Gastrointestinal infection-related disseminated intravascular coagulation mimicking Shiga toxin-mediated hemolytic uremic syndrome - implications of classical clinical indexes in making the diagnosis:A case report and literature review
Xiang-Yang Li,Yan-Fen Mai,Jing Huang,Pearl Pai
Abstract
Key words: Thrombotic microangiopathy;Thrombotic thrombocytopenic purpura;Hemolytic uremic syndrome;Schistocyte;Lactate dehydrogenase;Thrombocytopenia;Case report
INTRODUCTION
The term Thrombotic Microangiopathy (TMA) was first proposed by Symmers in 1952 to describe generalized microvascular thrombi in thrombotic thrombocytopenia purpura (TTP)[1].In 1955,Gasser first documented similar pathological changes in the kidneys in hemolytic uremic syndrome (HUS)[2].TMA was synonymous with microangiopathic hemolytic anemia (MAHA) in that mechanical fragmentation of erythrocytes occurred as they passed through the thrombotic meshwork and strictured microvasculature[1].MAHA diagnosis relies on the presence of peripheral schistocytes,elevated serum lactate dehydrogenase (LDH)[3],along with other markers of hemolysis (e.g.,indirect bilirubin and haptoglobins)[3,4].Nowadays,TMA is used to describe histological abnormalities of arterioles and capillaries characterized by thrombosis with endothelial impairment and mural damage[3,5].The clinical hallmarks of TMA include consumptive thrombocytopenia and MAHA with varying degrees of ischemic injury and organ dysfunction[3,5].The prototypes of TMA are TTP and HUS.Low platelet (PLT) counts makes disseminated intravascular coagulation(DIC) disorder part of a differential diagnosis.TMA may be induced by several disorders or medical conditions,such as DIC[6],systemic infection and sepsis,systemic rheumatological diseases (e.g.,systemic lupus erythematosus,small vessel vasculitis,and antiphospholipid syndrome),malignancies,pregnancy,malignant hypertension,coagulopathy,and may follow solid organ or hematopoietic stem cell transplantation and drug therapy[4].
Both TMA and DIC related disorders are a matter of clinical emergency.Hence,timely diagnosis and early initiation of targeted therapy is essential for the survival of patients and the affected organs[7].However,the complexity of pathological pathways and clinical overlaps of TMA prototypes create diagnostic uncertainties.In practice,physicians rely on clinical phenotype and biomarkers to diagnose TMA and its underlying conditions.However,these markers are limited by specificity or sensitivity and need to be interpreted carefully.Herein,we report a case of infectionrelated DIC in a woman who presented with diarrhea,thrombocytopenia,elevated LDH,schistocytes and acute kidney injury,mimicking Shiga toxin-HUS (ST-HUS).In this report,we review and discuss the utility and drawbacks of several classical clinical indexes used in the discrimination of TTP-HUS and DIC.
CASE PRESENTATION
Chief complaints
Vomiting,diarrhea and abdominal pain for 2 h.
History of present illness
A previously healthy 44-year-old female presented to the Accident and Emergency Department with a 2 h duration of diarrhea,vomiting,painful lower abdominal cramping and dizziness.The woman was working as a cleaner.According to the patient,she had eaten an unpeeled apple a few hours before.The diarrhea was described as watery but non-bloody.There was no chill,rigor or fever.
Personal and family history
The patient denied any significant past medical history and had no recent travel.She denied exposure to any animals or consumption of any under-cooked vegetables or meats.There was no significant family history.She reported no pregnancy related disorders or history of drug allergy.
Physical examination upon admission
The patient was fully oriented at presentation with a temperature of 37.1°C.There was no rash.Her respiratory rate was 23 breaths per minute and oxygen saturation was 98% on air.Her pulse was 48 beats per minute;her lying blood pressure was 69/41 mmHg.Her lungs were clear.There was no heart murmur.The abdomen showed only mild epigastric tenderness.There were no masses or hepatosplenomegaly.There were no abnormal neurology signs.
