Nerve coblation for treatment of trigeminal neuralgia: A case report
Xiao-Hui Yang, Yan Li, Li-Qiang Yang, Bai-Shan Wu, Jia-Xiang Ni
Abstract
Key words: Nerve coblation; Trigeminal neuralgia; Gasserian ganglion; Computed tomography guided; Case report
INTRODUCTION
Trigeminal neuralgia (TN) is characterized by sudden, severe, brief, stabbing, and recurrent pain, with a reported incidence of about 13/100000 persons every year[1].The etiology of the disease remains unclear and its clinical management, comprising medicinal and surgical approaches, is similarly inadequate. Technological advancements have paved the way for the application of minimally invasive interventional therapy, such as the treatment of TN. Benefits of these moments include little trauma, quick recovery, and adequate pain control.
However, postoperative numbness or hypoesthesia is the most common complication after treatment using the invasive techniques[2]. We therefore explored the gasserian ganglion nerve coblation (NC) technique to treat a patient with TN in the Department of Pain Medicine, Xuanwu Hospital, Beijing, China.
CASE PRESENTATION
Chief complaints
A 58-year-old man presented with chronic right facial pain and was followed at our hospital for about eight years. The pain was described as paroxysmal puncture with no obvious cause, mostly located in the right zygomatic zone, upper alveolar region,and jaws. Moreover, the pain, with a VAS score of 7-8 points, continued for about five seconds during each attack and resolved without intervention.
History of present illness
Identifiable triggers for the pain included activities such as eating, talking, brushing of the teeth, washing the face, and touching. Initially, the patient was started on acupuncture therapy together with oral carbamazepine (100 mg, once per day but still complained of right facial pain.
Physical examination upon admission
On further examination, we found that there was a trigger point on the right side of the zygomatic zone. However, muscles involved in mastication and movement of the mouth were normal and their functions were not limited.
Imaging examinations
Furthermore, examination of the skull base using magnetic resonance angiography(MRA) returned normal results.
FINAL DIAGNOSIS
The treatment presented in this Case Report was undertaken after obtaining the relevant ethical approval by the institutional review board of Xuanwu Hospital.Additionally, we obtained a signed informed consent form from the patient towards publishing this case report.
TREATMENT
On November 23, 2017, the patient received gasserian ganglion NC of the right trigeminal nerve guided by computed tomography (CT) at the positron-emission tomography-CT room of Xuanwu Hospital. As there was no standardized technique procedure, we adopted the method of CT-guided percutaneous radiofrequency thermocoagulation[1].
Prior to the procedure, the CT examination room was disinfected and the patient placed in a supine position with his head overhanging on the CT scanner bed. Vital signs were monitored during the entire procedure. First, access to the gasserian ganglion was explored following the Hartel's anterior route. The target was confirmed by CT scan to find the foramen ovale and mark the best puncture path(Figures 1 and 2). The route from the puncture point to the target was measured as a predetermined distance to ensure that skeletal obstacles were circumvented. An intravenous drip of 5 μg of sufentanil was conducted to relieve pain before puncture.After sterilization, the insertion point was anesthetized with 2 mL of 1% lidocaine.Second, a 150 mm 18G puncture needle was inserted. The angle and depth of insertion of the needle to the foramen ovale followed the best puncture approach. While piercing the needle into the foramen ovale, a repeat CT scan was done to ascertain the position of the needle tip (Figures 3 and 4). Third, the needle core was pulled out, and the coblation wand was inserted into the introducer needle and extended approximately 5 mm beyond the introducer needle. Stimuplex HNS 11 Nerve Stimulator (B. Braun Co. Ltd, Melsungen, Germany) was then connected. Electrical stimulation was induced while observing the patient's response to the stimulation.This guided the adjustment of the positioning of the wand until the target was accessed. Fourth, intravenous anesthesia comprising propofol (1-2 mg/kg)supplemented with facemask oxygen was administered after certifying the proper location. No tracheal intubation was performed. The coblation wand was changed to connect with a low temperature plasma multi-function operating system SM-D380C(GaoTon Co. Ltd, Xi'an, China). Fifth, the target nerve was ablated by the coblation wand using the following settings: ablation intensity at mode 2 and operation temperature at 40 to 50 °C. Ablation cycle lasted approximately 30 s. Thereafter, the coblation wand was retracted to 3 mm. Finally, the wand and puncture needle were pulled out. After the procedure, dressing was applied to the patient who, after regaining consciousness, was returned to the ward and instructed to rest for 24 h.
