Vertebral Artery Dissection Probably Caused by Massage: A Case Report
Weijian Chen, Hongyu Qiao, Guiting Fang, Xing Zhong*
1Medical Imaging Center, 2Department of Neurology, The First Affiliated Hospital of Jinan University, Guangzhou 510630, China
Key words: vertebral artery dissection; spinal cord infarction; chiropractic
Abstract MASSAGE has been recommended to more people as an adjunct to health care. We illustrate a case of vertebral artery dissection (VAD) probably caused by massage that almost resulted in the patient’s death. The patient experienced sudden cardiac arrest and paralysis. After treatment with anticoagulation and antiplatelet, he finally discharged without any sequelae.
M ASSAGE has been recommended to more people as an adjunct to health care. Although massage has advantages, it might also be hazardous.[1]This report illustrates a case of a patient with vertebral artery dissection (VAD) and spinal cord infarction (SCI) maybe due to massage. Because the diagnoses of VAD and SCI were missed during the first visit, the patient almost died.
CASE DESCRIPTION
On December 4, 2015, a 48-year-old man with hypertension had dizziness accompanied by neck pain after a recent massage, and he was immediately brought to the emergency room of a local hospital. His vital signs were within normal limits, except for hypertension (150/120 mm Hg, 1 mm Hg = 0.133 kpa). After abrupt antihypertensive therapy was provided, his symptoms were subsequently relieved. The patient was discharged home, but he felt dizzy again after 3 hours.progressive numbness and dyspnea occurred when the man reached the hospital again, which led to sudden cardiac arrest; however, normal heart rate reoccurred after performing cardiopulmonary resuscitation. Brain computed tomography (CT) revealed no abnormal findings. He was admitted to our hospital for further treatment on the same day. On neurological examination,both his limbs were weak (Medical Research Council Scale for muscle strength: left 0/5, right 1/5), and sensory examination showed symmetrical decrease in superficial sensation below the neck. Digital subtraction angiography (DSA) revealed dissection of the left vertebral artery (VA), blood sluggishness, and serious stenosis at the V2 level (Figure 1A).
We treated him conservatively as per the patient’s family’s decision. DSA-guided local injection of 10 ml tirofiban hydrochloride (5 mg/100 ml, Grand pharmaceutical Co., Ltd, China) was performed,then intravenous tirofiban hydrochloride (13 ml/h)and enoxaparin sodium (Sanofi, China) were administered. Three days after admission, DSA revealed that the stenosis had been relieved (about 50%),and blood flow velocity increased (Figure 1B). CT angiography (CTA) on axial images showed double lumen sign (Figure 2A), and the diagnosis of VAD was reconfirmed. MRI showed that the cervical cord was swollen, with patches of high signal intensity on T2-weighted image between the C1 and C4 vertebral bodies (Figure 1C). Clopidogrel sulfate was administered as maintenance medication. On the fourteenth day of admission, tirofiban hydrochloride and enoxaparin sodium were discontinued, and oral aspirin was administered instead. Thirty-three days after onset of stroke, MRI showed syringomyelia in the spinal cord(Figure 1D); however, reduction of the lesion range was also observed. No positive signs were found on vertebral ultrasonography. The patient was discharged from our hospital without any sequelae. CTA was performed 6 months after discharged, and showed a smooth VA (Figure 2B).