Laboratory examinations
Her initial blood tests at the Emergency Department showed a white blood cell (WBC)of 2.67 × 109/L (normal 4 × 109/L - 10 × 109/L);neutrophils,73.4%;lymphocytes,26.6%;hemoglobin (HB),134 g/L (normal 115-150 g/L);PLT count 31 × 109/L(normal 150 × 109/ L - 350 × 109/L) (Table 1).The serum creatinine was 74.5 μmol/L(normal 46-92 μmol/L);blood urea nitrogen (BUN),5.6 mmol/L (normal 2.5-6.1 mol/L);serum amylase,74 U/L (normal 30-110 U/L);total bilirubin,50.9 μmol/L(normal 3-22 μmol/L),indirect bilirubin,47.3 μmol/L (normal 0-19 μmol/L).The coagulation test showed normal prothrombin time (PT) of 12.9 s (normal 11-14.5 s;international normalized ratio (INR),1.0 (normal 0.8-1.2);activated partial thromboplastin time (APTT) was 34.9 s (normal 26-40 s);fibrinogen (Fib),2.53 g/L (2-4 g/L);thrombin time (TT),17.8 s (14-21 s) (Table 2,Figure 1).She was given oxygen,and intravenous 0.9% saline and dopamine were commenced at 10 μg per kg of body weight per minute.Her blood pressure rose to 97/58 mmHg after an hour.She was transferred to the Department of gastrointestinal disease with a primary diagnosis of acute gastroenteritis and early shock.The thrombocytopenia was thought to be related to severe infection.
Following admission,she was given 2.0 g intravenous ceftriaxone and fluid.The next day,her abdominal pain and the watery diarrhea had decreased.A repeat blood routine test showed:WBC,23.52 × 109/L;neutrophils,98%;lymphocytes,1.1%;eosinophils,0%;monocytes,0.9%;HB,120 g/L;PLT,20 × 109/L (Table 1).Urinalysis showed protein 1+,WBC 86/μL (normal,0-23/μL),red blood cell (RBC) 96/μL(normal,0-18/μL) (Table 3).The stool microscopy and culture and occult blood tests were negative.Repeat clotting study showed a prolonged PT of 19.2 s;INR,1.64;APTT,53.9 s;and Fib lowered to 1.51 g/L;TT to 25 s (Table 2,Figure 1).The Creactive protein was 55.13 g/L (normal < 10 mg/L);serum procalcitonin (PCT),73 ng/mL (normal < 0.05-0.1 ng/mL);amylase,92 U/L;lipase,77 U/L;alanine aminotransferase,38 IU/L (normal 9-52 IU/L);aspartate aminotransferase,54(normal 14-36 IU/L).The stool rotavirus antigen andClostridium difficiletoxin A/B tests were negative (Table 4).Despite a 24-h urine volume of two liters,her serum creatinine levels had increased to 145 μmol/L.
Intravenous ceftriaxone was continued at a dose of 2.0 g daily.On day 3,the diarrhea had reduced to four or five times per day.Total 24-h urine output was 1 L.The creatinine levels further increased to 215.7 μmol/L (Figure 2),BUN to 6.7 mmol/L.The peripheral blood count showed WBC,14.59-13.81 × 109/L;neutrophils 0.88-89;PLT,15 × 109/L.Peripheral blood smear showed a schistocyte count of 0.6%;serum LDH level was 1818 U/L (normal 313-618 U/L) (Figure 2).The clotting profile had improved:PT,15.4 s;INR 1.25;APTT,45.6 s;Fib 3.19 g/L;TT 16.3 s.D-dimer level > 20 mg/L (normal 0-0.5 mg/L) (Table 2).Plasma troponin I level was 0.082 ng/mL (normal 0-0.034 ng/mL);serum ferritin,1417.3 ng/mL (normal 11-306.8 ng/mL);PCT,40.3 ng/mL.Two stool cultures (taken on day 2 and 3) were negative forEscherichia coliO157:H7,Shigella,Salmonella,Vibrio,Aeromonas,Plesiomonas or Campylobacter.Two blood and urine cultures (taken on day 2 and 3) were negative for bacteria and fungus (Table 4).