OUTCOME AND FOLLOW-UP
The patient was followed for 3 d after the surgery. On examination, the right zygomatic, alveolar, submandibular, and cheek pain had disappeared completely with a VAS score of 0. The right zygomatic and alveolar regions manifested some mild numbness (level II). During follow-ups at 1, 2, 3, and 6 mo after surgery, the VAS score for pain was 0 and the numbness score was level I. The patient reported no other adverse effects during the follow-up examinations.
DISCUSSION
Early TN treatment is dominated by the use of drugs with carbamazepine as the drug of choice achieved pain control in 70% to 98% of patients[3,4]. With progression of the disease, carbamazepine, even at high doses, becomes ineffective in alleviating pain. In fact, higher doses of the drug can cause side effects, such as dizziness, drowsiness,fatigue, nausea, rashes, vomiting, occasional granulocytopenia, reversible thrombocytopenia, and even aplastic anemia and toxic hepatitis. Many patients,therefore, cannot tolerate high dose medication[5,6].
Surgical intervention becomes an alternative to treat TN when drug therapy fails.Presently, surgical methods are mainly divided into minimally invasive intervention and open surgery. The former includes the radiofrequency thermal coagulation of the trigeminal nerve[7], glycerol neurolysis[8], and percutaneous ganglion balloon compression[9]. On the other hand, open surgery includes trigeminal nerve root microvascular decompression[10], posterior root amputation of trigeminal nerve, and spinal cord amputation. A notable disadvantage of open surgery is that it requires craniotomy under general anesthesia, which may cause significant trauma. Greater risks and, in some cases, higher mortality rate have been associated with open surgery[10,11]. Minimally invasive interventional therapy has therefore become a preferred approach in the treatment of TN since it elicits little trauma, allows for quick recovery, and achieves effective relief of pain .

Figure 1 Accessing the gasserian ganglion according to the Hartel anterior route.
The case reported here was characterized by typical symptoms leading to a clear diagnosis of TN. The latest NC technology guided by CT was employed. The patient did not report feeling any pain three days after the surgery; a VAS score of 0 was recorded. The same results were observed at 1, 2, 3, and 6 mo after the surgery. From the foregoing observation, the pain-relieving effect of CT-guided NC is significantly distinct, and consistent with that reported for radiofrequency thermal coagulation in treating TN[12]. We are conscious, however, that there is need to observe the long-term effects of this procedure on pain relief and numbness. From a mechanistic point of view, NC does not rely on thermal effect as does radiofrequency thermal coagulation[13,14]. However, with 100-500 kHz and special bipolar radiofrequency electric field segment, the high-frequency oscillating tip locally generates a lowtemperature plasma layer. The activated ionic layer can break down the molecular bonds (layer thick 1 mm[15]), cut or ablate the nerve tissue, cause it to decompose and vaporize and drain out of the body from the puncture channel, block the pain signal transduction, and do not produce numbness at the same time. The patient had mild numbness 3 d after surgery, which was scored as level II. At 1, 2, 3, and 6 mo after surgery, numbness disappeared completely and was scored as level I. Postoperative numbness scores were significantly lower than those for the other case reported[2].Based on the techniques, it may be that the fine fibers (Aδ and C fibers), which transmit temperature sensation and pain, are damaged when ablating nerve tissue.However, there is little damage to the crude fibers (Aα and Aβ fibers) that transmit the sense of touch. Therefore, the incidence of postoperative numbness is low.
