Modified contralateral C7 nerve transfer: the possibility of permitting ulnar nerve recovery is confirmed by 10 cases of autopsy
Guang-Hui Hong , Jing-Bo Liu , Yu-Zhou Liu , Kai-Ming Gao , Xin Zhao , Jie Lao ,
1 Department of Hand Surgery, Huashan Hospital, Fudan University, Shanghai, China
2 Key Laboratory of Hand Reconstruction, Ministry of Health, Shanghai, China
3 Shanghai Key Laboratory of Peripheral Nerve and Microsurgery, Shanghai, China
Abstract Contralateral C7 nerve transfer surgery is one of the most important surgical techniques for treating total brachial plexus nerve injury. In the traditional contralateral C7 nerve transfer surgery, the whole ulnar nerve on the paralyzed side is harvested for transfer, which completely sacrifices its potential of recovery. In the present, novel study, we report on the anatomical feasibility of a modified contralateral C7 nerve transfer surgery. Ten fresh cadavers (4 males and 6 females) provided by the Department of Anatomy, Histology, and Embryology at the Medical College of Fudan University, China were used in modified contralateral C7 nerve transfer surgery. In this surgical model, only the dorsal and superficial branches of the ulnar nerve and the medial antebrachial cutaneous nerve on the paralyzed side (left) were harvested for grafting the contralateral (right) C7 nerve and the recipient nerves. Both the median nerve and deep branch of the ulnar nerve on the paralyzed (left) side were recipient nerves. To verify the feasibility of this surgery, the distances between each pair of coaptating nerve ends were measured by a vernier caliper. The results validated that starting point of the deep branch of ulnar nerve and the starting point of the medial antebrachial cutaneous nerve at the elbow were close to each other and could be readily anastomosed. We investigated whether the fiber number of donor and recipient nerves matched one another. The axons were counted in sections of nerve segments distal and proximal to the coaptation sites after silver impregnation. Averaged axon number of the ulnar nerve at the upper arm level was approximately equal to the sum of the median nerve and proximal end of medial antebrachial cutaneous nerve (left: 0.94:1; right: 0.93:1).In conclusion, the contralateral C7 nerve could be transferred to the median nerve but also to the deep branch of the ulnar nerve via grafts of the ulnar nerve without deep branch and the medial antebrachial cutaneous nerve. The advantage over traditional surgery was that the recovery potential of the deep branch of ulnar nerve was preserved. The study was approved by the Ethics Committee of Fudan University(approval number: 2015-064) in July, 2015.
Key Words: nerve regeneration; brachial plexus avulsion injury; nerve transfer; contralateral C7 nerve; modified surgery; deep branch of ulnar nerve; median nerve; medial antebrachial cutaneous nerve; hand function; neural regeneration
Graphical Abstract

Modified contralateral C7 nerve transfer surgery
Dorsal and superficial branches of ulnar nerve (dsbUN) and medial antebrachial cutaneous nerve (MACN) on the injured side were used as grafts. The contralateral C7 nerve (CC7) was transferred to the median nerve (MN)and the deep branch of ulnar nerve (dbUN).
Introduction
Brachial plexus avulsion injury is a most devastating injury to the upper extremity. Treatment is even more difficult when the supply of donor nerves is limited. Patients will completely or partially lose their motor and sensory functions of the affected side and suffer from serious physical and psychological harm (Hu et al., 2014; Wang et al., 2014;Yang et al., 2015a). Donor nerves from the brachial plexus,such as the phrenic nerve, accessory nerve, and intercostal nerves, are used to repair total brachial plexus avulsion injury (Gao et al., 2013b, 2018a). Contralateral C7 nerve (CC7)transfer surgery is one of the most important treatments.The first case of CC7 transfer was reported by Gu et al. in 1991 and later adopted by many other centers (Gu et al.,1991; Terzis et al., 2009; Wang et al., 2013, 2018; Tu et al.,2014; Vanaclocha et al., 2015). The CC7 on the intact side provided an abundant source of motor nerve fibers allowing some to be donated without permanent damage to the donor limb (Spinner et al., 2005; Chen et al., 2007; Li et al.,2017; Zheng et al., 2018). However, the traditional method using the whole ulnar nerve as a graft has some shortcomings. The traditional CC7 transfer surgery is performed in separate stages. In the first stage, the distal end of ulnar nerve (UN) on the paralyzed side is anastomosed with CC7;in the second stage, the proximal end of UN is anastomosed with a recipient nerve such as the median nerve (MN) (Gao et al., 2006; Chuang et al., 2012). The disadvantage of using the whole UN as a graft is that the possibility of recovery of the intrinsic muscles innervated by UN is completely sacrificed. On the other hand, as the CC7 transfer contains a large amount of nerve fibers, it has been suggested that it could be used for restoring more than one recipient nerve(Shin et al., 2005; Gao et al., 2018b).
