, especially in children aged 1 and 5-7 years. Vitamin D and calcium should be supplemented reasonably for children at high risk of BMD, outdoor activities should be strengthened, and balanced diet should be paid attention to.
[Key words] Preschool children; Bone mineral density; 25-hydroxyvitamin D; Correlation
学龄前儿童期是机体新陈代谢、生长发育最活跃的阶段,也是骨量增长、骨骼发育的时期,定量评估骨量可评估学龄前儿童生长发育进度[1]。骨密度(BMD),即骨骼矿物质密度,是指单位面积内骨矿物质的含量,是一项敏感且特异地反映人体骨营养状况的指标,也是目前临床评估骨钙水平,反映人体骨质量常用的客观指标[2]。调查发现[3],学龄期儿童BMD异常率可高达20%~30%,BMD降低的儿童更易出现骨折,同时患佝偻病的风险也明显增加。维生素D参与调节钙、磷代谢,对促进钙吸收和重吸收及其在骨骼中的沉积具有重要作用,研究表明[4]。25-羟维生素D [25-(OH)D]是反映机体中维生素D营养状态的敏感指标,检测BMD可反映25-(OH)D水平,进而评估机体维生素D水平,但也有研究对此尚存争议[5]。本研究通过检测学龄前儿童BMD,旨在了解该地区学龄期儿童BMD与25-(OH)D的关系,旨在为制订学龄期儿童BMD异常干预方案和评估机体维生素D营养状况提供指导。
1 资料与方法
1.1 一般资料
收集2017年3月~2018年3月629例在三亚市妇幼保健院(以下简称“我院”)儿童保健科门诊体检自愿行BMD检查的0~7岁学龄前儿童为研究对象。排除标准:①>7岁的儿童;②肝、肾功能障碍的儿童;③内分泌代谢性疾病、自身免疫性疾病儿童;④畸形性骨炎、成骨发育不全等可能影响本研究结果的骨骼疾病儿童。其中男382例,女247例;年龄0~7岁,平均(4.62±2.08)岁。
1.2 方法
1.2.1 资料采集 在我院儿童保健科门诊由专门经过培训的护士填写儿童基本资料,内容包括性别、年龄、身高、体重,以及儿童活动时间、睡眠情况、日照时间、挑食情况、维生素D摄入、奶制品摄入、豆制品摄入、水果摄入等。
1.2.2 BMD测定 采用Ominisense?誖7000超声BMD检测仪(购自于以色列Sunlight公司)对儿童左侧胫骨远端1/3处进行测量,并记录儿童超声传导速度(SOS),参照亚洲儿童同性别、同龄SOS的Z值评分对所测儿童的BMD进行分类[6]:Z>-1.0定义为BMD正常,Z≤-1.0且>-1.5定义为BMD轻度不足,Z≤-1.5且>-2.0定义为BMD中度不足,Z<-2.0定义为BMD重度不足,本研究根据BMD将儿童分为BMD正常组,BMD轻度、中度和重度不足统一定义为BMD异常组。
1.2.3 血清25-(OH)D测定 收集所有儿童静脉血置于4℃环境下保存,并以3000 r/min离心10 min,离心半径为15 cm,分离得到血清,并检测25-(OH)D水平,检测方法为酶联免疫吸附法,操作按照试剂盒(北京博晖创新生物技术股份有限公司,生产批号:20160413)说明进行。维生素D评定标准[7]:血清25-(OH)D≥30 ng/mL定义为充足(充足组,n = 169),20 ng/mL≤25-(OH)D<30 ng/mL定义为不足(不足组,n = 253),10 ng/mL≤25-(OH)D<20 ng/mL定义为缺乏(缺乏組,n = 177),25-(OH)D<10 ng/mL定义为严重缺乏(严重缺乏组,n = 30)。