DISCUSSION
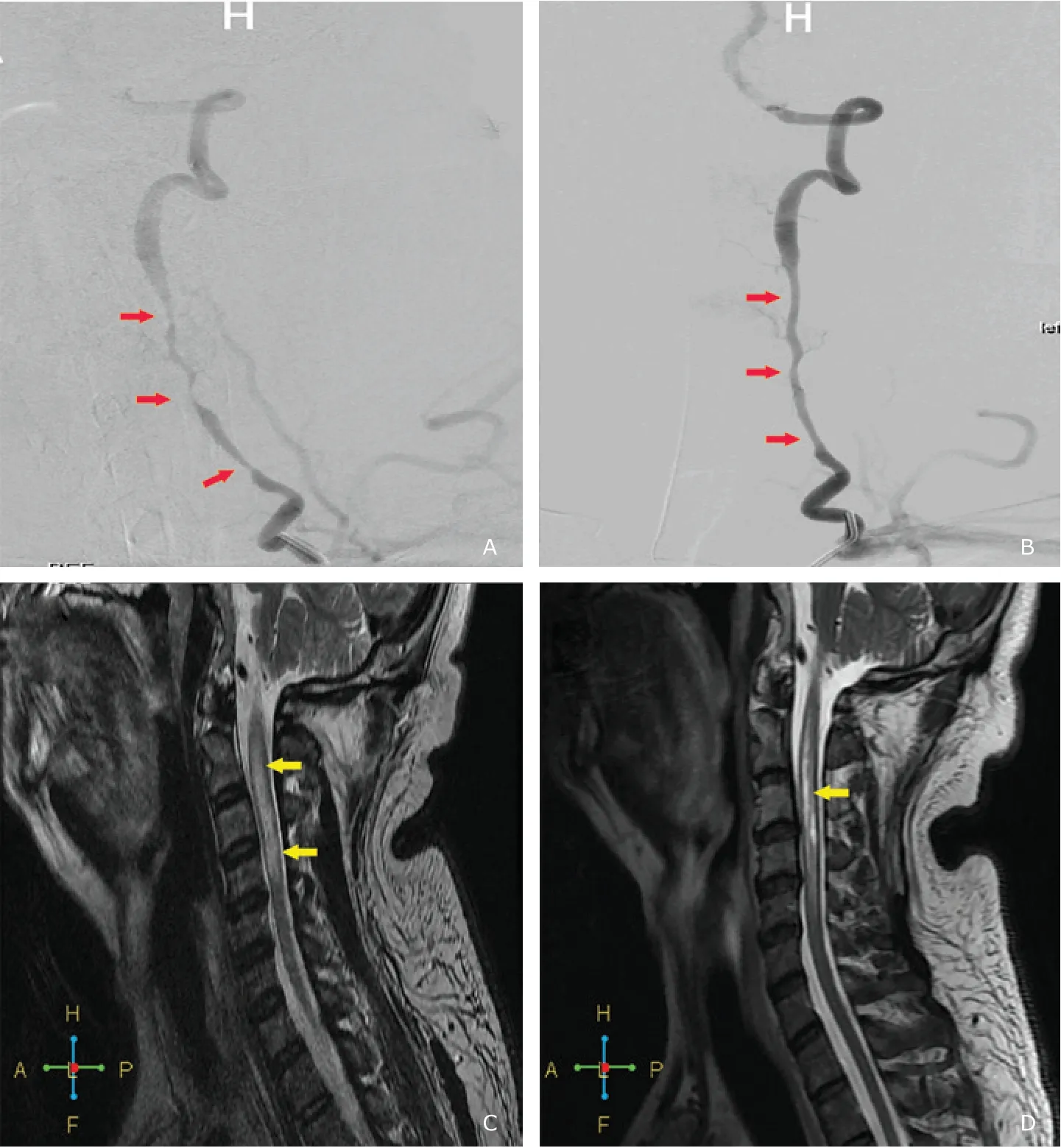
Figure 1. A. Emergency digital subtraction angiography (DSA) showed serious and irregular narrowing of the left vertebral artery (red arrows). B. DSA at three days after admission showed stenosis was relieved (red arrows). C. T2-weighted MRI of the cervical spine cord showed patches of high signal intensity between the C1 and C4 vertebral bodies (yellow arrows).D. T2-weighted MRI, performed at 33 days after stroke onset, showed syringomyelia in the cervical cord (yellow arrow).

Figure 2. A. Dual lumen sign (blue arrows) was shown on arterial phase image of CT angiography (CTA), and a zoomed image was provided on lower left corner of the picture. B. CTA of half a year after the patient was discharged showed a smooth vertebral artery.
