Symptoms of dengue at the acute and post-infection stage in the Western Province, Sri Lanka: A cross-sectional study
Chrishantha Abeysena, Sharika Peiris, Indrakantha Welgama, Upul Gunasekara, Kolitha Wickramage
1Lab1Department of Public Health, Faculty of Medicine, University of Kelaniya, Ragama, Sri Lanka
2Consultant, United Nations Migration Agency
3Medical Officer, Ministry of Health, Sri Lanka 4Global Research and Epidemiology Coordinator, United Nations Migration Agency, Geneva
Keywords:Control Dengue Outbreak Symptoms Vector Virus
ABSTRACT Objective: To describe the symptoms of dengue at acute and post-infection stage and to identify preventive strategies adopted by the patients in the Western Province, Sri Lanka.Methods: This was a descriptive cross-sectional study conducted in the Western Province of Sri Lanka in November 2017. The study population consisted of 473 confirmed dengue patients aged from 18 to 64 years who were hospitalized between June and August 2017. A stratified random sampling technique was applied to select the participants. Data collection was done by trained interviewers, using a structured, pre-tested interviewer-administered questionnaire.Results: The most common symptoms of dengue fever at the acute stage was body ache(81.81%, n=387), followed by headache (71.67%, n=339), loss of appetite (66.80%, n=316),tiredness (53.06 %, n=251) and vomiting (41.86%, n=198). The most common symptom during the post-infection stage was body ache (48.62%, n=230), followed by fatigue (39.74%,n=188), and loss of appetite (28.75%, n=136). Adding sand to the water in places where water accumulates (41.64%, n=197) was the most common method used to prevent transmission of dengue followed by removing/draining stagnant water regularly (36.15%, n=177). Use of mosquito nets (83.08%, n=393) was the most common method in preventing mosquito bites followed by the use of fans among dengue patients (56.02%, n=265).Conclusions: The study shows a prolonged persistence of clinical symptoms during the postinfection period.
1. Introduction
Dengue is one of the most common causes of viral fever outbreaks in Sri Lanka. The country is now recognized as hyper-endemic for dengue, with co-circulation of multiple serotypes of the virus at any given time[1]. In the recent past, Sri Lanka has witnessed several unusually large epidemics of dengue, with increasing case incidence. Usually, there are two dengue outbreaks twice a year and the outbreak from May to August 2017 was reported as the worst ever in history, causing over 300 deaths island wide. Approximately 43.5% of dengue cases had been reported from the Western Province[2].
There were anecdotal evidence and observations by the clinicians about complaints by the patients that there were prolonged symptoms following the dengue outbreak in 2017. According to the clinicians, these symptoms included body ache, skin rashes, and generalized body weakness. These symptoms have lasted for many weeks after the infection and have caused significant disability to the patients, affecting their quality of life and socio-economic aspects.Encephalopathy and liver failure are uncommon complications of dengue haemorrhagic fever, which are associated with a high mortality rate[3]. It is a burden to the health care cost as well as the economy of a country[4,5]. Evidence also recognizes the possible impact of the prolonged clinical symptoms following dengue on economic productivity[6]. Although there was some evidence reporting the prolonged persistence of clinical manifestations following dengue[1,2], literature was scarce about the situation in Sri Lanka. Therefore, this study was designed with the aim of broadening the understanding of post-infection debilitation and documenting symptoms of persons affected with dengue in Sri Lanka.
2. Material and methods
The study design was a descriptive cross-sectional study. This was conducted in the Western Province, which consists of Colombo,Kalutara and Gampaha Districts. The Western Province was purposively selected as the study area due to its highest number of dengue cases according to the reports from the Epidemiology Unit of the Ministry of Health. The data on confirmed dengue cases in the province were collected from the Medical officer of Health(MOH) areas. According to the routine surveillance mechanism in the country, the MOH receives a notification from the hospital once a patient is diagnosed with dengue. This information is recorded in the notification register. Using this information, the Public Health Inspector (PHI) conducts the field level investigation on the patient and surroundings. Following this investigation, the PHI enters information of all confirmed cases in the Infectious Diseases Register which is maintained by the Supervising Public Health Inspector. The dengue patients who had been hospitalized during the months of June to August 2017 was selected for the purpose of this study. Data collection period was November 2017. The study population consisted of patients diagnosed with dengue aged between 18 and 64 years, who were confirmed and entered in the MOH Infectious Diseases Register. Patients with mental disabilities,who are unable to comprehend and answer the questions on their own, were excluded from the study.