1.3 统计学方法
采用SPSS 22.0统计学软件进行数据分析,计量资料用均数±标准差(x±s)表示,两组间比较采用t检验;计数资料用率表示,组间比较采用χ2检验;采用Pearson积矩相关进行相关性分析;采用多因素Logistic回归分析学龄前儿童BMD异常的影响因素,以P < 0.05为差异有统计学意义。
2 结果
2.1 学龄前儿童BMD状况
629例儿童BMD SOS值平均(2986.34±329.70),Z值平均(-0.12±0.93),其中BMD正常492例,BMD异常137例,学龄前儿童BMD异常率为21.78%,不同年龄儿童BMD异常率情况见图1。
2.2 BMD正常组和异常组基线资料比较
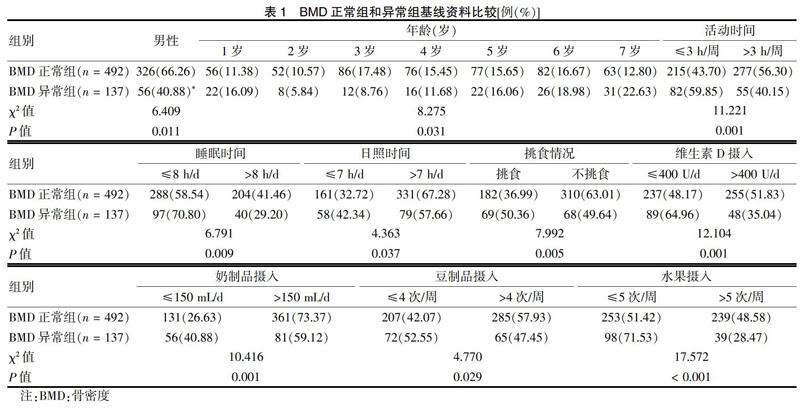
女童、1岁以及5~7岁儿童BMD异常率高于男童、2~4岁儿童(P < 0.05);活动时间≤3 h/周、睡眠时间≤8 h/d、日照时间≤7 h/d的学龄前儿童BMD异常率更高(P < 0.05);挑食、维生素D摄入≤400 U/d、奶制品摄入≤150 mL/d、豆制品摄入≤4次/周、水果摄入≤5次/周的学龄前儿童BMD异常率更高(P < 0.05)。见表1。
2.3 学龄前儿童BMD异常的多因素Logistic回归分析
以是否发生BMD异常为因变量,表1中差异有统计学意义的变量作为自变量,变量赋值见表2。多因素Logistic回归分析显示,与2岁儿童比较,1岁、5~7岁是BMD异常的独立危险因素,活动时间、睡眠时间、日照时间、挑食情况、维生素D摄入、奶制品摄入、豆制品摄入、水果摄入是学龄前儿童BMD异常的影响因素。见表3。
2.4 不同25-(OH)D水平儿童BMD比较
随着25-(OH)D水平的降低,SOS值逐渐增大,Z值逐渐减小,BMD异常率逐渐增加(P < 0.05)。见表4。
2.5 学龄前儿童BMD与血清25-(OH)D相关性分析
经Pearson积矩相关分析,学龄前儿童SOS与血清25-(OH)D呈负相关(r = -0.729,P < 0.05),Z值与血清25-(OH)D呈正相关(r = 0.761,P < 0.05)。
3 讨论
学龄前儿童处于生长发育关键时期,养不良以及骨骼发育迟滞不仅影响生长发育,也是造成儿童期骨质软化症、佝偻病的重要原因[8-10]。本研究中,629例学龄前儿童BMD异常率为21.78%,与西安[11]、广州[12]等地文献报道的结果相近,但是略高于苏州地区0~6岁儿童的11.90%[9],可能与不同地区日照时间长短密切相关。研究显示[13],日照时间长的地区儿童BMD异常率明显低于日照时间短的地区。研究[14]表明,1岁以内儿童钙元素的吸收来源主要依靠于食物中的营养物质、维生素D制剂或者钙剂的补充,并且1岁以内儿童日照时间以及活动时间相对较短,因此BMD异常率相对较高,本研究得到相似结果,即1岁以内儿童BMD异常率高于2~6岁儿童。本研究还发现,1岁以后儿童BMD异常率随着儿童年龄的增长,BMD异常率升高,7岁儿童BMD异常率高于1岁儿童,推测该趋势的发生原因,可能是因为1岁以后儿童口服维生素D制剂的配合程度较高,且这个年龄段儿童活动时间增加有关,但是随着年龄的增加,儿童逐渐开始挑食,补充维生素D的频率减少,且儿童进入幼儿园后减少了户外活动时间[15]。
