Reanalysis of Lymph node metastasis as predictor of the survival of patients with follicular variant papillary thyroid carcinoma: From SEER database 2004-2014
Jin Yang, Qing-Qing Liu, Hai-Rong He, Hai-Sheng You, Zhen-Yu Pan, Jun Lyu,2,5
1Clinical Research Center, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, Shaanxi, 710049,China;
2School of Public Health, Xi'an Jiaotong University Health Science Center, Xi'an, Shaanxi, 700049, China.
3Department of Pharmacy, The First Affiliated Hospital, Xi'an Jiaotong University, Xi'an, Shaanxi, 710049,China.
4Department of Pharmacy, The Affiliated Children Hospital of Xi'an Jiaotong University, Xi'an, Shaanxi,710049, China.
5Institute of Evidence-Based Medicine and Knowledge Translation, Henan University, Kaifeng,475001, China.
Abstract Background: Follicular variant papillary thyroid carcinoma (FVPTC) is the most common subset of papillary carcinoma. Lymph-node metastasis (LNM) is one of the main predictors of survival in PTC patients, but we found few data related to the correlation between LNM and FVPTC. We therefore aimed to elucidate the relationship between LNM and survival in patients with FVPTC.Methods: Logistic regression models were used to determine the factors associated with LNM. The Cox proportional-hazards model was applied to assess the association between LNM and disease-specific mortality. Kaplan-Meier survival analysis and the log-rank test were used to estimate the disease-specific survival rates in patients with and without LNM.Results: In total, 1418 FVPTC patients were identified. The multivariate logistic regression model showed that age, female sex, being married, tumor size > 4cm and extrathyroidal extension and radiation were predictors of LNM. The multivariate Cox regression model showed that age, multifocality and radiation were risk factors of diseasespecific mortality. Especially, LNM (p=0.271) did not independently predict disease-specific mortality. Kaplan-Meier survival analysis and the log-rank method also showed that LNM did not impact survival in FVPTC (p=0.235).Conclusion: Using data in the SEER database from 2004 to 2014, and after multivariate model correction, we found that age, multifocality and radiation were strongly related to disease-specific mortality. It is worth noting that LNM does not impact the survival of FVPTC patients.
Keywords: LNM; Risk factors; Survival; FVPTC patients; SEER database
Introduction
The incidence of thyroid cancer has tripled since 1975[1], and this is mainly due to papillary thyroid carcinoma(PTC) [ 2,3], which accounts for 80-90% of all thyroid malignancies [4]. Classical papillary thyroid carcinoma and follicular variant papillary thyroid carcinoma(FVPTC) are the two most common papillary thyroid cancers. FVPTC is the most common subset of papillary carcinoma, reportedly accounting for 9-33% of patients with PTC [1,5-7]. It is characterized by a follicular architecture with nuclear features of papillary carcinoma,and the nuclear features can be subtle with instances of it being mistaken for follicular adenoma [8]. It has been found that FVPTC accounts for up to 41% of PTC cases[9]. Despite the high incidence, the clinical behavior and outcomes of FVPTC remain controversial [9].
Lymph-node metastasis (LNM) occurs in 20-50%of patients presenting for initial treatment of papillary thyroid cancer [9,10]. The regional lymph nodes to which thyroid carcinoma can metastasize are classified into three regions: central, lateral, and mediastinal compartments.It has been shown that central LNM is valuable for predicting lateral-compartment involvement in patients with PTC [11]. The primary treatment for LNM is surgical resection [12,13]. LNM occurs frequently in PTC and is associated with a poor prognosis [14]. Prophylactic lymph-node dissection is still controversial in the management of PTC due to the potential for surgeryrelated morbidity [15]. Such dissection is one of the main predictors of the survival rate of PTC patients. However,we found few data on the correlation between LNM and FVPTC.