2.1. Sample size and sampling
Assuming that one in every four dengue patients (25%) complains of post-infection symptoms and the level of absolute precision as 5% and the design effect as 1.5, the required minimum sample size was 432 patients. When adjusted for a 20% non-response rate,the final sample size required to be interviewed was 520 patients.Stratified random sampling technique was used under which the primary sampling unit was a district and secondary sampling unit was a MOH area. Four MOH areas were selected randomly from each district after listing and numbering them in the alphabetical order which totalled to 12 MOH areas from the Western Province.Study subjects were selected proportionate to the total number of population in the district area as 1:2:2 respectively, 104 from the Kalutara District, 208 dengue patients each from Colombo and Gampaha districts. However, we increased the sample size during the implementation stage due to a higher non-response rate than the expected. From a MOH area in each district, an equal number of patients were selected. The records of the dengue confirmed patients who had been affected by dengue from the months of June to August 2017 were selected as the sampling frame. Confirmed cases were listed and sorted according to the date of entry in the confirmed cases register of the Supervising Public Health Inspector of each selected MOH office, and the required number of subjects from the MOH area were selected using random number tables.
2.2. Data collection
The data collection was done by trained interviewers using an interviewer-administered questionnaire. This structured questionnaire was designed by a team of experts in the fields of clinical and community medicine using the available literature and published recommended guidelines on dengue to ensure face validity and content validity of the questionnaire. Pretesting the questionnaire was done using a sample of similar patients, but living outside of the Western Province in this case from the Ratnapura district. Twelve pre-intern medical officers were selected as data collectors and were provided with thorough training on data collection and entering the data into a computer-based worksheet. Data collectors also explained the voluntary participation of the patients and the possibility of withdrawing from the study at any time. The data collectors were regularly supervised by the investigators to ensure the quality of the data collection and data entering. All data collectors were given an equal number of questionnaires. They were provided with transport facilities to visit the households. Data collectors were advised to first call the patients using the contact numbers obtained from the register and to get an appointment prior to visiting them. Then the data collectors met the patient at an agreed place and conducted the interview after getting informed written consent from the patient.Participants' anonymity and strict confidentiality of information were maintained.
2.3. Data analysis
Post dengue infection symptoms were assessed by calculating the percentage of patients who had experienced dengue-related disease symptoms for a period of one week or more, after being discharged from the hospital. All data were entered into an MS Excel data sheet.We used SPSS for Windows, Version 16.0. Chicago for data analysis.The incidence of symptoms was calculated. The chi-squared test was applied to assess the difference of incidence of symptoms across the sex and age groups. Stratified analysis was performed to assess any confounding effect.
The ethical clearance was obtained from the Ethics Review Committee of the University of Kelaniya (Ref No: P/271/11/2017).Permission to conduct the study was obtained from the Director General of Health Services of the Ministry of Health, the Provincial Director of Health Services (Western Province), the Regional Directors of Health Services and respective MOH's prior to conducting the study.
3. Results
We invited 650 dengue patients to participate. A total of 473 patients participated in the study, with a response rate of 72.76%.The flow diagram describes the process of recruitment to the study(Figure 1). The mean age of the participants was 36.6 (SD=13) years and age range was between 18 to 64 years. There were 182 (38.48%)dengue patients who were below the age of 30 years, 209 (44.18%)between 31 and 50 years, 80 (16.91%) above 50 years and 2 (0.42%)missing data. The percentage of male and female patients were 48.62% (n=230) and 51.37% (n=243) respectively. A total of 71.03%(n=336) of the dengue patients had completed the general certificate of education, ordinary level (Grade 10).
Figure 1. Study flowchart.
The median duration of hospital stay was 5 d (IQR 4 to7 d). A total of 187 (39.53%) patients stayed for more than 5 d in the hospital.46 (9.72%) patients were admitted to an Intensive Care Unit (ICU).Among them, 17 (36.95%) stayed only a day in the ICU and 7(15.21%) stayed for more than 4 d (range 1-10 d). A total of 123(26.00%) patients had complications due to the disease, and of them,66(13.95%) had complications related to chest, 62(13.10%) to the abdomen and one to heart. A total of 170 (35.94%) of them thought that they contracted the disease at home and 141 (29.80%) assumed it was at the workplace. Two hundred and five (43.34%) patients worked in an open environment, for example, in the field.