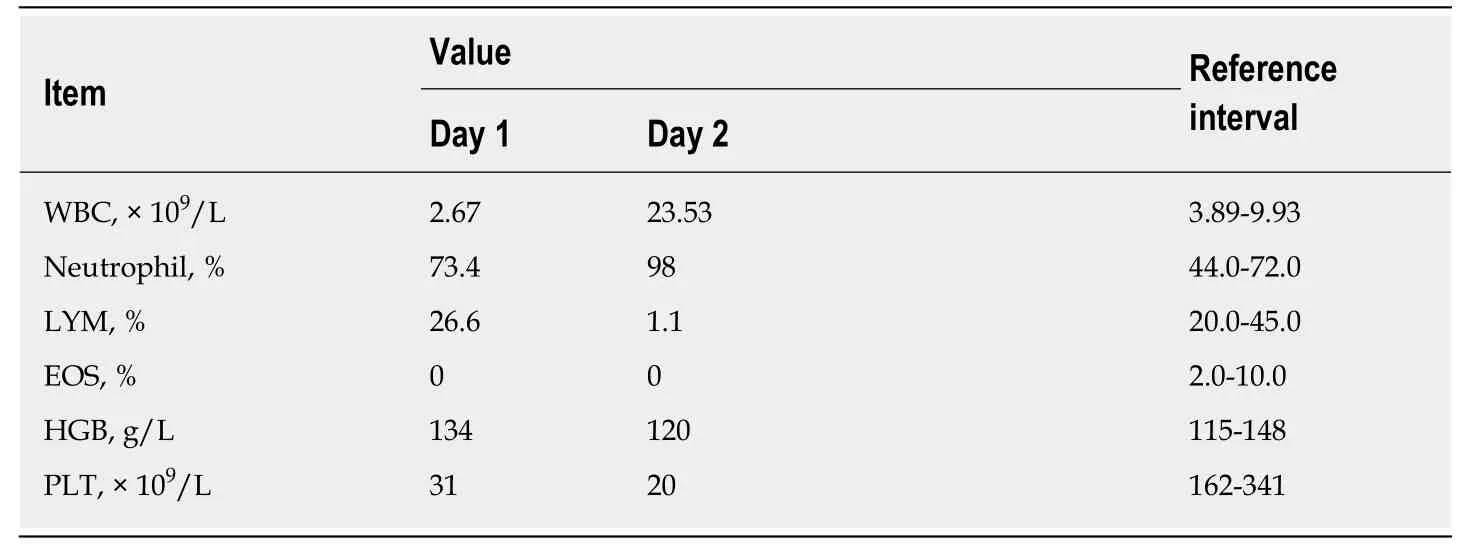
Table1 Complete blood cell counts on days 1 and 2
Imaging examinations
Ultrasonography of the urinary system on day 2 revealed symmetrical bilateral kidneys with increased parenchymal echogenicity and a low echogenic area of 57 mm by 21 in the lower right kidney,suggestive of effusion or hematoma.A subsequent whole abdominal computed tomography scan showed signs of upper abdomen peritonitis,mild ascites and a peri-renal hematoma around the lower right kidney(Figure 3).
FINAL DIAGNOSIS
Acute gastroenteritis complicated by DIC.
TREATMENT
The antimicrobial therapy was increased to 1 g meropenem every 12 h starting on day 3 for 3 days,followed by Piperacillin/Tazobactam from day 5 to 11 (Figure 2).A dose of 40 mg methylprednisolone daily was given intravenously for sepsis from day 3 to 4.On day 3,she was also given 400 mL fresh frozen plasma (commonly referred to as FFP) and ten units concentrated PLT (3-4 × 1011) to correct the coagulopathy and to control the right peri-renal hemorrhage.On day 4,the PLT was 77 × 109/L;WBC 14.39× 109/L;Hb 111 g/L.Another 200 mL FFP was given along with 20 mg methylprednisolone.On day 5,her diarrhea had resolved.The serum creatinine levels had plateaued at 220 μmol/L;PLT,98 × 109/L;LDH lowered to 952 U/L (Figure 2).Serum complement 3 (C3) and C4,and immunoglobulins G,A and M were within normal ranges.Serum anti-nuclear antibody,anti-cardiolipin antibodies,lupus anticoagulant,anti-beta 2 glycoprotein I,and extractable nuclear antigens were all normal or negative.On day 6,PLT was 127 × 109/L;WBC was 7.8 × 109/L.By day 11,serum LDH had decreased to 786 U/L and serum creatinine fell to 148.9 μmol/L (Figure 2).