The Surveillance, Epidemiology, and End Results(SEER) program of the National Cancer Institute (NCI)is the largest publicly available source for data on cancer incidence and survival in the United States [16,17]. The SEER database is commonly used as a data source in cancer research [18], with it recording information on the morbidity and mortality of millions of patients diagnosed with many types of cancer and followed up over long time periods.
The purpose of this study was to determine whether LNM affects the survival of patients with FVPTC and the association between LNM and FVPTC patients. .
1 Materials and methods
1.1 Study design and participants
This retrospective study was performed using data from the SEER database maintained by the NCI. The SEER*Stat analysis program was downloaded from(www.seer.cancer.gov) and used to query the SEER database in order to identify patients older than 18 years with histologically confirmed FVPTC diagnosed from 2004 to 2014. The FVPTC screening used the ICD-O-3(Third Edition of the International Classification of Disease for Oncology) with a code of 8340. Cases without surgery or a diagnosis or only with an autopsy were excluded. LNM was defined as group N. We used the Sixth Edition of the American Joint Committee on Cancer Staging Manual to describe the TNM staging.
The SEER database contains the records of more than 95,000 thyroid cancer patients. The application of our selection criteria identified 24,695 FVPTC patients and 23,277 patients who did not meet the screening criteria
Funding:This study was supported by the National Social Science Foundation of China(No.16BGL183),the Natural Science Foundation of Shaanxi Province (No.2015JM8415),the Fundamental Research Funds for the Central Universities of China (No.2011jdhz55),the Clinical Research Award of the First Affiliated Hospital of Xi'an Jiaotong University of China (No.XJTU1AF-CRF-2016-021), and the Research Fund of Health Bureau of Xi'an (No.QFO1330).
Competing interests:The authors report no conflicts of interest in this work.
Copyright:©2018 TMR Publishing Group Limited. This is an open access article distributed under the terms of the Creative Commons Attribution Non Commercial License.
Submitted:22 January 2019. Accepted: 22 January 2019. Online: 25 January 2019.
(who were rejected) (Figure 1).
1.2 Statistical analysis
We constructed a univariate logistic regression model to identify significant variables, then used a multivariate logistic regression model to determine the factors that were associated with LNM. Meanwhile, the Cox proportional-hazards model was applied to assess the association between LNM and disease-specific mortality.Hazard ratios (HRs) with 95% confidence intervals (CIs)were used to quantify the strength of the association between LNM and disease-specific mortality. Kaplan-Meier survival analysis was used to estimate the diseasespecific survival rates for patients with and without LNM. The log-rank test assessed statistical differences between survival curves. While the SEER database is publically available, it is of utmost importance to protect the identities of cancer patients. All of the authors signed the “SEER Research Data Agreement” in order to protect the patients' privacy, which is consistent with ethical principles.
All analyses were performed using Rsoftware and SPSS(version 24.0). All tests were two-sided, and statistical significance was defined as a probability value of p<0.05.
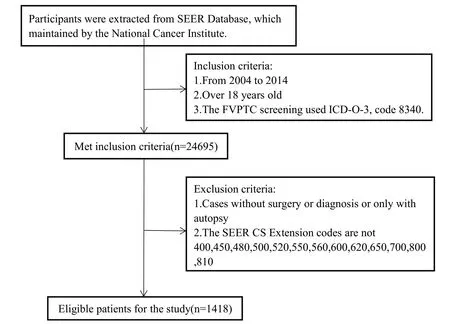
Figure 1. Flow diagram for the selection of patients.
2 Results
2.1 Patient characteristics
The demographic characteristics and tumor features of the FVPTC patients as well as the treatments they received are presented in Table 1. The average age was 49.46 years old. There were 362 male patients (25.53%),as well as 223 single patients (15.73% of the total).Among racial groups, white patients accounted for 80.04% of the total (n=1135). Tumor size was divided into three categories: ≤2 cm, >2 cm and ≤4 cm, and>4 cm. Those with tumor size ≤2 cm accounted for 49.9% of the patients (n=707), 442 patients had a tumor size of >2 cm and ≤4 cm (31.2%), and 245 patients had tumors larger than 4 cm (17.3%). There were 741 patients with LNM (52.26%). Multifocality was present in 1368 patients (97.74%), and 1028 patients received radiation therapy (72.50%). There were 72 deaths, giving a final number of survivors of 1346. The overall survival period was 48.01±33.90 months (Table 1).