3.1. Symptoms of dengue during the acute and post-infection stage
The most common symptoms of dengue fever during acute stage were body ache (myalgia/arthralgia) (81.81%), followed by headache (71.67%), loss of appetite (66.80%), fatigue (53.07%) and vomiting (41.86%). The least common symptoms were numbness(1.05%) followed by skin rashes (8.03%). The most common symptoms during the post-infection stage were body ache (48.63%),followed by fatigue (39.74%), and loss of appetite (28.75%). At least one symptom appeared for 79.70% (n=377) of patients during the post-infection period (Table 1). The median number of symptoms appeared during the acute stage and post infection stage was 4.92(IQR 3-6) and 1.0 (IQR 1-3) respectively.
A significantly higher percentage of vomiting, fatigue, and loss of weight were reported by those who stayed in the hospital for five or more days compared to those who stayed less than five days during the acute stage. A significantly higher percentage (86.10%) of participants who stayed for five or more days in the hospital during the acute stage complained of at least one symptom during the post infection stage compared to those who stayed less than five days in the hospital (75.52%). The association between those who stayed for more than five days in the hospital during the acute stage and complained of at least one symptom at the post infection stage was assessed by stratification based on sex and age categories. It has shown that those who stayed for five or more days in the hospital during the acute stage had a higher percentage (n=63, 86.30%) of at least one symptom during the post infection stage than those who stayed for less than five days in the hospital (n=73, 66.97%) among the age group below 30 years (P=0.003). Similarly, it was shown that those who stayed for five or more days in the hospital during the acute stage had a higher percentage (n=82, 85.41%) of at least one symptom during the post infection stage than those who stayed for less than five days in the hospital (n=94, 70.15%) among the males(P=0.007). A higher percentage (n=40, 86.95%) of patients among those who have been admitted to an ICU during the acute stage hadat least one symptom during the post infection stage than those who had not been admitted to an ICU (n=337, 78.92%, P=0.198).
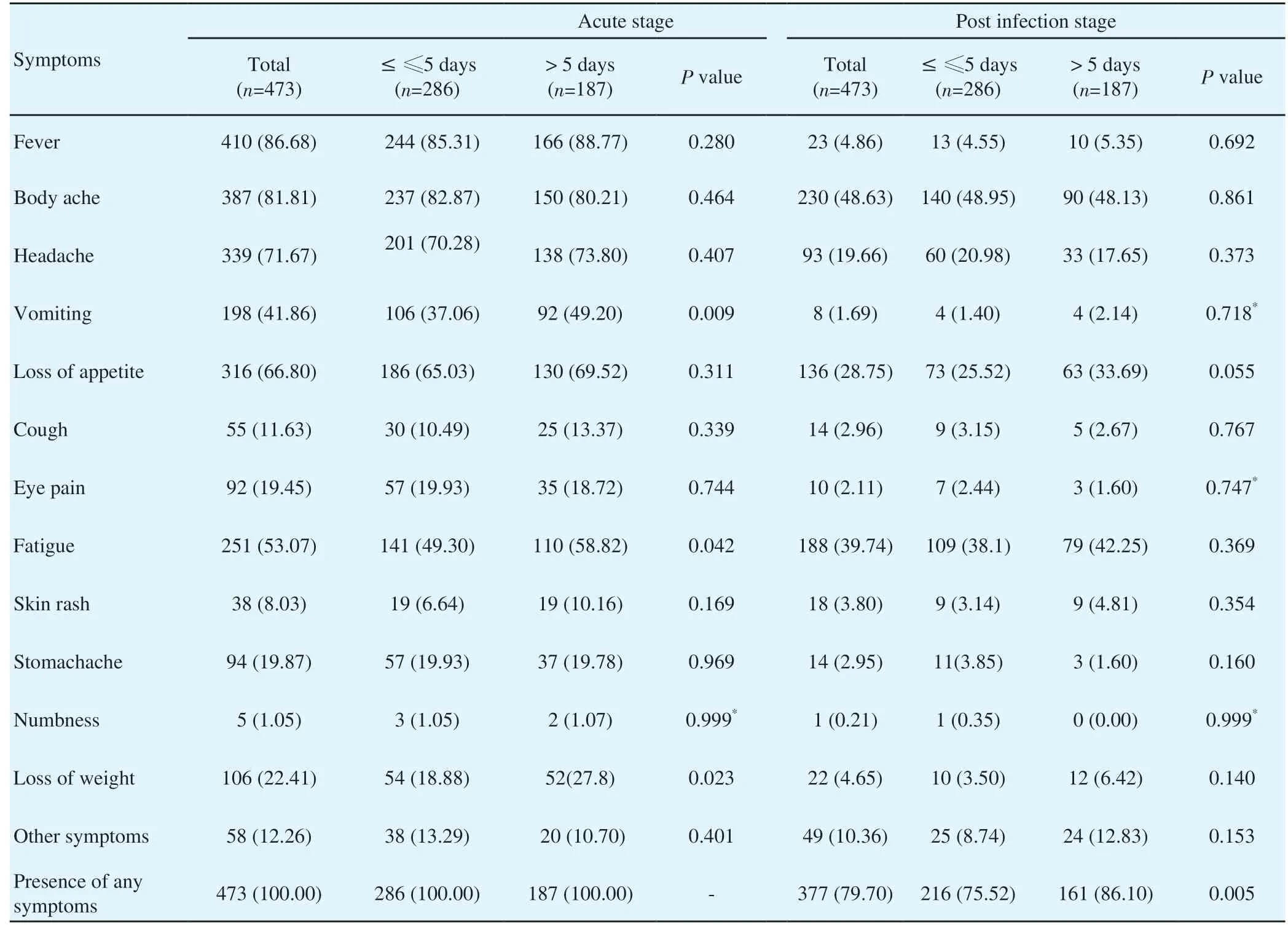
Table 1. Symptoms of dengue fever during the acute and post infection stage by duration of hospital stay.