OUTCOME AND FOLLOW-UP
The patient was feeling better and was discharged on day 11 after her condition further stabilized.At her 3 mo follow-up visit,her serum creatinine level was 78 μmol/L.
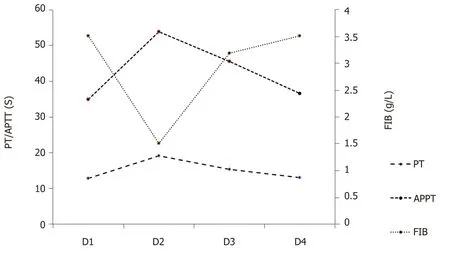
Figure1 The variations of prothrombin time,activated partial thromboplastin time and fibrinogen as a function of time from day 1 to day 4.
DISCUSSION
This previously healthy woman presented with the acute onset of abdominal cramping and diarrhea.Physical examination at presentation revealed hypotension and mild epigastric tenderness.The initial presentation was thought to be related to acute gastroenteritis,systemic inflammation syndrome and hypovolemic shock.The subsequent development with worsening thrombocytopenia,schistocytes,elevated serum LDH,and acute kidney injury suggested a diagnosis of HUS,but the presence of leukocytosis,coagulopathy,hypofibrinogenemia and spontaneous visceral bleeding indicated possible infection related-DIC.Differentiation between these diseases is crucial for proper clinical management.
Schistocyte
Schistocyte may be induced by mechanical fragmentation of RBCs when passing through strictured microvasculature.The Mayo Clinic issued a consensus statement that the “mere presence of schistocytes is adequate (for a diagnosis of TMA) in the appropriate clinical context”[4].But,correct interpretation of this marker can only be achieved if its significance and limitation under different clinical settings are understood.
Schistocytes are fragments of RBCs with the morphology of helmet cells;small,irregular,triangular,or crescent-shaped cells,pointed projections,and without central pallor[8].Their presence is suggestive of but not specific to TMA[9].In fact,a low rate of schistocytes at 0.05% ± 0.03% (range 0%-0.27%)[10],or ≤ 0.2%[11]may be observed in healthy donors.Further,it might be seen in disorders of erythrocyte cytoskeletal abnormalities or hemoglobinopathies,as well as a range of other conditions,chronic renal disease[10],renal failure[12],sepsis (0.87% ± 0.67%)[12],and mechanical heart valves(0.18% ± 0.15%[10]or 0.43% ± 0.32%[12]).It is noted that patients with TTP and HUS had a relatively higher schistocyte rate of 8.35% ± 2.74%[10]and 3.5% ± 1.88%[12],respectively.Although schistocytes can also be detected in the setting of DIC,it is seldom >1%.In a retrospective study of 35 patients (mostly in intensive care units),schistocytes were present in 30 subjects (85.7%),among which 20 patients (57.1%) had schistocytes< 0.5%,6 (17.1%) patients had schistocytes between 0.5%-1%,and only 4 (11.4%) had schistocyte counts ≥ 1%;The four DIC patients with schistocytes ≥ 1% had concurrent diseases of leukemia,pregnancy,and severe infection[11].The International Council for Standardization in Hematology recommends that ≥ 1% schistocytes in the absence of other moderate dysmorphic RBC is an important criterion for TMA[8].It is also important to note that automated schistocyte analysis is unreliable[12,13];the detection of schistocytes needs to be performed manually,and is thus subject to observer bias[10,12].Occasionally,at the early presentation of TMA,schistocytes may not be detected for up to 2-3 d on serial peripheral blood smear[14].Rarely,schistocytes have not been detected during TMA recurrence[15].