In view of the drawbacks of traditional CC7 transfer surgery, we designed a modified CC7 transfer procedure. In this procedure, the deep branch of the ulnar nerve (dbUN)on the injured side was preserved, while the dorsal and superficial branches of the ulnar nerve (dsbUN) were used as grafts. The medial antebrachial cutaneous nerve (MACN)was also used to bridge the gap between the proximal end of ulnar nerve (peUN) and the proximal end of dbUN. In this way, both the dbUN and MN were innervated.
The present study aimed to investigate the feasibility of this modified CC7 transfer surgery in cadavers. The axons were counted to study the degree of matching in the number of donor and recipient nerve fibers.
A completely new design was used in modifying traditional CC7 nerve transfer surgery. Although it was traditionally supposed that it would be impossible to recover the function of the ulnar nerve after total brachial plexus avulsion injury,there remained the possibility of using the ulnar nerve as a graft without sacrificing the whole nerve.
Materials and Methods
Materials
A total of 20 upper extremities in 10 fresh cadavers that have been dead for 5-10 days (4 males and 6 females; aged 70.6 ±6.6 years old, ranged from 59 to 82 years old), provided by the Department of Anatomy, Histology, and Embryology at the Medical College of Fudan University, China, were dissected. This study was carried out in the Anatomy Department of Shanghai Medical College, Fudan University.The study was approved by the Ethics Committee of Fudan University (approval number: 2015-064) in July, 2015.
Surgical technique
The modified CC7 transfer surgery was carried out in four steps. In the first step, dbUN was fully separated from the UN under a 5× magnification loupe and disassociated as distally as possible. The sample was sectioned at the point when it could not be further separated from the UN. In this way, the neuromuscular junction between dbUN and the intrinsic muscles was preserved (Figure 1A). In the second step, the dsbUN was dissected at the proximal end of Guyon's Canal where it was sectioned. The dsbUN was drawn to the contralateral side through the subcutaneous route and then anastomosed with CC7 (Figure 1B). In the third step,the proximal end of UN (peUN) was sectioned and anastomosed with the MN and proximal end of MACN (peMACN)(Figure 1C). In the last step, the distal end of MACN(deMACN) was anastomosed with dbUN (Figure 1D). The schematic diagram comparing the traditional and modified CC7 transfer surgeries is shown in Figure 2. Distances from dbUN and peMACN to the midpoint of the line between the medial and lateral epicondyles of the humerus were recorded respectively. It was decided that it would be feasible to suture the deMACN and dbUN directly.
In the traditional CC7 transfer surgery, the CC7 on the intact side was also transected proximal to the point where it joined with other nerves. The whole UN on the injured side was transected at the wrist level and drawn to the supraclavicular area on the intact side through the subcutaneous tunnel. The distal end of CC7 was anastomosed with the distal end of the reversed UN. The peUN was anastomosed with the peMN (Figure 2B) or other targets (such as musculocutaneous nerve).
Silver impregnation
After these four steps, the axon numbers of bilateral C7 nerves, dsbUN, peUN, peMACN, peMN, deMACN, and dbUN were harvested and stained by the silver impregnation method.
The specimens of nerve tissues were obtained and fixed with formalin and then embedded in paraffin blocks. The paraffin blocks were sliced into sections 5-8 μm thick for pathological studies and mounted on slides. The sections were then gently placed in xylol for 5 minutes, absolute alcohol for 5 minutes, 95% alcohol for 5 minutes and washed in distilled water. They were immersed in a mordant, which contained 30 mL silver nitrate, 10 drops of 2% pyridine and 15 drops of absolute alcohol, at 60°C until they turned yellow. The samples were quickly washed in 95% alcohol, and then impregnated in a solution containing 30 mL Hortega's strong silver carbonate, 10 drops pyridine and 15 drops of absolute alcohol at 60°C until they darkened. After rapid washing in 95% alcohol, the sample were reduced in 10%formol for one to two minutes, washed in distilled water,and left in a 2% oxalic acid solution for a few minutes until the sections turned reddish. This step accentuated the staining of axons. The sample was fixed, if desired, in a 5%solution of sodium thiosulfate, washed in distilled water, dehydrated, cleared and mounted in balsam. All the reagents were provided by the Sinopharm Chemical Reagent Co.,Ltd., Shanghai, China.