Table 2. Post infection dengue symptoms across the age and sex categories.
There was a statistically significant higher incidence of vomiting,loss of appetite and other symptoms during the post infection stage among the age group of 30 years and above compared to the age group of below 30 years (Table 2). However, stratified analysis showed that there was no statistically significant association between age categories and post infection symptoms except for the loss of appetite which was more frequent (n=62, 36.25%) in the age group 30 and above compared to the age group below 30 years (n=15,21.12%) among the females (P=0.023). The incidence of fatigue was significantly higher among the females than males (Table 2).However, stratified analysis showed that there was no statistically significant association between sex and fatigue across the age categories. Of the 473 patients, 96 (20.29%) had not complained about any post infection symptoms. At least one post-infection symptom appeared for 74.73% (n=136) of patients among the age group below 30 years, the figure was significantly higher (n=239,82.70%) among the age group 30 years and above (P=0.036) (Table 2). However stratified analysis showed that there was no association between age and presence of at least one symptom across the sex categories and sex and the presence of at least one symptom across the age groups.
3.2. Preventive methods adopted for dengue infection
The most common preventive methods of transmission of dengue were reported as adding sand to places where water accumulates(41.65%) and drainage of stagnant water regularly (36.15%) (Table 3). Use of mosquito nets (83.09%) was the most common method of prevention of mosquito bites. A majority (56.03%) of patients reported that they use the wind generated by the electric fans to keep mosquitoes away from indoors without killing them.
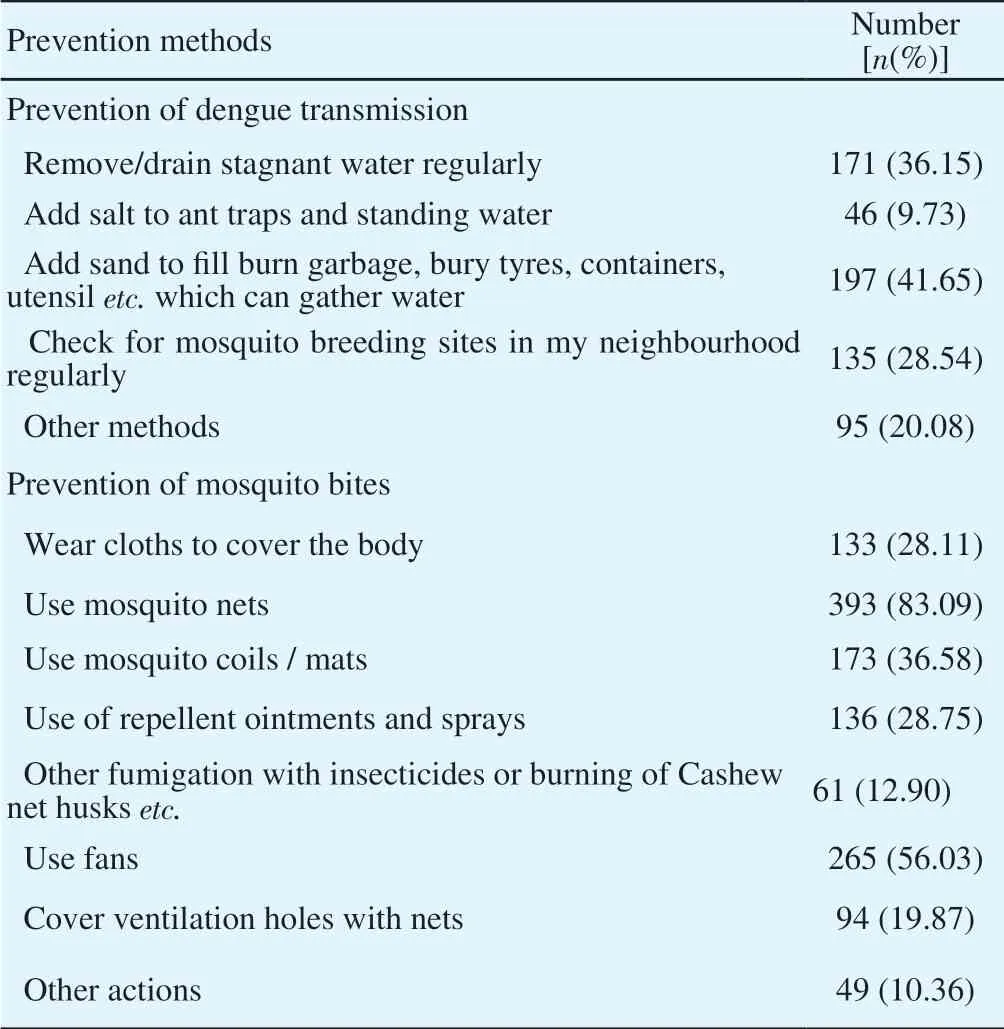
Table 3. Methods adapted to prevent dengue infection (n=473).
4. Discussion
The most common symptoms of dengue fever were body ache(81.81%), followed by headache (71.67%). These results match some of the previous studies which reported that myalgia/arthralgia(64%) was the common symptom followed by headache (59%)[7,8].Another study also reported that the most common symptom was headache (53.6%) at the acute stage of dengue fever[9]. In Sri Lanka,studies were scarce on the prevalence of post-infection symptoms and their longevity. A study conducted in Singapore reported that increased age, female sex, the presence of chills, and the absence of rashes were significantly associated with the development of fatigue post-dengue infection[10]. We could not find any significant association between age, sex, and persistence of post infection symptoms. It was suggested that the presence of persistent symptoms is associated with alterations in some immunological parameters and FcγRIIa gene polymorphism which may be autoimmune based[11].