中国和欧盟是《公约》和《京都议定书》重要的参与者,双方开展气候合作始于1996年。1996年,欧委会制定《欧盟对华新战略》,不仅将“推动改善环境和可持续发展战略”作为欧盟对华四大战略之一,还讨论了推动中国改善环境和可持续发展战略的领域和手段[5]。2012年签署的《中欧能源安全联合声明》标志着中国和欧盟结成能源消费国战略合作伙伴关系。2016年,中国和欧盟签署《中国-欧盟能源合作路线图》,指出发展可再生能源是中欧能源合作的基础。
Serum LDH
LDH is a commonly used TMA biomarker[3],but its level is variable between patients.LDH catalyzes the reversible transformation of pyruvate to lactate under anaerobic conditions.Normal tissues produce five distinct function-related LDH isoenzymes with different electrophoretic mobility[16].LDH1 and LDH2 are primarily found in RBCs,heart muscle and the kidneys;LDH3 is highest in the lungs;LDH4 and LDH5 are highest in skeletal muscle and liver[17].Serum LDH increases in response to tissue injury,hemolysis,necrosis,hypoxia,and myocardial infarction.LDH is released from ruptured RBCs,and ineffective erythropoiesis has been regarded as an index of hemolysis.The routine determination of serum LDH includes all of the five isoenzymes.Interestingly,LDH isoenzymatic distributional study showed LDH1 and LDH2(erythrocytic origin) were not disproportionately elevated in 9 out of 10 TTP patients,suggesting the increased serum LDH observed in TTP patients is released from a variety of ischemic tissues rather than by intravascular hemolysis alone[18].In the context of TTP,LDH levels are unlikely to be > 2500 IU/L,and a higher level should raise the possibility of other hematological disorders,such as B12 deficiency[19].Rarely,LDH levels may not exceed the normal range in TTP.Among the 72 TTP patients reported in a series at Johns Hopkins University,the median serum LDH concentration was 1184 IU/L with an interquartile range of 152 to 5950 IU/L[20].In an Oklahoma TTP registry comprising 261 patients,serum LDH ranged from 114 to 12587 IU/L[21].In the TTP cohort from Washington University with 36 patients,serum LDH levels were between 328 and 28000 IU/L;32 out of the 36 patients had LDH < 2000 IU/L,and 35 out of the 36 patients had LDH < 3000 IU/L[22].As a biomarker,LDH is often used to monitor disease activity of HUS or TTP and treatment response.In practice,once the LDH is normalized or near normal for 2 consecutive days,therapeutic plasma exchange (TPE) for TTP or HUS may cease[23,24].However,LDH normalization has been shown to lag behind PLT recovery by an average of 9 d,so the initial LDH levels might not be used to predict response to TPE[20].
