Causes associated with recurrent choledocholithiasis following therapeutic endoscopic retrograde cholangiopancreatography: A large sample sized retrospective study
Feng Deng, Mi Zhou, Ping-Ping Liu, Jun-Bo Hong, Guo-Hua Li, Xiao-Jiang Zhou, You-Xiang Chen
Abstract
Key words: Choledocholithiasis; Endoscopic retrograde cholangiopancreatography;Recurrence; Common bile duct
INTRODUCTION
Due to its minimal trauma and high safety, endoscopic retrograde cholangiopancreatography (ERCP) has become one of the most important methods for the clinical diagnosis and treatment of choledocholithiasis. Currently, ERCP technology is very advanced, but the recurrence of choledocholithiasis after ERCP is still a challenging problem. Follow-up studies have shown that the incidence of choledocholithiasis recurrence after endoscopic treatment is 2%-22%[1-5]. Many studies have reported that choledocholithiasis is associated with bacterial infection, an abnormal biliary structure, inflammation, endoscopic and surgical treatment, and other factors[1-3,6-8]. However, risk factors for the recurrence of choledocholithiasis have not been thoroughly defined, and the risk factors identified are different across studies. This study aimed to explore the independent risk factors for stone recurrence by comprehensively analyzing the relevant factors for stone recurrence in a largesized sample.
MATERIALS AND METHODS
Patients
From January 2007 to January 2016, we retrospectively reviewed cases from a welldesigned ERCP database at the First Affiliated Hospital of Nanchang University. The follow-up period was from the date of the initial removal of choledocholithiasis to the date of the visit to the hospital for choledocholithiasis recurrence or more than one year for the control group. The patients with the symptoms of fever, abdominal pain,jaundice, or other typical symptoms who revisited our hospital underwent abdominal computed tomography (CT) and ERCP to confirm choledocholithiasis. The patients who underwent choledocholithiasis removal by ERCP and were confirmed to have had their stones completely removed were enrolled. The exclusion criteria were as follows: (1) History of previous ERCP; (2) Patients with tumors of the liver,gallbladder, common bile duct (CBD), or duodenal papilla; (3) Patients were confirmed not to have had their stones completely removed after first choledocholithiasis removal by ERCP; and (4) Patients with incomplete clinical data. The study was approved by the institutional review board of the First Affiliated Hospital of Nanchang University (No. 2017-040).
Outcome measurements
The primary outcomes were risk factor s for recurrence of choledocholithiasis.Choledocholithiasis recurrence was defined as recurrence of symptoms of fever,abdominal pain, jaundice, or other typical symptoms, and choledocholithiasis was confirmed by abdominal B-scan ultrasonography, CT, or magnetic resonance cholangiopancreatography 6 mo after the stones were completely removed. The patients were classified into two groups: Recurrence and control groups. The following clinical data were recorded: (1) General characteristics, including sex, age,time from disease onset to stone removal, and history of drinking and smoking; (2)Past medical history, including history of hypertension, diabetes, hepatitis B, fatty liver, cirrhosis, cholecystectomy, biliary-enteric anastomosis, choledocholithotomy, or Billroth II gastrectomy; (3) ERCP-related factors, including endoscopic mechanical lithotripsy (EML), endoscopic papillary balloon dilation (EPBD), endoscopic sphincterotomy (EST), CBD stent implantation, endoscopic nasobiliary drainage, and the number of ERCP procedures; (4) CBD-related factors, including the presence of a combined biliary tract infection, gallstones, stones in the intrahepatic bile duct, a bile duct-duodenal fistula, CBD stenosis, duodenal ulcers, periampullary diverticula(PAD) or ectopic duodenal papilla, duodenal papilla shape, bile duct angle referring to the angle between the horizontal part of the CBD and a horizontal line[9], common bile diameter, CBD diameter, and the number of stones; and (5) Laboratory indicators and treatment, including total bilirubin, direct bilirubin, alanine aminotransferase,aspartate aminotransferase, gamma-glutamyl transferase, gallbladder parameters,triglycerides, and the use of preoperative antibiotics.
Statistical analysis
Continuous variables are reported as the mean and standard deviation (SD), and categorical variables are reported as absolute numbers and percentages. Variables found to be statistically significant in the univariate logistic regression analysis were introduced into a multivariate logistic analytic model (stepwise regression) to identify independent risk factors with odds ratios (ORs) and 95% confidence intervals (CIs). AP-value < 0.05 was considered statistically significant. Data were analyzed using SPSS software (v17.0; SPSS Inc., Chicago, IL, United States).