Table1. Patient characteristics
2.2 Factors related to LNM
We used univariate logistic regression and multivariate logistic regression to analyze the relationships between various factors and LNM; the results are presented in Tables 2. Further multivariate logistic regression analysis showed that age (OR=0.978, 95% CI=0.970-0.986,p<0.05), female sex (OR=0.493, 95% CI=0.374-0.649,p<0.05), being married (OR=0.715, 95% CI=0.519-0.986,p<0.05), radiation (OR=0.754, 95% CI=0.583-0.977,p<0.05), tumor size >4cm (OR=1.672, 95% CI=1.179-2.372, p<0.05) and extrathyroidal extension (OR=5.640,95% CI=4.305-7.389, p<0.05) were predictors of LNM.
2.3 Factors related to disease-specific mortality
We used both univariate and multivariate Cox regression to analyze the relationship between LNM and diseasespecific mortality; the results are presented in Tables
3. Further multivariate Cox regression analysis showed
that age (HR=1.064, 95% CI=1.047-1.082, p<0.05),multifocality (HR=2.418, 95% CI=1.036-5.642, p<0.05),and radiation (HR=1.780, 95% CI=1.106-2.865, p<0.05)were significant risk factors for disease-specific mortality.Female sex (HR=0.513, 95% CI=0.401-0.657, p<0.05)was a protective factor for disease-specific mortality.Importantly, LNM did not independently predict diseasespecific mortality (p=0.271).
2.4 Survival analysis of patients with FVPTC