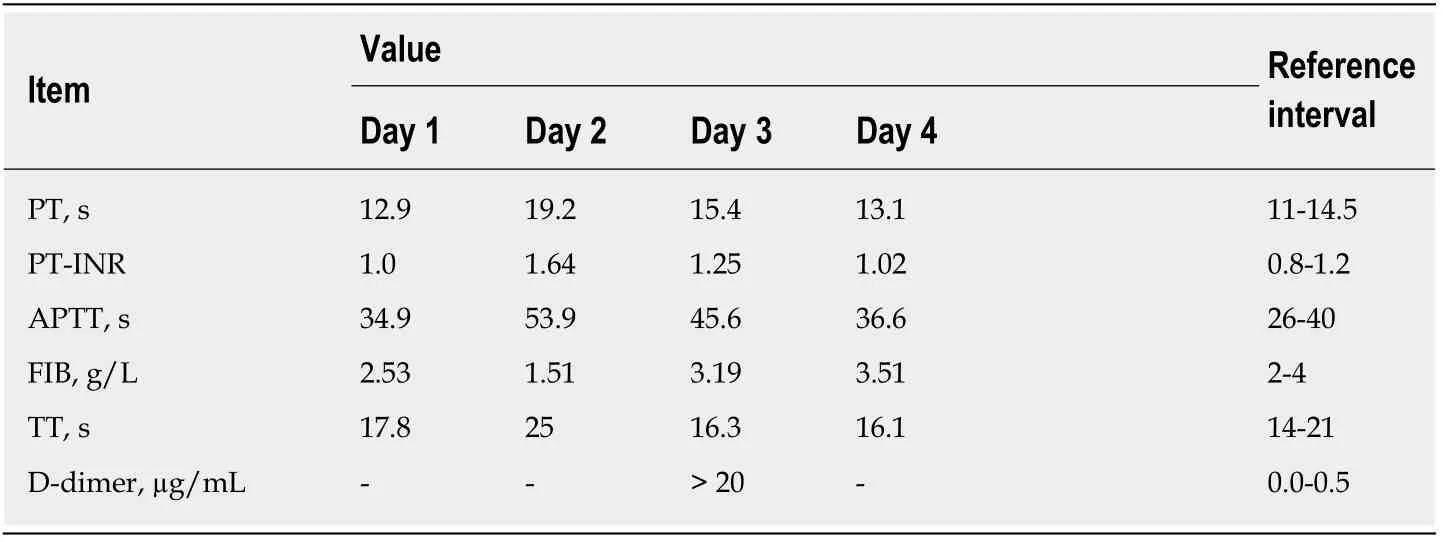
Table2 Clotting tests from days 1 to 4
Thrombocytopenia
Thrombocytopenia is commonly present in TTP and HUS.A depressed PLT may be caused by infections,hemodilution,increased consumption,decreased production,increased sequestration,drugs,and immune-mediated destruction.Thrombocytopenia is defined as PLT count below the lower limit of normal range (i.e.< 150 ×109/L for adults).The severity of thrombocytopenia can be further subdivided into mild (100-150 × 109/L),moderate (50-99 × 109/L),and severe (< 50 × 109/L)[25].Thrombocytopenia is generally prominent in TTP (< 30 × 109/L) due to extensive PLTrich thrombi formation[6].While significant thrombocytopenia (15-50 × 109/L) is typical of TMA[4],a normal PLT count at initial presentation does not exclude the diagnosis[6].There have been reports that PLT may fall within the normal range at TMA onset or during early recurrence of the disease[4].An abrupt decrease or a decreasing trend of PLT reflects progressive PLT consumption[26].Similarly,PLT may be used to monitor disease activity.It has been suggested that the restoration of PLT(above 150 × 109/L) signifies clinical remission and that TPE therapy may be discontinued[24].
Clotting abnormality
According to the Scientific Subcommittee on DIC of the International Society of Thrombosis and Hemostasis,DIC is “an acquired syndrome characterized by the intravascular activation of coagulation with loss of localization arising from different causes.DIC can originate from and cause damage to the microvasculature,if sufficiently severe,can produce organ dysfunction”[27].Using this definition,it is clearthat there is an overlap between DIC and TMA both clinically and pathologically.Some authors even consider DIC as a common cause of TMA[6].In contrary to DIC,the coagulation profile is essentially normal in TTP-HUS and other TMA diseases.Normal values of PT,APTT and Fib distinguish TTP-HUS from DIC in the presence of schistocytes and high LDH levels.In comparison with DIC control,a very low PLT count (< 20 × 109/L) and a PT within 5 s of the upper limit are specific to TTP-HUS[28].This is because the microthrombi plugged in TTP-HUS are PLT-rich[29,30],whereas in DIC,the microthrombi formed in small vasculature are rich in fibrin[31].