VAD, which is rarely encountered in clinical practice, however is the main cause of stroke in young adults. Owing to its anatomical features, stroke of spinal cord seldom occurs, only accounting for < 1%of all cases of stroke, compared with cerebral stroke.The upper cervical cord (C1-C3) was supplied by the intracranial VA. The main branches of intracranial segment (V4 segment) including the posterior inferior cerebellar, anterior spinal, and posterior spinal arteries are very slender, which make the brain regions,such as cerebellum and brainstem, fed by them to take place infarct easily. On the contrary, the cervical cord supplied by V2 segment that is enveloped by periosteum covering the surface of transverse foramen and the surrounding cervical vertebras as well is not susceptible to cerebral infarction generally. In addition, movements of cervical spine depending on the shape of the joints and the direction of the articular surfaces can increase risks of vascular injuries of VA.[2]Rotation and extension of the neck can make the elastic pull of VA, thereby causing VA nestling up against vertebra and increasing the tension of the blood vessel wall. Biller et al.[3]found pathological changes of vascular injuries caused by bony spur and hyperplasia of superior articular surface around transverse foramen.
For the reason that the muscular branch of extracranial VA is anastomosed with cervicalis profunda,ascending cervical artery, and external carotid artery,unilateral injury of extracranial VA is not sufficient to give rise to ischemia in the territory of this branch theoretically. However, infarction caused by VAD occurs in clinical practice, and this phenomenon is probably attributed to the abrupt interruption of blood supply, and the collateral circulation cannot compensate completely. Short-term ischemia may cause diplopia, coma, or even cardiac arrest, and prolonged ischemia may lead to infarction. Therefore, the emergency operation was performed immediately after the patient arrived at our hospital, because CTA and MR are time-consuming, and the inspection cannot be carried out in time. Yet there were about 3 hours from first visit to sudden cardiac arrest, and more than 20 hours from sudden cardiac arrest to interventional therapy. Finally, We found spinal cord infarction on postoperative MR examination.
There are no specific symptoms of patients with spinal cord stroke, who may present with headache,neck pain, dizziness, or senso-motor deficits.[4]In this case, the patient’s initial manifestation was neck pain and dizziness, and the emergency physician missed VAD due to the presence of hypertension. Most cases of VAD are spontaneous. Hereditary connective tissue disorders are considered as well-characterized risk factors for spontaneous artery dissections, besides other potential factors, such as age, hyperhomocysteinemia, current infection, and diabetes mellitus.[5]A fraction of VAD is caused by violence, such as various types of sports,[6-7]history of twisting the neck, and chiropractic treatment,[8]which is the most frequently discussed risk factor for cerebral artery dissection.There is on evidence to verify VAD already existed before massage in this subject. Young male patients usually present with more severe spinal cord strokes in the initial phase. Dramatically, men tend to improve more rapidly than women.[9]As previously mentioned,the patient experienced a life-threatening situation;however, after neurotrophic, anticoagulation, and antiplatelet therapies, he survived well without any functional deficits.
In conclusion, we hope to draw the physician’s attention to this rare disease. Diagnosis of VAD should be considered in young adults presenting with headache, neck pain, and dizziness, so as to avoid death due to missed diagnosis.
Conflict of interest statement
The authors have no conflict of interest to disclose.
 Chinese Medical Sciences Journal2019年1期
Chinese Medical Sciences Journal2019年1期
- Chinese Medical Sciences Journal的其它文章
- Successful Treatment of Severe Heparin-induced Thrombocytopenia with Intravenous Immunoglobulin, Platelet Transfusion and Rivaroxaban: A Case Report
- Bilateral Peripheral Facial Paralysis Combined with HIV Meningitis During Acute HIV-1 Infection: A Case Report
- Prediction of Hidden Blood Loss During Posterior Spinal Surgery
- Value of Magnetic Resonance Imaging Texture Analysis in the Differential Diagnosis of Benign and Malignant Breast Tumors
- Value of Texture Analysis on Gadoxetic Acid-enhanced MR for Detecting Liver Fibrosis in a Rat Model
- MRI Histogram Texture Feature Analysis of the Optic Nerve in the Patients with Optic Neuritis