RESULTS
General characteristics
From January 2007 to January 2016, 477 patients revisited the hospital for their choledocholithiasis recurrence. Among these patients, the second and several instance(≥ 3 times) recurrence rates were 19.5% (93/477) and 44.07% (41/477), respectively.The average number of instances of stone recurrence was 1.45, and the average time to first stone recurrence was 21.65 mo. A 1:1 case-control study was used for this investigation, and the controls were 477 patients without choledocholithiasis recurrence after ERCP in more than one year of follow-up. The average age of all patients was 57.43 ± 14.92 years, and the study included 445 males (46.65%) and 509 females (53.35%). There were more patients > 65 years old in the recurrence group than in the control group (OR = 2.437, 95%CI: 1.818-3.266;P =0.000). No statistically significant differences between the two groups were observed in terms of sex, weight,time from the onset of stone removal to recurrence, or history of drinking or smoking(Table 1).
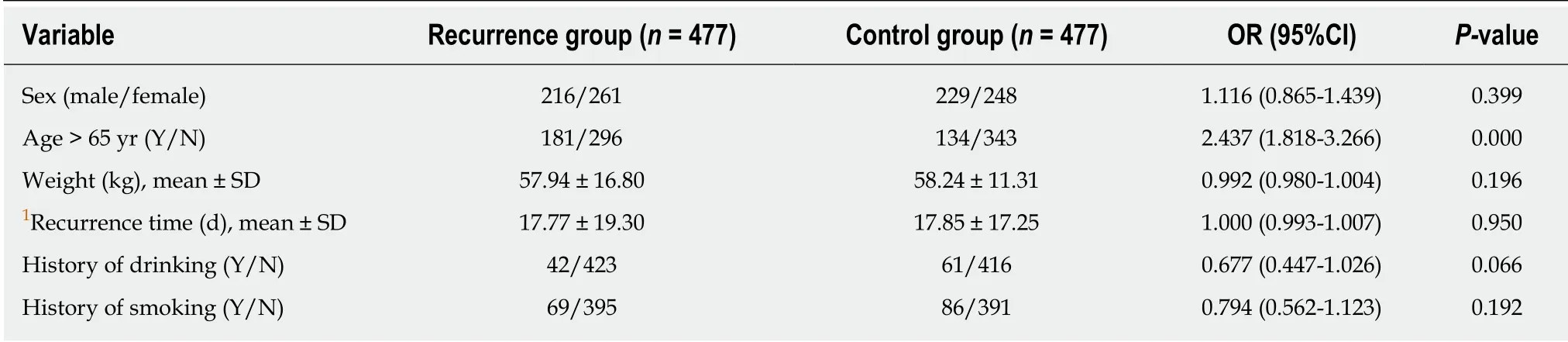
Table 1 General characteristics compared between the recurrence group and control group
Univariate analysis
On univariate analysis, significant differences were noted between the two groups in terms of medical history: A medical history of cholecystectomy (OR = 1.4, 95%CI:1.085-1.806;P =0.01) and choledocholithotomy (OR = 3.255, 95%CI: 2.114-5.01;P =0.000) (Table 2). Moreover, significant differences in ERCP-related factors were observed: ERCP with EML (OR = 2.068, 95%CI: 1.375-3.11;P =0.000), EPBD (OR =5.669, 95%CI: 3.594-8.941;P =0.000), EST (OR = 1.701, 95%CI: 1.197-2.417;P =0.003),CBD stent implantation (OR = 3.737, 95%CI: 2.587-5.398;P =0.000), and multiple ERCP procedures (OR = 3.043, 95%CI: 2.242-4.13;P =0.000) (Table 3). CBD-related factors, such as complications including biliary tract infections (OR = 1.034, 95%CI:1.007-1.061;P =0.014), stones in the intrahepatic bile duct (OR = 2.687, 95%CI: 1.919-3.762;P =0.000), PAD (OR = 1.607, 95%CI: 1.227-2.105;P =0.001), bile-duct duodenal fistula (OR = 2.324, 95%CI: 1.088-4.964;P <0.05), CBD stenosis (OR = 1.661, 95%CI:1.051-2.626;P <0.05), CBD diameter (OR = 1.988, 95%CI: 1.589-2.486;P =0.000), and choledocholithiasis diameter ≥ 10 mm (OR = 1.580, 95%CI: 1.202-2.067;P =0.001) also showed significant differences between the two groups (Table 4). Additionally,compared with patients in the control group, patients in the recurrence group used fewer antibiotics before ERCP (OR = 0.523, 95%CI: 0.385-0.711;P =0.000) (Table 5).