女童BMD异常率高于男童,可能与女童相对比较文静,户外活动相对减少有关。1岁以及5~7岁儿童BMD异常率高于2~4岁儿童,可能是因为户外活动时间减少。此外,活动时间≤3 h/周、睡眠时间≤8 h/d、日照时间≤7 h/d的学龄前儿童BMD异常率较高,挑食、维生素D摄入≤40 U/d、奶制品摄入≤150 mL/d、豆制品摄入≤4次/周、水果摄入≤5次/周的学龄前儿童BMD异常率较高,活动时间、睡眠时间、日照时间、挑食情况、维生素D摄入、奶制品摄入、豆制品摄入、水果摄入可能是学龄前儿童BMD异常的影响因素,提示光照、睡眠、膳食营养均衡与儿童BMD密切相关。采用多因素Logistic回归分析校正混杂因素,1岁、5~7岁儿童是BMD异常的独立危险因素,可能与1岁儿童户外活动时间减少,维生素D及钙剂补充不足有关,而5~7岁儿童则是挑食、维生素D制剂和钙剂补充频率不高、室外活动减少等有关。活动时间少是儿童BMD异常危险因素,这与有关研究结果一致[16],即活动,尤其是阳光下活动可以使维生素D合成增加并加快钙、磷吸收,从而提高BMD水平。睡眠时间短也是儿童BMD异常的危险因素,可能是因为睡眠有助于机体分泌生长激素,睡眠不足影响生长激素的分泌,进而影响骨骼生长发育[17]。日照时间不足是BMD异常危险因素,这也与光照不足导致维生素D合成减少密切相关。研究表明[18],膳食均衡有助于兒童骨量的增加以及为能量储备提供物质基础,挑食或者饮食不均衡可能导致微量元素或者脂肪等的摄入不足,进而影响BMD。上述结果提示,密切监测学龄前儿童BMD,适时补充适量钙剂和维生素D,增加户外活动时间,保持良好的睡眠及合理营养膳食。
血清25-(OH)D是反映儿童营养状况的敏感指标,有研究表明[19],25-(OH)D水平与BMD呈正相关,25-(OH)D水平越高,BMD含量越丰富。但是,也有研究[4]认为BMD仅能反映维生素D不足时的维生素D水平。还有研究[20]发现25-(OH)D与BMD无明显关系。
综上所述,学龄前儿童BMD异常率较高,尤其是1岁和5~7岁儿童是高发人群,定期监测学龄前儿童BMD有重要意义,适量补充维生素D、钙剂,合理膳食、均衡营养、保证充足睡眠、加强户外活动是预防儿童BMD异常,确保骨骼正常生长发育的重要措施。
[参考文献]
[1] Smith GC,Stenhouse EJ,Crossley JA,et al. Early pregnancy levels of pregnancy-associated plasma protein a and the risk of intrauterine growth restriction,premature birth,preeclampsia,and stillbirth [J]. J Clin Endocrinol Metab,2002,87(4):1762-1767.
[2] Bujold E,Roberge S,Nicoladids KH. Low-dose aspirin for prevention of adverse outcomes related to abnormal placentation [J]. Prenat Diagn,2014,34(7):642-648.
[3] VanWijk MJ,Kublickiene K,Boer K,et al. Vascular function in preeclampsia [J]. Cardiovasc Res,2000,47(1):38-48.
[4] Monte S. Biochemical markers for prediction of preeclampsia:review of the literature [J]. J Prenatal Med,2011,5(3):69-77.