As an emerging technology, NC for the treatment of TN has not been extensively explored globally. This is a very promising minimally invasive interventional technique that holds multiple benefits to the patient not least because of effective pain control. A larger patient sample and longer follow-up period are warranted to ascertain the effectiveness of NC in the management of TN.
CONCLUSION
We conclude that CT-guided gasserian ganglion NC is a promising, effective treatment for TN and associated with minimal or non-postoperative numbness or hypoesthesia.
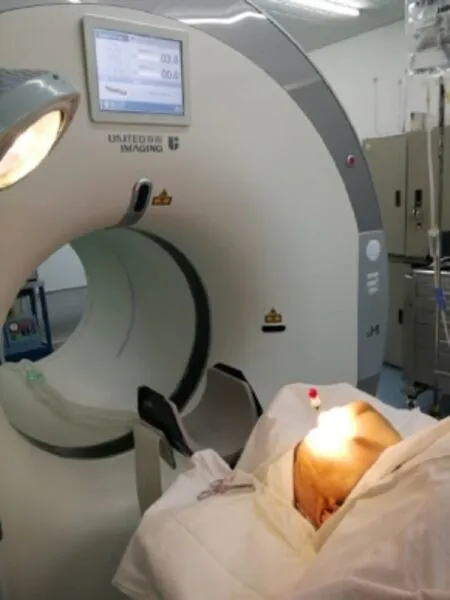
Figure 2 Target confirmation by a computed tomographic scan.
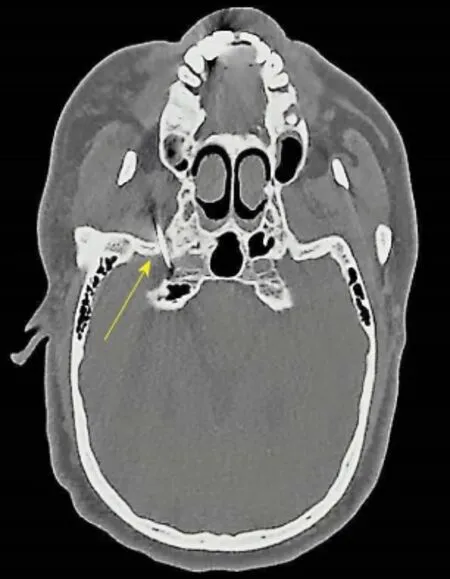
Figure 3 Computed tomographic image showing the introducer needle and coblation wand (yellow arrow). The coblation wand extended approximately 5 mm beyond the introducer needle.

Figure 4 Computed tomographic three-dimensional skull reconstruction image showing the introducer needle and coblation wand (yellow arrow), which pierced the needle into the foramen ovale and reached the target nerve.
 World Journal of Clinical Cases2019年9期
World Journal of Clinical Cases2019年9期
- World Journal of Clinical Cases的其它文章
- Coexistence of breakpoint cluster region-Abelson1 rearrangement and Janus kinase 2 V617F mutation in chronic myeloid leukemia: A case report
- Crizotinib-induced acute fatal liver failure in an Asian ALK-positive lung adenocarcinoma patient with liver metastasis: A case report
- Rare variant of pancreaticobiliary maljunction associated with pancreas divisum in a child diagnosed and treated by endoscopic retrograde cholangiopancreatography: A case report
- Adult-onset mitochondrial encephalopathy in association with the MT-ND3 T10158C mutation exhibits unique characteristics: A case report
- Management of the late effects of disconnected pancreatic duct syndrome: A case report
- Sofosbuvir/Ribavirin therapy for patients experiencing failure of ombitasvir/paritaprevir/ritonavir + ribavirin therapy: Two cases report and review of literature