Multivariate analysis
Multivariate stepwise logistic regression analysis showed that age > 65 years (OR =1.556, 95%CI: 1.079-2.244;P =0.018), history of choledocholithotomy (OR = 2.474,95%CI: 1.417-4.320;P =0.001), EPBD (OR = 5.545, 95%CI: 3.026-10.162;P =0.000), EST(OR = 3.378, 95%CI: 1.968-5.797;P =0.000), CBD stent implantation (OR = 5.562,95%CI: 3.326-9.301;P =0.000), multiple ERCP procedures (OR = 3.601, 95%CI: 1.778-3.805;P =0.000), stones in the intrahepatic bile duct (OR = 2.359, 95%CI: 1.516-3.668;P=0.000), PAD (OR = 1.579, 95%CI: 1.090-2.289;P =0.016), choledocholithiasis diameter ≥ 10 mm (OR = 1.599, 95%CI: 1.117-2.290;P =0.010), biliary-duodenal fistula(OR = 2.720, 95%CI: 1.094-6.765;P =0.031), no use of preoperative antibiotics (OR =0.527, 95%CI: 0.346-0.801;P =0.003), and biliary tract infections (OR = 1.059, 95%CI:1.021-1.099;P =0.003) were independent risk factors for the recurrence of choledocholithiasis after ERCP (Table 6). A Kaplan-Meier analysis showed that as age increased, the rate of choledocholithiasis recurrence increased proportionally (Figure 1).
DISCUSSION
The recurrence rate of choledocholithiasis after ERCP is reported to be 2%-22%[1-5]. In our studies, once choledocholithiasis recurred, the next recurrence rate increased in proportion to the number of instances of recurrence, as reported previously[1,10].Several risk factors have been reported in various studies[1-3,6-8]. This study showed that age > 65 years, history of choledocholithotomy, EPBD, EST, CBD stent implantation,multiple ERCP procedures (≥ 2), stones in the intrahepatic bile duct, PAD,choledocholithiasis diameter ≥ 10 mm, bile duct-duodenal fistula, biliary tract infection, and no preoperative antibiotic use were independent risk factors for the recurrence of choledocholithiasis after ERCP.
It has been reported that the recurrence rate of choledocholithiasis in elderly patients (age > 65 years) can be as high as 30%[11]. The specific mechanism is unclear,but Keizmanet al[4]believe that elderly patients have more risk factors for the recurrence of stones, such as CBD dilatation, CBD angulation, and PAD, which are related to the recurrence of stones. PAD is rare in patients younger than 40 years ofage. It is found more often in older patients, and the occurrence of PAD increases with increasing age.

Table 2 Past medical history compared between the recurrence group and control group
The surgical removal of choledocholithiasis, whether open or laparoscopic, is seldom performed and is usually reserved for patients in whom ERCP has failed[12].Laparoscopic CBD exploration is considered in patients with larger stones in whom ERCP has failed. Stone recurrence caused by a history of choledocholithotomy may be due to long-term compression of the biliary tract by the T-tube placed during the choledocholithotomy leading to necrosis and scarring of the epithelial cells of the biliary tract, which easily cause biliary tract stenosis and disorders of biliary excretion[13].
Under physiological conditions, the sphincter of Oddi functions as a “switch” that controls the excretion of pancreatic juice and bile and prevents the reflux of intestinal fluid. Intraoperative ERCP surgeries, such as EPBD, EST, and multiple ERCP procedures, can cause dysfunction of the sphincter of Oddi, which cannot be restored within a short period of time. Then, the barrier against intestinal fluid reflux weakens or disappears, and intestinal fluid can reflux into the bile duct. Because intestinal fluid contains a large amount of bacteria, digestive juices, and food residues, when it refluxes into the bile duct, it changes the bile duct loop and leads to bile duct infection[14]; the colonized bacteria produce β-glucuronic acid, which is associated with the formation of bilirubin calcium stones[5,6,15,16], thus promoting the recurrence of stones. Because bacterial contamination of the bile duct is a common finding in patients with choledocholithiasis, incomplete duct clearance may put patients at risk of cholangitis. Therefore, it is important for endoscopists to ensure that adequate biliary drainage is achieved in patients with choledocholithiasis that cannot be retrieved[17]. However, stents have been placed for long periods of time, leading to bile salt deposition and adherence to the stents. The stents can be a nidus for CBD stones.Bile duct stent placement affects biliary tract dynamics, predisposing the patient to cholestasis. On the one hand, siltation of bile is conducive to bacterial reproduction.On the other hand, concentration of bile stimulates inflammatory changes in the bile duct mucosa, resulting in the precipitation of bile bacteria, shedding cells, and inflammatory cells, which promote the recurrence of stones[18].