[5] Afrakhteh M,Moeini A,Taheri MS,et al. Uterine Doppler velocimetry of the uterine arteries in the second and third trimesters for the prediction of gestational outcome [J]. Rev Bras Ginecol Obstet,2014,36(1):35-39.
[6] Jamal A,Abbasalizadeh F,Vafaei H,et al. Multicenter screening for adverse pregnancy outcomes by uterine artery Doppler in the second and third trimester of pregnancy [J]. Med Ultrason,2013,15(2):95-100.
[7] Nicoladids KH. A model for a new pyramid of prenatal care based on the 11 to 13 weeks′ assessment [J]. Prenat Diagn,2011,31(1):3-6.
[8] Bujold E,Roberge S,Lacasse Y,et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy:a meta-analysis [J]. Obstet Gynecol,2010,116(2Pt1):402-414.
[9] Roberge S,Nicolaides KH,Demers S,et al. Prevention of perinatal death and adverse perinatal outcome using low dose aspirin:a meta-analysis[J]. Ultrasound Obstet Gynecol,2013,41(5):491-499.
[10] Roberge S,Nicolaides KH,Demers S,et al. The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction:systematic review and meta-analysis [J]. Am J Obstet Gynecol,2017,216(2):110-120.
[11] Kafkasl A,Turkcuoglu I,Turhan U. Maternal,fetal and perinatal characteristics of preeclampsia cases with and without abnormalities in uterine artery Doppler indexes [J]. J Matern Fetal Neonatal Med,2013,26(9):936-940.
[12] Madzli R,Yuksel MA,Imamoglu M,et al. Comparison of clinical and perinatal outcomes in early- and late-onset preeclampsia [J]. Arch Gynecol Obstet,2014,290(1):53-57.
[13] Martin AM,Bindra R,Curcio P,et al. Screening for pre‐eclampsia and fetal growth restriction by uterine artery Doppler at 11-14 weeks of gestation[J]. Ultrasound in Obstetrics and Gynecology,2001,18(6):4.
[14] Gómez O,Martínez JM,Figueras F,et al. Uterine artery Doppler at 11-14 weeks of gestation to screen for hypertensive disorders and associated complications in an unselected population [J]. Ultrasound Obstet Gynecol,2005, 26(5):490-494.
[15] Albaiges G,Missfelder-Lobos H,Lees C,et al. One-Stage Screening for Pregnancy Complications by Color Doppler Assessment of the Uterine Arteries at 23 Weeks? Gestation [J]. Obstet Gynecol,2000,96(4):559-564.
[16] Martin AM,Bindra R,Curcio P,et al. Screening for preeclampsia and fetal growth restriction by uterine artery Doppler at 11-14 weeks of gestation [J]. Ultrasound Obstet Gynecol,2001,18(6):4.
[17] Li N,Ghosh G,Gudmundsson S. Uterine artery Doppler in high-risk pregnancies at 23-24 gestational weeks is of value in predicting adverse outcome of pregnancy and selecting cases for more intense surveillance [J]. Acta Obstet Gynecol Scand,2014,93(12):1276-1281.
[18] Velauthar L,Plana MN,Kalidindi M,et al. First-trimester uterine artery Doppler and adverse pregnancy outcome:a meta-analysis involving 55,974 women [J]. Ultrasound Obstet Gynecol,2014,43(5):500-507.
[19] D′Silva A,Fyfe R,Hyett J. First trimester prediction and prevention of adverse pregnancy outcomes related to poor placentation [J]. Curr Opin Obstet Gynecol,2017,29:367-374.
[20] Hafner E,Metzenbauer M,Honfinger D,et al. Comparison between three-dimensional placental volume at 12 weeks and uterine artery impedance/notching at 22 weeks in screening for pregnancy-induced hypertension, pre-eclampsia and fetal growth restriction in a low-risk population [J]. Ultrasound Obstet Gynecol,2006,27(6):652-657.