Axon counting
The total number of axons was calculated for each specimen and counted under 200× magnification with Leica Microsystems (LeicaDWLB2, Leica, Heidelberg, Germany). The axon ratio of CC7 to dsbUN, peUN axons to the sum of peMACN and peMN, and deMACN to dbUN were calculated.
Images were taken using a Motic Med 6.0 digital medical image analysis system (Xiamen Motic Software Engineering Co., Ltd., Xiamen, China), at 200× magnification and the number of axons were counted by clicking one by one.
The distance between either of two coaptating nerve ends in the bilateral upper extremities of each cadaver was the primary outcome. The numbers of axons in nerve segments distal and proximal to the coaptation sites were also counted.
Statistical analysis
Results were expressed as the mean ± SD, and analyzed using SPSS 17.0 software (SPSS Inc., Chicago, IL, USA).
Results
Distances between either of two coaptating nerve ends
In all of the 10 cadavers, CC7 could be transferred to the MN and dbUN on the paralyzed side together with the combined nerve grafts of dsbUN and MACN.
The distance between the starting point of dbUN and the midpoint of the line between the medial and lateral epicondyles of the humerus were close to the distance between the branching point of the MACN and the midpoint of the line between the medial and lateral epicondyles of the humerus (Table 1). Therefore, the distal end of MACN and the proximal end of dbUN were close to each other, and close to the line between the medial and lateral epicondyles of the humerus, allowing direct suturing between them. This exploratory study of modified CC7 transfer surgery was successfully performed in 10 cadavers.
Axon number counting
The representative cross sections of nerve segments were shown in Figure 3. The axon numbers were presented in Table 2. The matching degree of axonal counts proximal and distal to the anastomosed sites was presented as ratios. The ratio of right C7 nerve root to the left dsbUN was 19:1. The ratio of left C7 nerve root to right dsbUN was 17:1. The ratio of peUN to the sum of peMN and peMACN was 0.94:1 on the left side and 0.93:1 on right side. The ratio of deMACN to dbUN was 0.61:1 on the left side and 0.65:1 on the right side.
Discussion
The traditional CC7 transfer surgery, first reported by Gu et al., has been one of the most important treatments for total brachial plexus avulsion injury (Gu et al., 1991). It has also been performed in many clinical centers all over the world(Yang et al., 2015b; Jiang et al., 2016). It is especially useful when other donor nerves (such as the accessory nerve,phrenic nerve and intercostal nerves) are also injured or not sufficient for repairing all the target nerves. In these cases,no donor nerves are available from the ipsilateral side therefore the CC7 from the intact side becomes the best available source for transfer (Cambon-Binder et al., 2018; Dahlin et al., 2018; Socolovsky et al., 2018). According to Terzis et al.'s report, fair (M2+to M3), good (M3+to M4-) and excellent(M4+to M5-) outcomes have been achieved in a total of 56 cases of brachial plexus nerve injuries where the functional recovery rates (M3 or more) were 74% in biceps, 57% in triceps, 50% in deltoids, 62% in wrists and finger flexors, and 50% in wrists and finger extensors, respectively (Terzis et al.,2000). In the traditional technique of CC7 transfer surgery,Gu and co-workers (1991) used the entire CC7 elongated by a vascularized ulnar nerve graft from the paralyzed upper extremity. Therefore, the recovery potential of the intrinsic muscles innervated by the UN was completely sacrificed, as the physical connectivity between dbUN and the intrinsic muscles is the primary foundation for the restoration of the hand functions.