PAD form adjacent to the biliary and pancreatic duct confluence. When a diverticulum is large, it can directly compress the CBD, resulting in poor bile excretion. When a diverticulum is complicated by duodenal dysfunction, the food and refluxed intestinal fluid can remain in the diverticulum, stimulating long-term inflammation of the sphincter of Oddi, leading to dysfunction, duodenal papillary stenosis, and cholestasis[19]. PAD promotes the multiplication of beta-glucuronidaseproducing bacteria, leading to earlier binding of dissociated glucuronide to bilirubin salts and promoting the pigmentation and formation of stones[20,21]. Larger stones often require lithotripsy, which may increase the risk of postoperative recurrence of stones.Larger stones cause greater forced expansion of the bile ducts and induce impaired function of normal bile ducts, leading to difficulties in bile excretion, which can easily cause cholestasis and bacterial infections[22,23]. Biliary tract infections mainly result from preoperative infections and retrograde reflux of intestinal fluid caused by reduced biliary pressure after cholecystectomy. Studies have shown that more than 94.6% of patients with pigmentary stones have positive bacterial cultures in their bile samples[24]. A variety of causes, such as abnormal biliary anatomy, PAD, abnormal biliary secretion, and biochemistry, can contribute to biliary tract infections. Bile duct bacteria is present, and the resulting beta-glucuronidase causes bilirubin hydrolysis to nonconjugated bilirubin, which can easily combine with calcium to form bilirubincalcium and promote gallstone formation[6,25-29]. The lack of preoperative use of antibiotics may increase the risk of biliary tract infections and promote the recurrence of stones. The presence of a biliary-duodenal fistula is a risk factor for the recurrence of choledocholithiasis. No relevant literature has been reported. Bile duct-duodenal fistulas often exist for a long time, and the refluxed intestinal fluid irritates the biliary mucosa, eventually leading to chronic inflammation.
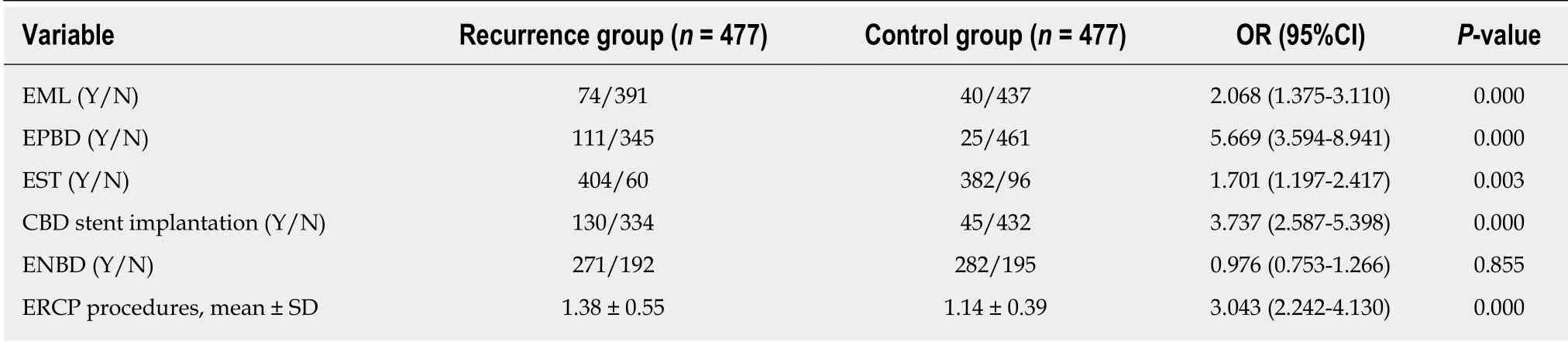
Table 3 Endoscopic retrograde cholangiopancreatography-related factors compared between the recurrence group and control group
This study was a single-center retrospective study. Although the clinical data of the patients were comprehensively analyzed and the risk factors for recurrence of choledocholithiasis after ERCP were studied in all aspects, there were still limitations to this retrospective study. This study did not further analyze the accuracy of individual risk factors for predicting the recurrence of choledocholithiasis. In conclusion, patient age greater than 65 years is an independent risk factor for the development of recurrent choledocholithiasis following ERCP, as is history of biliary surgeries, measures during ERCP, and prevention of postoperative complications.
