62例急性白血病流式细胞仪免疫分型的特点及预后分析
陈瑛 陈海娟 王萍
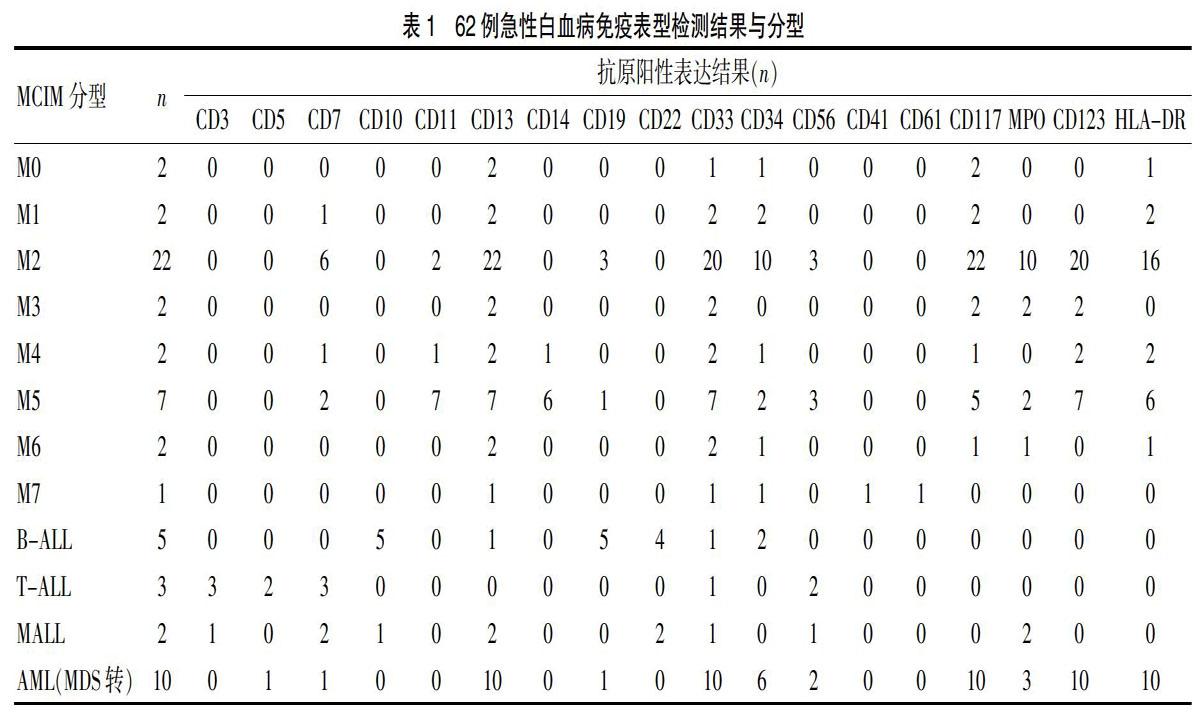
[摘要] 目的 探討流式细胞仪免疫分型在急性白血病(AL)患者中的表达特点、诊断价值及其预后意义,为建立个体化的治疗提供指导。 方法 回顾性对我院收治的62例初发AL患者的骨髓细胞形态学、流式细胞仪免疫分型检测结果进行对比分析,了解二者诊断相符率。结合细胞遗传学及分子生物学检查结果进行预后分析,之后分组观察患者治疗反应及生存情况。 结果 5例急性白血病患者通过骨髓细胞形态学和组织化学检查未能明确分型诊断,经流式细胞仪免疫分型检测后确定。2例骨髓细胞形态与流式细胞仪免疫分型结果不符,结合细胞遗传学特点,予以修正诊断。AML及ALL均存在跨系表达抗原,AML常见的跨系抗原表达为CD56、CD7、CD19。ALL常见跨系抗原表达为CD13、CD15、CD33。部分分子遗传学异常可对应有异常抗原表达,AML中CD7表达常伴有FLT3/ITD突变。AML伴t(8;21)(q22;q22)/AML1-ETO阳性患者中,60%左右表达CD19。在疗效观察中发现伴有预后不良染色体核型或分子遗传学标志的老年性急性髄系白血病患者(年龄≥70岁)中,非化疗组总生存期(OS)与化疗组相比无差异性(P>0.05)。 结论 流式细胞仪免疫分型检测可以提高急性白血病分型诊断的准确性,结合细胞遗传学和分子生物学可有效地指导临床制定治疗方案和预后判断。
[关键词] 急性白血病;流式细胞术;免疫表型;预后分析
[Abstract] Objective To investigate the expression characteristics, diagnostic value and prognostic significance of flow cytometry immunophenotyping in patients with acute leukemia(AL), and to provide guidance for the establishment of individualized treatment. Methods The bone marrow morphological and flow cytometry immunophenotyping results of 62 patients with initial AL admitted in our hospital were retrospectively analyzed to understand the diagnostic coincidence rate. The prognostic analysis was performed by combining the results of cytogenetics with molecular biology examination. And then the treatment response and survival of the patients were observed in groups. Results Five patients with acute leukemia were not diagnosed by bone marrow cell morphology and histochemical examination, and were identified by flow cytometry immunophenotyping. The morphology of 2 cases bone marrow cells was inconsistent with the results of flow cytometry immunophenotyping, and combined with cytogenetic characteristics, the diagnosis was corrected. Both AML and ALL had cross-line expression antigens, and common cross-line antigens of AML expressed were CD56, CD7 and CD19. The common cross-line antigens ALL expressed were CD13, CD15, CD33. Some molecular genetic abnormalities may correspond to abnormal antigen expression, and CD7 expression in AML was often accompanied by FLT3/ITD mutation. In AML patients with t(8;21)(q22;q22)/AML1-ETO positive, about 60% expressed CD19. In the efficacy observation, it was found that there was no significant difference in overall survival (OS) between the non-chemotherapy group and the chemotherapy group in the elderly patients with acute sputum leukemia (age≥70 years) with poor prognosis karyotype or molecular genetic markers(P>0.05). Conclusion Flow cytometry immunophenotyping can improve the accuracy of acute leukemia typing diagnosis, which can effectively guide clinical planning and prognosis combined with cytogenetics and molecular biology.