Table3 Urinalysis on day 2
ADAMTS13
ADAMTS13 (A Disintegrin And Metalloproteinase with Thrombospondin type 1 motif,member 13) is a specific marker for TMA.In addition,it is well known that TTP may result from severe functional deficiency of the VWF-cleaving protease ADAMTS13,which leads to accumulation of ultra-large VWF-multimers along the lumen of small blood vessels,resulting in extensive PLT/VWF-rich intravascular thrombus formation.ADAMTS13 assay includes activity,functional inhibitor (based on plasma mixing studies) and anti-ADAMTS13-IgG[6].The proteolytic activity of ADAMTS13 is considered “normal” if it is above 50% activity of the normal control(tested with pooled local blood samples).A high certainty of TTP (90% specificity) can only be made if the ADAMTS activity is < 10%[32].Such a low cut-off value (< 10% of normal activity) is applied because most ADAMTS13 molecules are bound to CD36(an integral membrane also known as PLT glycoprotein 4) on the endothelial cell surface.Therefore,thein vivoADAMTS13 activity exceeds the circulatory value determinedviaperipheral blood specimen[3].In practice,these assays are usually available in specialized centers and laboratories and are not easily available.
Shiga toxin-producing Escherichia coli (STEC) infection
Nowadays,HUS is generally divided into ST-HUS,secondary-HUS and atypical HUS(aHUS)[33].The majority of ST-HUS cases are caused by STEC or Shigella infections.Isolation of STEC and identification of alternative complement pathway defects may be used to pinpoint a definite illness underlying TMA syndrome.Approximately 6%-9% of STEC infections are complicated by ST-HUS.The triad of acute kidney injury,MAHA,and non-immune thrombocytopenia typically begin 5 to 10 d after the onset of diarrhea[34].The diagnosis of ST-HUS from atypical HUS may be challenging.Stool culture for STEC may take days,and Shiga toxin stool PCR assay is not widely used[35].A panel approach is required to identify complement disorders utilizing serological,genetic and flow cytometric analyses (CD46).However,apart from C3,C4 and CH50,the determination of AP components (e.g.,FH,FB,FI,CFHR1-5 and anti-FH) is not easily available.Serological detection of components of AP is neither sensitive nor specific[36].So far,genetic screening for dysregulated complement genes,mutation or deletion can be found in only approximately 50%-80% of complementmediated TMA[4,37].ST-HUS is best managed by supportive care with symptomatic treatment.Interestingly,antibiotic use is thought to increase the release of Shiga toxin and has been associated with subsequent development of HUS in some studies[38,39].Where acquired or hereditary TTP is suspected,treatment is necessary with TPE or FFP replacement,whereas eculizumab (complement inhibition) may be considered for cases of aHUS.
CONCLUSION
With reference to our case,the patient presented with diarrhea and vomiting without neurological deficit,in the background of severe thrombocytopenia,acute kidneyinjury,elevated LDH level and slightly increased schistocytes (0.6%).There was also an elevated indirect bilirubin level indicative of intravascular hemolysis.While the initial presentation was consistent with the clinical “triad” of ST-HUS,there were points to support DIC as a cause.In a typical ST-HUS case,abdominal pain and diarrhea often begin several days after contaminated food has been ingested,and thrombocytopenia and renal failure commonly occur after gastrointestinal symptoms are resolved[40],but this was not the case here.The schistocytes were < 1%,which makes the diagnosis of TMA less likely.The negative stool culture of STEC/Shigella and the presence of coagulopathy further argue against ST-HUS as the cause.According to the International Society on Thrombosis and Hemostasis (ISTH)diagnostic criteria of DIC can be made if the ISTH score ≥ 5 is in the context of gastrointestinal infection.Our patient scored 7 with reference to the ISTH-DIC score(PLT ≤ 50 × 109/L,2 points;3 s < PT < 6 s,2 points;a marked increased D-dimer,3 points).The presence of low rate of schistocytes,a high LDH level,acute kidney injury and perirenal hematoma fit well into a DIC diagnosis.