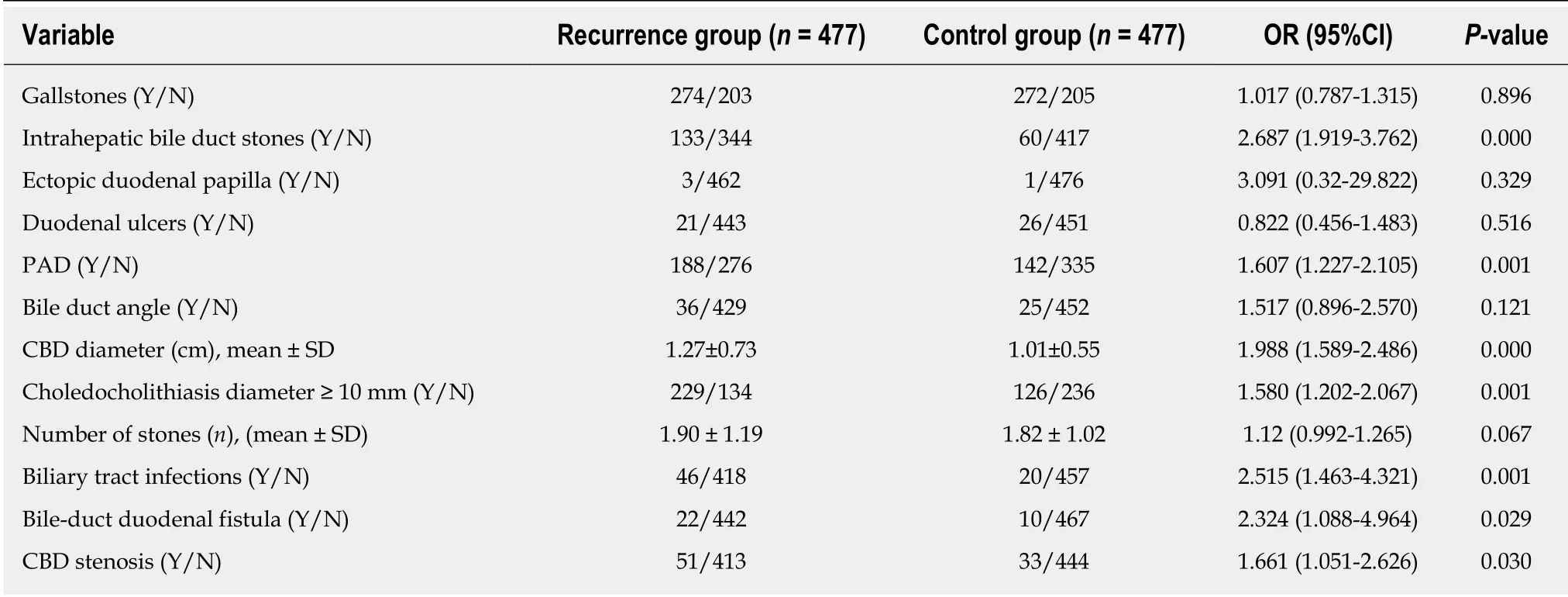
Table 4 Common bile duct-related factors compared between the recurrence group and control group
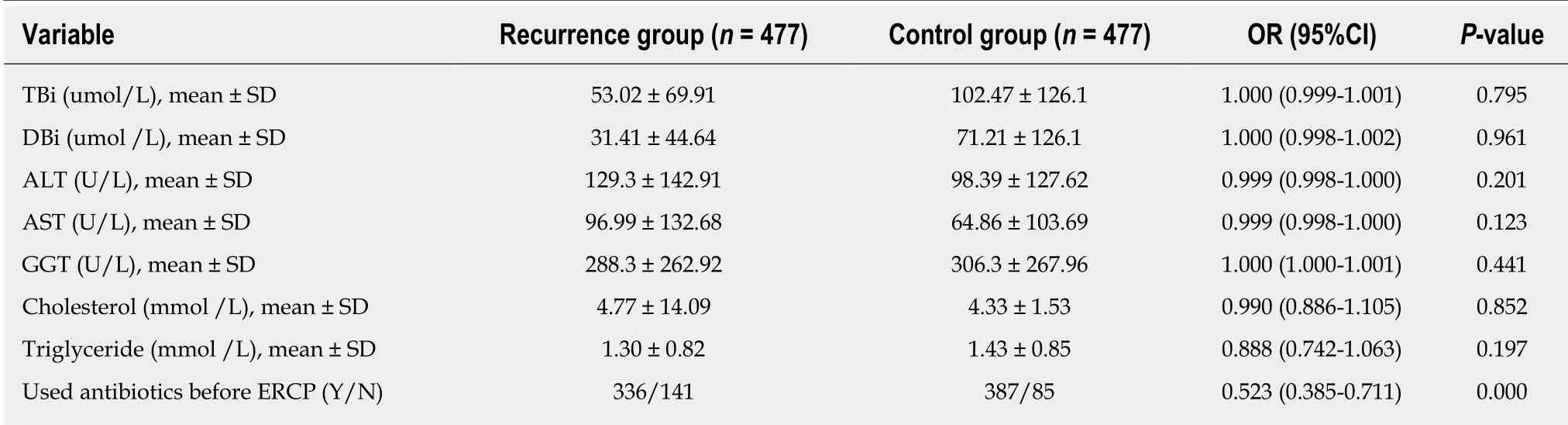
Table 5 Laboratory indicators and treatment compared between the recurrence group and control group

Table 6 Multivariate stepwise logistic regression analysis for the recurrence of choledocholithiasis

Figure 1 Kaplan-Meier curves showing the recurrence rate of CBD stones according to age (< 50 years, blue line; 50-59 years, green line; 60-69 years,yellow line; ≥ 70 years, red line) (log-rank P < 0.0001).
ARTICLE HIGHLIGHTS
Research background
Currently, endoscopic retrograde cholangiopancreatography (ERCP) technology is very advanced, but the recurrence of choledocholithiasis after ERCP is still a challenging problem.The potential causes of the recurrence of choledocholithiasis after ERCP are unclear.
Research motivation
To explore the independent risk factors for stone recurrence by comprehensively analyzing the relevant factors for stone recurrence in a large-sized sample.
Research objectives
The study aimed to analyze the potential causes of the recurrence of choledocholithiasis after ERCP.
Research methods
The ERCP database of our medical center was retrospectively reviewed, and information regarding eligible patients was collected. A 1:1 case-control study was used for this investigation.Data were analyzed by univariate and multivariate logistic regression and Kaplan-Meier analyses.
Research results