However, the C7 nerve contains 27,000-41,000 nerve fibers, which is an abundant source to reconstruct not only a single recipient but also multiple recipients (Chen et al.,2007; Xu et al., 2008). Gao et al. (2013a) reported that acceptable outcomes have been achieved by CC7 transferred to the musculocutaneous nerve and MN. This meant that the benefit of CC7 transfer grew from repairing a single nerve to multiple nerves. However, in the traditional CC7 transfer surgery, the whole UN was harvested as the grafted nerve to restore the function of a single MN on the paralyzed side. Although this might have wasted some of the fibers of the CC7 nerve, it was traditionally supposed that it was impossible for the UN on the injured side to recover after high-level injury (Woo et al., 2015; Bertelli et al., 2018).Therefore, the whole UN was sacrificed and used as a graft.As the microsurgical techniques and research in the nerve regeneration have progressed (such as brain reorganization theory, nerve conduit, electrical nerve stimulation, stem cell transplantation, ultrasound treatment, and tissue engineering techniques), it was realized that there was greater potential for the recovery of the UN (Li et al., 2015; Zhang et al.,2015; Geuna et al., 2016; Jiang et al., 2017; Zhou et al., 2017;Bergmeister et al., 2018; Choi et al., 2018; Yu et al., 2018).Therefore, there was a need to devise a method to preserve the recovery possibility of the UN nerve on the injured side.The present study provided a strategy for modifying the traditional method of CC7 transfer.
In our study on cadavers, we have verified that the connection between dbUN and intrinsic muscles could be retained, thus the recovery potential of dbUN was preserved.A combination of dsbUN and MACN was used as nerve grafts for reinnervating both the MN and dbUN simultaneously. Through this modified CC7 transfer surgery, we aimed to preserve innervation of the hypothenar, adductor pollicis, palmar interosseous, dorsal interosseous and the 3/4 of the lumbrical muscles.
The cut ends of dbUN and MACN were located at the elbow so that they could be directly anastomosed without additional nerve grafts.
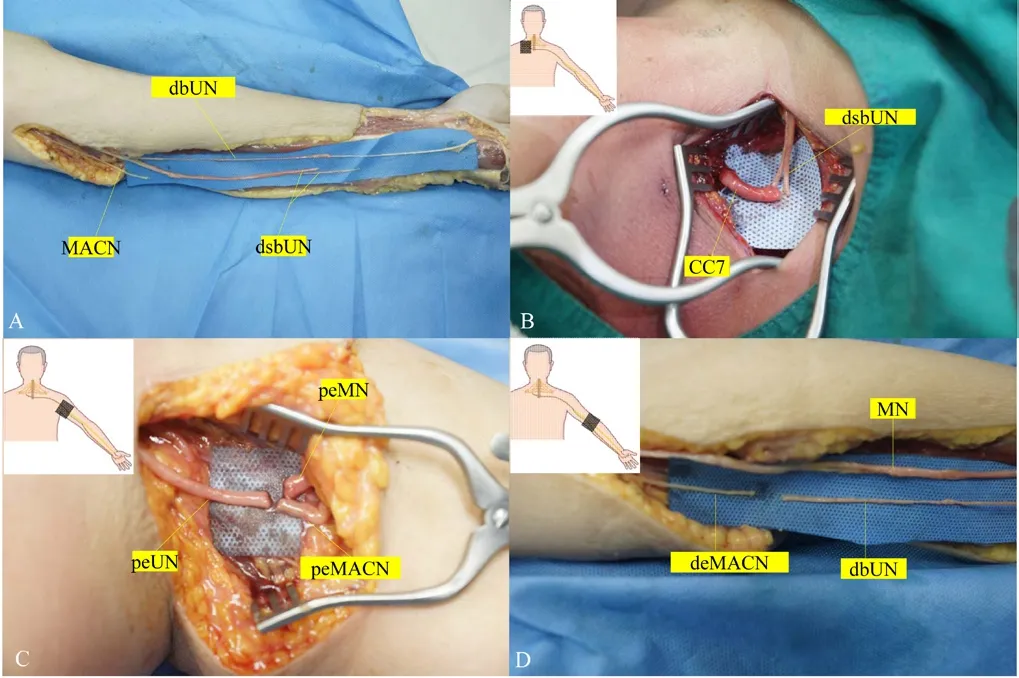
Figure 1 Demonstration of modified contralateral C7 (CC7) nerve root transfer.(A) Exposure of the full length of ulnar nerve (UN) and the medial antebrachial cutaneous nerve (MACN). The deep branch of UN (dbUN)was separated from the main trunk. The distal and superficial branches of UN (dsbUN) were transected at the wrist level. (B) The contralateral C7 nerve was transected proximal to the point where it joined with other nerves. The distal end of the dsbUN was drawn to the supraclavicular area of the contralateral side through the subcutaneous tunnel and anastomosed with the CC7. (C) The UN was reversed and the proximal end of ulnar nerve (peUN) was transected and anastomosed with the proximal end of MACN (peMACN) and proximal end of median nerve (peMN) simultaneously at the upper arm level. (D) The distal end of MACN (deMACN) was anastomosed with proximal end of dbUN.