Thirty-seven of the 72 deaths were associated with LNM (51.39%), and the 5-year cumulative survival rate was 98.9%. Thirty-five of the patients did not have LNM(48.61%), and their 5-year cumulative survival rate was 99.8%. We further analyzed whether LNM affects the survival of patients with FVPTC by applying Kaplan-Meier survival analysis and the log-rank method. The results showed that LNM did not impact survival in FVPTC (p=0.235, Figure 2).
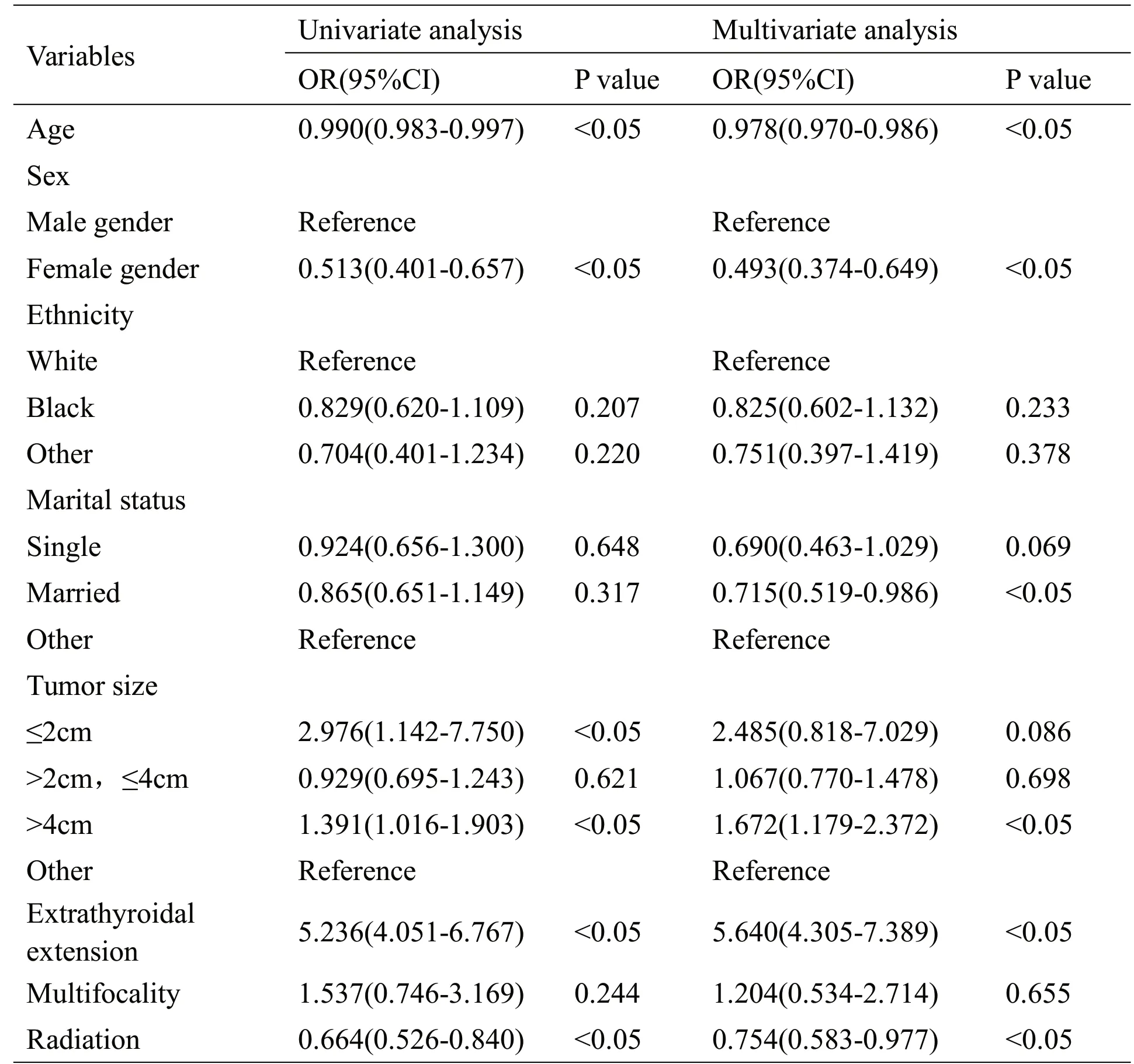
Table 2. Logistic regression analysis for factors related to LNM

Table 3.Cox regression analysis for factors related to disease-specific mortality
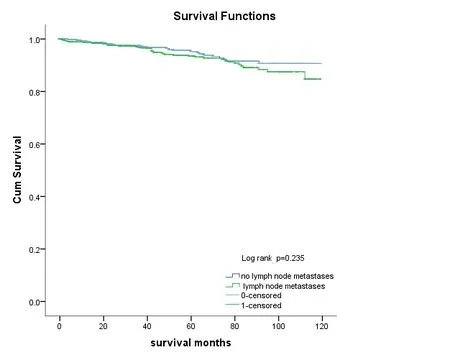
Figure 2. disease-specific survival for patients with and without LNM
3 Discussion
FVPTC is a common variant of papillary carcinoma whose incidence is increasing. This cancer typically favors nodal spread [19]. Nonetheless, lymph node metastasis were observed in some FVPTC patients [20]. Since LNM is a proven predictor of recurrence in PTC, it is important to assess LNM metastasis in FVPTC patients.However, we found few data related to the correlation between LNM and FVPTC. Our review of the literature revealed only a few studies of the relationship between LNM and FVPTC, and only one involving data coming from the SEER database [6]. We therefore wanted to elucidate the relationship between LNM and FVPTC based on recent data from the SEER database.