Multivariate logistic regression analysis showed that age > 65 years, combined history of choledocholithotomy, endoscopic papillary balloon dilation, endoscopic sphincterotomy,common bile duct stent implantation, multiple ERCP procedures (≥2), stones in the intrahepatic bile duct, periampullary diverticula, choledocholithiasis diameter ≥ 10 mm, bile duct-duodenal fistula, combined biliary tract infections, and no preoperative antibiotic use were independent risk factors for the recurrence of choledocholithiasis after ERCP.
Research conclusions
In this large sample sized retrospective study, we concluded that patient age greater than 65 years is an independent risk factor for the development of recurrent choledocholithiasis following ERCP, as is history of biliary surgeries, measures during ERCP, and prevention of postoperative complications.
Research perspectives
The pathogenesis of recurrence of choledocholithiasis should be studied in future, as well as the prevention and treatment.
 World Journal of Clinical Cases2019年9期
World Journal of Clinical Cases2019年9期
- World Journal of Clinical Cases的其它文章
- Coexistence of breakpoint cluster region-Abelson1 rearrangement and Janus kinase 2 V617F mutation in chronic myeloid leukemia: A case report
- Crizotinib-induced acute fatal liver failure in an Asian ALK-positive lung adenocarcinoma patient with liver metastasis: A case report
- Rare variant of pancreaticobiliary maljunction associated with pancreas divisum in a child diagnosed and treated by endoscopic retrograde cholangiopancreatography: A case report
- Adult-onset mitochondrial encephalopathy in association with the MT-ND3 T10158C mutation exhibits unique characteristics: A case report
- Nerve coblation for treatment of trigeminal neuralgia: A case report
- Management of the late effects of disconnected pancreatic duct syndrome: A case report