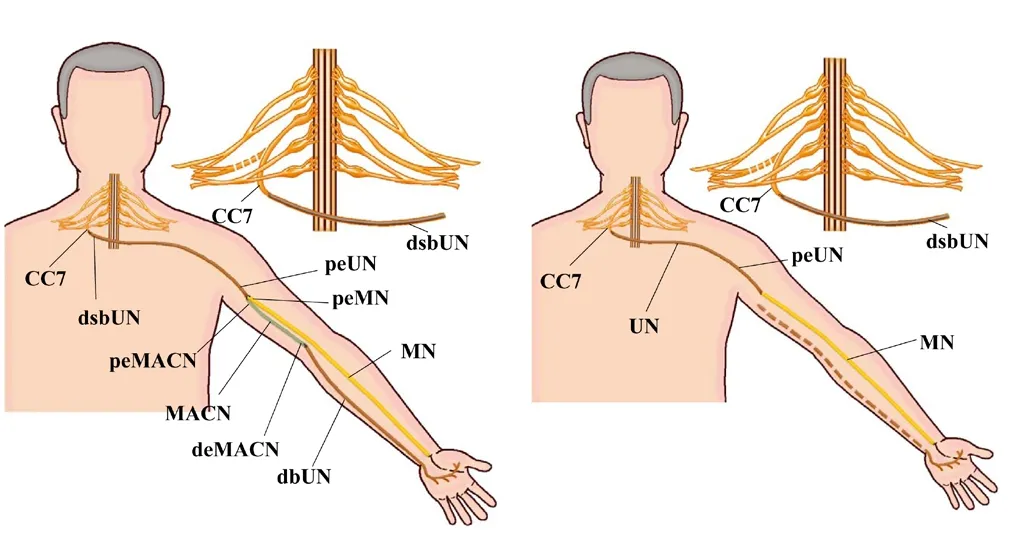
Figure 2 Comparison of the modified and traditional contralateral C7 (CC7) nerve transfer surgeries.(A) Demonstration of modified CC7 nerve transfer surgery. CC7 on the intact side was transected proximal to the point where it joined with other nerves. The distal and superficial branches of ulnar nerve(dsbUN) on the injured side were transected at the wrist level and drawn to the supraclavicular area of the contralateral side through the subcutaneous tunnel. The deep branch of UN (dbUN) was dissected from the main trunk of ulnar nerve (UN). The distal end of CC7 was anastomosed with the dsbUN. The proximal end of UN (peUN) was anastomosed with both the proximal end of median nerve (peMN) and the proximal end of medial antebrachial cutaneous nerve (peMACN).The distal end of medial antebrachial cutaneous nerve (deMACN) was then anastomosed with the dbUN. (B) Demonstration of traditional CC7 nerve transfer surgery. The CC7 on the intact side was also transected proximal to the point where it joined with other nerves. The whole UN was transected at the wrist level and drawn to the supraclavicular area of the contralateral side through the subcutaneous tunnel.The distal end of CC7 was anastomosed with the distal end of the reversed UN. Then the peUN was anastomosed with the peMN. The continuous lines indicated the nerve path after nerve transfer surgery.The dash line indicated the original position of the UN before nerve transfer surgery.
In the axon count study, the number of axons in CC7 was sufficient to be used as a donor. Moreover, the sum of MN and dbUN axon numbers matched with that of the nerve grafts, i.e. the combination of MACN and dsbUN.
At the medial aspect of the paralyzed upper arm, we simultaneously anastomosed peUN with peMN and pe-MACN. The axon number of peUN also matched with the sum of peMN and peMACN. As MACN and UN originate from the medial cord of brachial plexus, UN could be readily anastomosed with MACN at the same level of the upper arm. Since the axon number of deMACN and dbUN roughly matched (0.6:1), dbUN could be anastomosed with deMACN after separation. Therefore, it was anatomically feasible to anastomose deMACN with dbUN, according to the principle that the axon number of donor nerve should equal to at least 30% of that in the recipient nerve (Zhang et al., 2011; Chuang et al., 2012; Benedikt et al., 2017).
There were several advantages using dsbUN combined with MACN as the grafted nerve to reinnervate multiple recipient nerves using this modified CC7 transfer surgery. First, the dbUN was preserved so that the recovery potential of intrinsic muscles innervated by dbUN was not completely sacrificed.Second, the anatomical location of the grafted nerve remains unchanged. Third, the blood supply of the grafted nerve could be largely preserved. Finally, no extra incisions were needed and the source of CC7 was fully utilized.