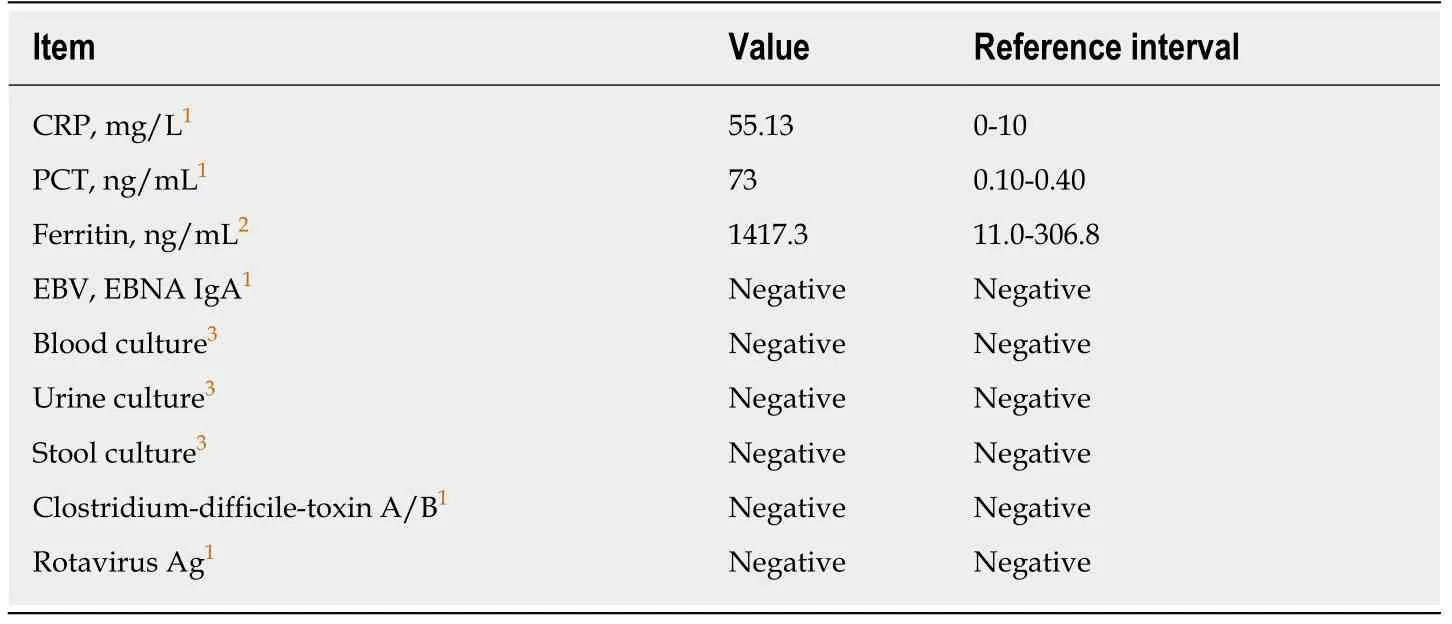
Table4 lnfection-related tests
In our case report,we made a diagnosis of infection-associated DIC,which allows timely treatment.Correct understanding and careful interpretation of various biomarkers including schistocytes,LDH,and PLT can enable clinicians to differentiate TMA from other related diseases.However,clinicians need to be aware that each of these biomarkers bears its own limitations in specificity and sensitivity.

Figure2 The variations of platelet,creatinine and lactate dehydrogenase as a function of time and interventions from day 1 to day 11.

Figure3 Abdominal computed tomography scan.
 World Journal of Clinical Cases2019年13期
World Journal of Clinical Cases2019年13期
- World Journal of Clinical Cases的其它文章
- Intracranial pressure monitoring:Gold standard and recent innovations
- Role of the brain-gut axis in gastrointestinal cancer
- Cholestatic liver diseases:An era of emerging therapies
- Neural metabolic activity in idiopathic tinnitus patients after repetitive transcranial magnetic stimulation
- Neuroendoscopic and microscopic transsphenoidal approach for resection of nonfunctional pituitary adenomas
- Safety and efficacy of transjugular intrahepatic portosystemic shunt combined with palliative treatment in patients with hepatocellular carcinoma