According to our study, the median duration of hospital stay was 5 d. One study reported that the mean duration of hospitalisation in children with dengue fever and dengue haemorrhagic fever was 4.1 d and 4.8 d respectively[9]. A study in Taiwan reported that only 3.7% of dengue patients were admitted to an ICU[7]. According to our study, a higher percentage of patients (9.72%) were admitted to the ICU which requires more human and financial resources for management of such patients. According to a review conducted in 2016, if persistent symptoms affect a non-negligible share of the population, previous studies have likely underestimated the burden of dengue[6].
Recall bias is a possible limitation that was present when obtaining information. To minimize this, the information was collected from patients who had been confirmed to have had dengue during the past six month's period. Even then the recall bias was unavoidable.The response rate was lower than expected. Therefore we had to invite more patients for the study. It may affect the generalizability of the results. Even though we expected to assess the duration of the symptoms during the post infection stage, it was not possible to achieve it due to the lower response rate of this item. Furthermore,the study population was restricted to adults. Therefore, a comparison of post-infection symptoms with the paediatric population was impossible. We recommend a prospective study to assess post-infection burden of the disease including the economic burden to the patient's family.
In conclusion, persistent clinical symptoms during post-infection period is evident. The most common preventive methods of transmission of dengue were adding sand to the water collecting places and regular drainage of stagnant water. Use of mosquito nets was the most common method of prevention of mosquito bites.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Acknowledgments
We acknowledge the generous financial contribution by the Government of Canada and implementation support by the United Nations Migration Agency (IOM). We would also like to thank all the participants for the study, the data collectors and authorities of the Ministry of Health Sri Lanka.
Foundation project
Funding support was provided by the Government of Canada and the study was implemented with the technical and logistical support by the United Nations Migration Agency.
 Asian Pacific Journal of Tropical Medicine2019年6期
Asian Pacific Journal of Tropical Medicine2019年6期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Epidemiology and immunodiagnostics of Strongyloides stercoralis infections among migrant workers in Malaysia
- Anticancer activity of Mahonia leschenaultii methanolic root extract and berberine on Dalton’s ascitic lymphoma in mice
- Optimized combinations of statins and azoles against Acanthamoeba trophozoites and cysts in vitro
- Community-acquired pneumonia with Acinetobacter radioresistens bacteremia in an immunocompetent host: A case report
- Laboratory diagnosis of schistosomiasis mansoni: Current status and future trends