The modified CC7 transfer surgery still has some shortcomings. The deep, superficial and dorsal branches of the UN were very complex at the meeting point, i.e., 10 cm proximal to the wrist, making it difficult to dissect from the main trunk of UN. The dissecting procedure should be carried out carefully under the loupe magnification to acquire as many nerve bundles as possible. After separation of the dbUN, nerve fibers on the distal end of UN left for grafting was less than those in the traditional method. Whether it would eventuallyaffect the functional recovery of the recipient nerve or not would need clinical evaluation. The comparison of advantages and disadvantages of the modified and traditional CC7 transfer surgeries has been presented in Table 3.
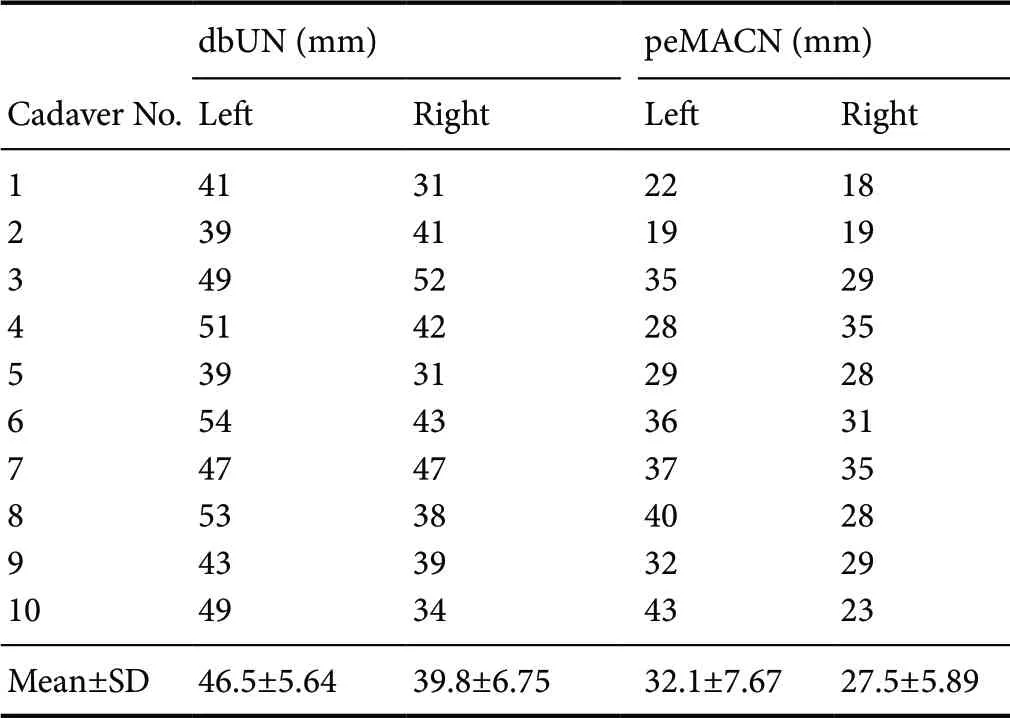
Table 1 Distances from the deep branch of ulnar nerve (dbUN) and the proximal end of medial antebrachial cutaneous nerve (peMACN)to the midpoint of the line between the medial and lateral epicondyles of the humerus