In this study, we included 1,418 cases obtained from the SEER database from 2004-2014. Further multivariate logistic regression analysis showed that age, female sex,being married, radiation, tumor size >4cm and extrathyroidal extension, were predictors of LNM.Age was a protective factor for LNM, which may be related to the relatively high degree of malignancy of thyroid cancer with a low age of onset. Radiotherapy was also a protective factor for LNM, suggesting that radiotherapy had an important role in reducing the probability of LNM. In addition, women and married were also protective factors for LNM. However, tumor size >4cm and extrathyroidal extension were risk factors for LNM, especially extrathyroidal extension was a strongest predictor. The results suggested that FVPTC patients with tumors >4cm and extrathyroidal extension should pay attention to the thoroughness of lymph node dissection. Understanding these factors associated with LNM helped us to further analyze the relationship between LNM and disease-specific mortality.
Further multivariate Cox regression analysis showed that age, multifocality, and radiation were significant risk factors for disease-specific mortality. The results suggested that the risk of death increases in older FVPTC patients. To strengthen the early diagnosis and treatment of thyroid cancer patients is the key to ensure the safety of patients. Although radiation therapy can reduce the probability of lymph node metastasis and eradicate normal-thyroid remnants, it may also induce other symptoms, such as lacrimal and salivary gland toxicities [16]. Female sex was a protective factor for disease-specific mortality. However, LNM still did not independently predict disease-specific mortality in the multivariate analysis.
To make the result more conservative, We further used Kaplan-Meier survival analysis and the log-rank method to determine that whether LNM could affect the survival of patients with FVPTC. The results were same:LNM did not impact survival in FVPTC (log-rank test:p=0.235, Figure 2).
We reached the same conclusion that LNM did not impact disease-specific mortality. The use of new methods and updates of data make our conclusions more accurate. We used Kaplan-Meier survival analysis and the log-rank method—which they did not use—to further support our conclusions. Although the rate of diseasespecific deaths was slightly higher in patients with LNM,this seems to be a risk factor for survival in FVPTC.However, we found that the two curves crossed in the Kaplan-Meier survival analysis and that p>0.05 in the log-rank test, which further support our conclusions.
This study was subject to some limitations. The SEER database contains some flaws, with many of its indicators containing missing data, an absence of subtle clinical indicators and molecular markers, and no patient recurrence records, all of which may be crucial to this type of research. For example, genomics are considered to prevent disease and improve health care [21]. The presence of the BRAF mutation has been shown to be an independent predictive factor for central LNM [22],while the SEER database does not include information on BRAF. Since the data fields in SEER are incomplete,most patients who do not meet the conditions were rejected. Therefore, our conclusions need further analysis. Although case completeness is superior in fields covered by the SEER database, patients included in the SEER database exhibit greater economic disadvantage and greater minority diversity compared to the general population [23], this restricts the generalizability of the conclusions drawn in the present study. In addition,whether radiotherapy contributes to improving survival rates needs to be discussed. Finally, since the present study had a retrospective design, the obtained data were not controlled by the researchers and so some of it might not have been consistent with the inclusion criteria. The conclusions of a retrospective study can only provide clues about the related diseases but cannot confirm the causal link between LNM and disease-specific mortality.
4 Conclusions
We reassessed the association between LNM and the survival of patients with FVPTC. Using data in the SEER database from 2004 to 2014, and after multivariate model correction, we found that age, multifocality and radiation were related to disease-specific mortality. In this study,LNM did not impact the survival of FVPTC patients.Despite the shortcomings of the SEER database, it still provides good data for use in research. Perhaps these data could be helpful when designing future clinical trials.
- Medical Data Mining的其它文章
- Efficacy and safety of atomized inhalation for Shuanghuanglian on chronic pharyngitis:a Meta-analysis of the randomized controlled trials
- Heating infusion for gastrointestinal complications in patients with enteral nutrition: A meta-analysis
- Literature Research on Drug Use Regulation of Miao Medicine in Suppression of Gastric Cancer
- Clinical Medicine Characteristics Study of Traditional Chinese Medicine in the treatment of cancer pain based on Data Mining