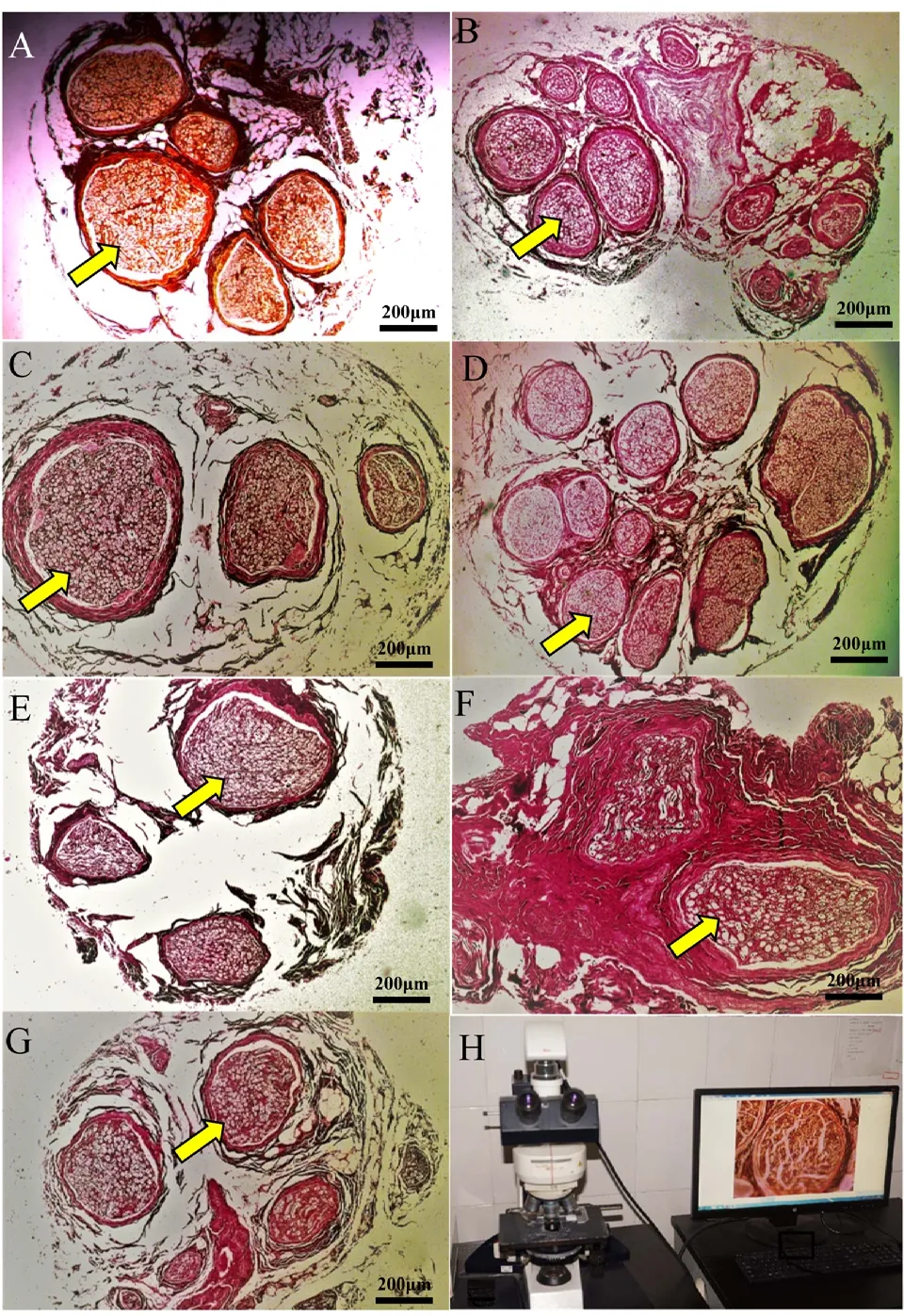
Figure 3 Histology of axons in the nerves after silver impregnation under optical microscope involved in the modified contralateral C7 nervetransfer surgery.All axons of involved nerves were stained by silver impregnation. (A)Cross-sectional view of the C7 nerve root; (B) cross-sectional view of dorsal and superficial branches of ulnar nerve; (C) cross-sectional view of proximal end of ulnar nerve; (D) cross-sectional view of the proximal end of median nerve; (E) cross-sectional view of the proximal end of medial antebrachial cutaneous nerve; (F) cross-sectional view of the distal end of medial antebrachial cutaneous nerve; (G) cross-sectional view of the deep branch of ulnar nerve; (H) demonstration of the Leica Microsystems used in the slice observation. Yellow arrows indicate axons in cross sections of nerves. Original magnification: 200×. Scale bars: 200 μm.
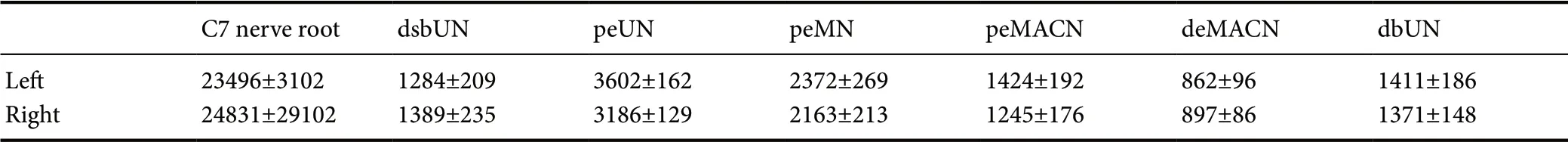
Table 2 Number of axons in the nerves involved in the modified contralateral C7 nerve root transfer surgery
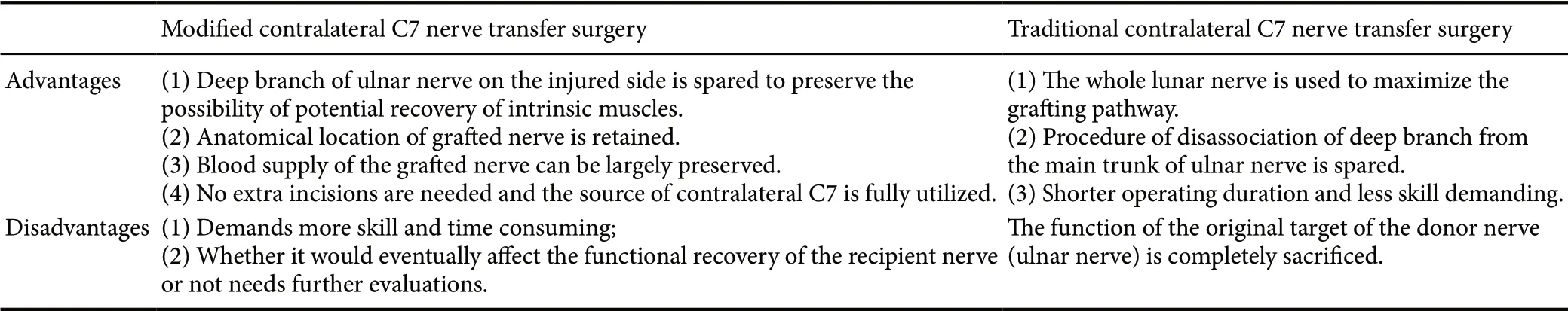
Table 3 Comparison of advantages and disadvantages between modified and traditional contralateral C7 nerve transfer surgeries
When this modified CC7 transfer surgery is applied in clinical practice, a two-stage surgery is suggested for the modified CC7 transfer. In the first stage, the dbUN is labeled and fixed subcutaneously by a suturing line nearby the elbow joint. The dsbUN should be drawn to the contralateral side through anterior cervical subcutaneous tunnel and anastomosed with CC7 nerve. In the second stage, the peUN is anastomosed with MN and peMACN simultaneously and then deMACN was anastomosed with dbUN, which has been labeled a suturing line. This surgical approach is clinically feasible.
However, the present study was only an anatomical investigation. There might still be limitations for extrapolating this surgery in clinical practice. Recovery of the intrinsic muscles in the injured upper extremity is still uncertain due to the long distance from the donor nerve to the recipient nerve. The restoration of intrinsic muscle of the paralyzed hand is still a difficult problem for total brachial plexus avulsion injuries (Giuffre et al., 2010; Aszmann et al., 2015;Dy et al., 2015; Franzblau et al., 2015; Yang et al., 2016).The present study verified the feasibility of a modified CC7 transfer surgery on cadavers. In conclusion, it is anatomically feasible that the CC7 can be transferred to the MN and the dbUN grafted by dsbUN combined with MACN from the paralyzed side. This approach may provide a theoretical and practical basis for preserving the recovery potential of the intrinsic muscles with a modified CC7 transfer surgery.
Author contributions:Study design: JL and GHH; experimental implementation: GHH and KMG; data analysis and paper writing: JBL, YZL and XZ.All authors approved the final version of the paper.
Conflicts of interest:The authors declare that there are no conflicts of interest associated with this manuscript.
Financial support:This study was supported by the National Natural Science Foundation of China, No. 81572127 (to JL). The funder played no role in the study conception and design, collection, analysis and interpretation of data in the writing of the paper, and in the decision to submit the paper for publication.
Institutional review board statement:The study protocol was approved by the Ethics Committee of Fudan University of China (approval number: 2015-064) in July, 2015.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- Improvement of ataxia in a patient with cerebellar infarction by recovery of injured cortico-ponto-cerebellar tract and dentato-rubro-thalamic tract: a diffusion tensor tractography study
- Tandem pore TWIK-related potassium channels and neuroprotection
- Dendritic shrinkage after injury: a cellular killer or a necessity for axonal regeneration?
- Regenerative biomarkers for Duchenne muscular dystrophy
- Exploring the efficacy of natural products in alleviating Alzheimer's disease
- Role of macrophages in peripheral nerve injury and repair

